Diphtheria is a serious infectious disease known to people for many centuries. Previously, it was called strangulation loop, malignant tonsillitis, Sicilian ulcer, strangulation disease, diphtheria, and so on.
Galen, Hippocrates and many other ancient doctors mentioned diphtheria in their works. But it would be a mistake to believe that diphtheria is a thing of the distant past and no longer threatens modern children.
Of course, the incidence has decreased hundreds and thousands of times, and deaths from diphtheria have become rare, but the likelihood of becoming infected remains to this day.
Diphtheria is an acute infectious and inflammatory disease caused by corynebacteria. Pathogens affect the mucous membranes, primarily the oropharynx, less often the larynx, nasal mucosa, eyes, ear canals, and genitals.
The main danger of this bacterium is the toxins it produces. They spread through the bloodstream throughout the body, damaging organs and tissues, primarily the nervous system, heart muscle and kidneys. In addition, diphtheria provokes severe inflammation of the larynx (croup), blockage of the airways with films, spasm and swelling.
It is acute respiratory failure in combination with general intoxication of the body that leads to death.
Diphtheria can affect people of any age, but it is most dangerous for children. Before the invention of the vaccine and antitoxin, the mortality rate reached 50%. But even today, with the availability of modern methods of therapy, the probability of death remains in 5–10% of cases.
How can you become infected with diphtheria?
The main route of transmission of this disease is airborne droplets. Most often, infection occurs indoors, in groups, especially children's.
In addition, other transmission mechanisms are possible: through objects, for example, books, cutlery, toys. Outside the human body, the pathogen does not retain its activity for long, so this route is more rare. In some cases, mass infection was recorded through food, especially dairy products, where bacteria can actively multiply.
The source of infection is always a person with diphtheria or an asymptomatic carrier. The more severe the disease, the more pathogens a person releases into the environment.
How can diphtheria occur?
Diphtheria pathogens can settle on the mucous membrane, as well as on damaged skin. Therefore, there are several primary localizations:
- Oropharynx. This is a typical option, which is recorded in 90–95% of all cases. The palatine tonsils are the first to be affected, so at an early stage the disease looks like tonsillitis or tonsillitis. Such diphtheria can be catarrhal, when only the tonsils are inflamed, or widespread, involving the palatine arches, palate, larynx, and so on. Following diphtheria of the oropharynx, secondary inflammatory processes may begin.
- Nose. Inflammation of the nasal mucosa can be either a primary form or a complication of oropharyngeal diphtheria. With this form, a runny nose begins, there may be plaque and diphtheria films on the nasal mucosa, and weeping areas appear on the skin. General symptoms rarely appear.
- Eyes. Most often it manifests itself as conjunctivitis, the appearance of diphtheria films on the mucous membrane, and swelling of the eyelids is possible. This form also rarely provokes the appearance of general intoxication.
- Ears. In most cases, ear diphtheria is a complication of another form of the disease. Damage to the inner ear is possible when pathogens spread through the Eustachian tube, or to the external ear when carried by hands or objects. Signs of this form are pain in the ear, discharge from the ear canal. Upon examination, diphtheria films, weeping plaque, and signs of inflammation are found in it.
- Genital organs. A rare form, most often it is a complication. The mucous membranes are inflamed and films appear on them.
- Wounds. It can develop if a pathogen gets into a wound or scratch. There are signs of local inflammation around the wound; there may be films. Such skin damage heals slowly.
Regardless of the primary localization, diphtheria can occur in different ways:
- Asymptomatic carriage. Laboratory diagnostics reveals the presence of pathogens on the affected mucosa, but there are no symptoms of the disease. Carriage can last up to several months.
- Catarrhal diphtheria. The inflammation is local, there are no signs of intoxication. The disease is mild and does not cause general symptoms or complications. Like carriage, it is typical for people who have been vaccinated.
- Subtoxic. There may be signs of general intoxication, such as fever, headache and general malaise, but there are no complications.
- Toxic. Develops in unvaccinated people. It is difficult to tolerate; on the 2nd–3rd day of the course, general symptoms appear: high fever, headaches, malaise, shortness of breath. Without treatment, complications develop: damage to the nervous, respiratory, and cardiovascular systems.
- Hypertoxic. It is characterized by a lightning-fast, severe course. Death is possible already on the second day.
In most cases, toxic diphtheria of the oropharynx occurs. Therefore, it is its symptoms that you should focus on first.
Diphtheria: clinical course, diagnosis and treatment
Diftheria is an acute infectious disease caused by toxigenic corynebacteria diphtheria, transmitted by airborne droplets, characterized by local fibrinous inflammation of predominantly the mucous membranes of the oropharynx and nasopharynx, as well as symptoms of general intoxication and damage to internal organs.
Etiology
The causative agent of diphtheria, Corynebacterium diphtheriae, was discovered by Klebs in 1883 in sections of diphtheria films, and in 1884 Leffler isolated it in pure culture. According to the modern classification of bacteria, the genus Corynebacterium includes several species that cause disease in humans. The species C. diphtheriae is heterogeneous in cultural, morphological and enzymatic properties, and therefore three biovars are distinguished: gravis, mitis and intermedius. Biovars received their name due to the supposed connection with the severity of the clinical course. The gravis type (short polymorphic rods that ferment starch) was isolated mainly in severe and complicated forms of diphtheria, accompanied by high mortality. The mitis type (long curved polymorphic rods that do not ferment starch) predominated in mild forms, and intermedius occupied an intermediate position. This dependence was confirmed during the current diphtheria epidemic in Russia. Diphtheria bacilli are straight or slightly curved, 1 - 8 microns long, 0.3 - 0.8 microns wide, polymorphic. Under a microscope you can see that they are better stained at the poles, where the presence of granules (inclusions) is noticeable. In smears, corynebacteria are located at an angle, taking on the appearance of “spread fingers.” The optimal growth temperature for C. diphtheriae is 37.0 °C. The causative agents of diphtheria are well cultivated on media containing protein. They are adversely affected by direct sunlight and high temperatures. When boiled, they die after 1 minute; disinfectants (bleach, 1% chloramine solution, Lysol, etc.) have a detrimental effect on them. When dried, they can be stored for up to 1 month. The main factor in the pathogenicity of corynebacteria is exotoxin. Exotoxin-producing pathogens are defined as toxigenic strains. There are corynebacteria that do not produce exotoxin (nontoxigenic strains) that do not cause disease. Diphtheria toxin was discovered in 1888. The molecular composition of the toxin was deciphered in the 60s and 70s of our century. Diphtheria toxin is a protein with a mol. weighing 62 - 63 kDa. During mild hydrolysis, it breaks down into two fragments - A and B. The antigenic composition of fragment A is heterogeneous. When administered to animals, it had no toxicity, and when administered to tissue culture, it had no cytotoxicity. The B fragment is a thermostable protein that determines the toxic effect. An analysis carried out using monoclonal antibodies to fragments A and B of the toxin showed that in humans, 80% of antibodies are formed to fragment A and only 20% to fragment B. In addition to the toxin, the rod has a number of cell wall antigens. The main ones are polysaccharides, peptilopolysaccharides, proteins and lipids. Surface antigens of the cell wall provoke a type-specific antibody response, while deep antigens provoke a species-specific response. A cord factor was found in the surface layers of the cell wall of the pathogen, which promotes the adhesion of corynebacteria. The presence of antitoxic antibodies in the blood serum of those who had diphtheria was established at the end of the last century.
Epidemiology
Diphtheria is an anthropogenic disease. The source of infection is a patient with diphtheria or a carrier of toxigenic strains of corynebacteria. The pathogen is isolated from patients with severe forms of the disease in greater quantities than from people who have had the disease mildly. However, from an epidemiological point of view, patients with mild and erased forms of diphtheria are more dangerous if the true nature of the disease is not recognized and the patients are not isolated in a timely manner. Bacteria carriers play a special role in the spread of the disease, although they excrete the pathogen quantitatively much less intensively than patients with manifest forms. The most dangerous are bacteria carriers that secrete microbes for a long time (up to 1 month or more), which is more often observed in patients with concomitant diseases of the upper respiratory tract and oropharynx. The mechanism of transmission of the pathogen is airborne (during talking, sneezing, coughing). The main route of transmission of the pathogen is airborne, as well as through household contact - through dishes, towels, toys, etc. There are known “dairy” outbreaks of diphtheria associated with infection through infected dairy products. The causative agent of diphtheria is stable in the external environment. In diphtheritic film it persists for 3 - 5 months, in dust - up to 2 months, on food - up to 12 - 18 days, in droplets of saliva remaining on the walls of a glass, on door handles, on children's toys, diphtheria bacteria can persist 15 days. The survival rate of corynebacteria on environmental objects in the autumn-spring period can reach 5.5 months, and all this time the pathogenic properties of the pathogen are preserved. The contagiousness index for diphtheria is 15 - 20%, i.e. When the pathogen circulates among the non-immunized population, 15-20% become ill with diphtheria. The most common outcome of infection is bacterial carriage. During an influenza epidemic, the circulation of toxigenic corynebacteria increases 7-15 times. The incidence of diphtheria is influenced by a number of factors, including the state of natural and artificial, i.e. vaccination, immunity. The infection is defeated if 70% of children under 2 years of age and 70% of adults are vaccinated. Socio-ecological factors also occupy a certain place.
Pathogenesis
The entrance gates are usually the mucous membranes of the oropharynx (microbes use mucus as a habitat), nose, larynx, less often the eyes, genitals, and skin. The pathogen is fixed at the site of penetration and multiplies there, releasing an exotoxin. During their life, corynebacteria also produce other biologically active substances: hyaluronidase, neuraminidase - necrotizing and diffusion factors. Pathological changes in the patient's body - intoxication, local inflammation, early and late complications - are caused by the damaging effect of the toxin, which consists in blocking protein synthesis by the cell. Under the influence of the toxin, membrane permeability increases. In this it is assisted by other bacterial flora present in the oropharynx. The consequence of local exposure to the toxin is coagulative superficial necrosis of the epithelium, resulting in increased penetration of toxic substances. Paralytic dilatation of blood vessels occurs with a sharp increase in the permeability of their walls and the sweating of exudate rich in fibrinogen. In the acute period of the disease, as a result of the inflammatory process, the concentration of fibrinogen in the blood increases. Fibrinogen, under the influence of thrombokinase, released from necrotic tissue, coagulates and turns into fibrin. This is how a fibrinous film is formed, which is the most characteristic sign of diphtheria. Those areas of integumentary tissue that have multilayered epithelium (oropharynx) are covered with a film that is difficult to remove. On single-layer epithelium (trachea, larynx), films are easily rejected. Regional lymph nodes are involved in the process; they enlarge due to sudden congestion, edema and proliferation of cellular, mainly reticuloendothelial, elements. In the immediate vicinity of the affected lymph nodes, swelling of the subcutaneous tissue of the neck occurs. This swelling is caused by serous inflammation with numerous cellular infiltrates, and the general toxic effect is due to the toxin entering the blood. Bacteremia is extremely rare and does not play a role in pathogenesis. Of great importance in the pathogenesis of toxic and hypertoxic forms is preliminary sensitization of the body as a result of diseases suffered shortly before diphtheria. Fixation of the toxin in tissues leads to characteristic damage to the nervous and cardiovascular systems. In the myocardium, parenchymal degeneration of muscle fibers occurs early, up to complete myolysis and clumpy disintegration. Characteristic is fatty degeneration with subsequent destruction of myofibrils and the formation of diffuse sclerosis. Changes in the peripheral nervous system occur as parenchymal neuritis with predominant damage to the myelin and Schwann sheaths without significant involvement of the axial cylinder. The severity of diphtheria and the outcome of the disease are significantly influenced by the level of antitoxic immunity in the patient, the degree of toxigenicity of the corynebacterium strain and the dose of the pathogen.
Clinical course
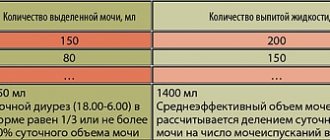
Depending on the location of the process, diphtheria is distinguished between the oropharynx, nose, larynx, trachea, bronchi, eyes, ears, genitals, and skin. In some cases, simultaneous damage to various organs occurs - combined diphtheria. Most often, the diphtheria process is localized in the oropharynx. The clinical forms of oropharyngeal diphtheria are extremely varied and depend on the nature and distribution of the fibrinous film, the degree of swelling of the mucous membrane of the oropharynx and subcutaneous tissue of the neck, and the severity of intoxication. Criteria for the severity of the process are the severity of symptoms of damage to the oropharynx and the amount of swelling of regional skin tissue. The more severe the disease, the earlier its characteristic symptoms appear and the more pronounced they are. Obviously, the criteria by which the severity of the disease is determined are subjective, conditional and depend on the time of onset and severity of symptoms and on the experience of the doctor. According to the existing classification of oropharyngeal diphtheria, the following forms are distinguished: localized, widespread, subtoxic, toxic I, II, III severity and hypertoxic. Localized oropharyngeal diphtheria is the most common form. It is especially difficult to diagnose, since its clinical picture is similar to that of tonsillitis of other etiologies. The difficulty of diagnosis is aggravated by the presence of coccal pus-like flora. The disease begins acutely with chills or chills, an increase in body temperature, often not higher than 38 ° C, although on the 2nd day of illness there may be a higher temperature. At the same time, other signs of intoxication appear: headache, severe weakness, and possibly fainting. From the first hours of illness, a moderate sore throat appears when swallowing, which increases during the day. The submandibular lymph nodes are slightly painful on palpation, sometimes moderately enlarged. The febrile period lasts no more than 3 days. With normalization of temperature, all symptoms of intoxication practically disappear, pain in the throat decreases or disappears when swallowing. Depending on the nature of the fibrinous plaque within the palatine tonsils, oropharyngeal diphtheria is divided into island, membranous, and tonsillar variants. A number of clinicians identify the catarrhal form of diphtheria, with which there is no plaque on the tonsils. The mucous membrane of the oropharynx in the localized form of diphtheria is moderately hyperemic; as a rule, the hyperemic area has the appearance of a narrow rim bordering the film. The mucous membrane of the tonsils is swollen, the relief is smoothed. The film is located mainly on the convex surface of the tonsils, dense, grayish-white or dirty-gray in color with a smooth shiny surface, clearly defined edges (“plus” tissue), of equal thickness throughout, difficult to remove with a spatula. In the island version, the film has the appearance of sitting islands with irregular outlines; with membranous, the film covers a significant part of the tonsils, and with tonsillar, it envelops the entire tonsil. The film on the tonsils lasts 6-7 days without treatment. The widespread form of oropharyngeal diphtheria differs from the localized one only in the prevalence of the diphtheritic film, which spreads from the tonsils without interruption to the mucous membrane of the arches and uvula. In this case, the swelling of the mucous membrane of the oropharynx is moderate. The tonsillar lymph nodes are slightly enlarged and slightly painful on palpation. There is no swelling of the subcutaneous tissue of the neck. The common form of oropharyngeal diphtheria in adults is uncommon (no more than 5% of cases). Mild and moderate forms of oropharyngeal diphtheria, which include localized and widespread, are also characterized by pronounced pallor of the skin, tachycardia, and a tendency to hypotension. Toxic diphtheria of the oropharynx rarely develops after localized diphtheria; more often the disease occurs in a toxic form from the very beginning. For successful treatment of toxic diphtheria, an indispensable condition is early diagnosis (ideally, the 1st day of the disease). Toxic diphtheria begins acutely and violently. From the first hours of the disease, symptoms of intoxication are expressed. The temperature immediately rises to 39-40°C, chills, repeated vomiting, severe weakness, lethargy, even adynamia are often observed. Sometimes there may be abdominal pain. From the first hours of illness, patients complain of severe pain in the throat when swallowing, pain in the neck, and pain when opening the mouth (painful trismus). The tonsillar lymph nodes are significantly enlarged (to the size of a chicken egg), painful, and swelling of the subcutaneous tissue appears around them. The swelling is soft, doughy, painless, then, depending on the severity of the disease, the swelling spreads to the neck, sometimes descending to the chest to the xiphoid process; may rise behind the ears and onto the cheek area. The skin over the edematous tissues is usually unchanged. In the hemorrhagic form, the swelling of the tissue is denser, the skin over it may be pinkish in color. A sickly sweet smell emanates from the mouth. With toxic diphtheria, swelling of the mucous membrane of the oropharynx appears early, the severity of which correlates with the severity of diphtheria. Hyperemia of the mucous membrane is often stagnant, but at first it can be bright. The film in the first hours is thin, cobweb-like, then becomes dense, uneven in thickness, dirty-gray, quickly spreading beyond the tonsils, reaching the soft and even hard palate. The more severe the disease, the more striking symptoms appear in the first hours of the disease. In subtoxic diphtheria of the oropharynx, intoxication is moderate, plaques are often located on the tonsils, swelling of the subcutaneous cervical tissue is insignificant and is localized mainly in the area of the submandibular lymph nodes. Sometimes, in the subtoxic form, swelling of the subcutaneous tissue around the lymph nodes is not pronounced, but significant swelling of the mucous membrane of the oropharynx is detected with the diphtheritic film spreading from the tonsils to the arches and uvula. In case of toxic diphtheria of the 1st degree of severity against the background of severe intoxication, swelling of the mucous membrane of the oropharynx, the presence of a dense widespread plaque, swelling of the subcutaneous tissue of the neck by the end of the 1st - beginning of the 2nd day spreads to the middle of the neck, in the 2nd degree - to the collarbone and in the 3rd degree - below the collarbone. The most severe (malignant) forms of toxic diphtheria are hypertoxic and hemorrhagic. Hypertoxic diphtheria occurs with lightning speed. It begins violently, with high fever, repeated vomiting, delirium, and convulsions. Hemodynamic disorders and infectious-toxic shock develop rapidly. The hemorrhagic form develops more slowly and is characterized by the addition of hemorrhagic phenomena to the clinical picture of toxic diphtheria of the third degree of severity. The plaque becomes saturated with blood, hemorrhages appear in various places, and there may be bleeding. The number of platelets is significantly reduced, the deformability and architecture of erythrocytes are impaired. Diphtheria of the respiratory tract.
The next most common localization of diphtheritic inflammation is the respiratory tract and especially the larynx.
Diphtheria damage to the larynx and underlying respiratory tract is known as “true croup.” Depending on the distribution of the process, localized croup (diphtheria of the larynx), widespread (diphtheria of the larynx and trachea) and descending (larynx, trachea, bronchi) are distinguished. More often, diphtheria croup occurs in combination with diphtheria of the oropharynx, but can be isolated. In adults, due to its anatomical features, laryngeal diphtheria is difficult to diagnose; typical symptoms appear late. Sometimes the only symptom of damage to the larynx is hoarseness, even with descending croup. Respiratory failure may be indicated by pale skin, tachycardia, difficulty breathing, forced positioning, participation of the wings of the nose in breathing, patient anxiety, and agitation. In adults, diphtheria croup is most often recognized with stenosis of the larynx during the asphyxial period. Nasal diphtheria
as an independent form of the disease is rare in adults.
Localized nasal diphtheria (a process in the nasal cavity) occurs in catarrhal, catarrhal-ulcerative and membranous forms. Widespread (plaques spreading to the paranasal sinuses) and especially toxic nasal diphtheria (widespread plaques, swelling of the subcutaneous tissue under the eyes, in the cheeks and neck) are accompanied by severe symptoms of intoxication. Immunocompetent adults may develop ocular diphtheria
, usually in combination with oropharyngeal or nasal diphtheria.
There is a localized form of diphtheria of the eyes, which is clinically expressed by catarrhal conjunctivitis, a common form, which is characterized by the development of keratoconjunctivitis, and a toxic form, manifested by panophthalmitis with severe swelling of the eyelids and periorbital edema. Rare localizations of diphtheria include skin lesions
. The diphtheria process is layered on damaged areas (wounds, burns, eczematous areas, pyoderma, etc.), proceeds for a long time, is characterized by the appearance of infiltration and swelling of the skin, the formation of a fibrinous film, enlargement of regional lymph nodes and even swelling of the surrounding subcutaneous tissue (toxic form). Atypical forms may be observed (pustular, panaritium, phlegmon). Complications of diphtheria can be specific, i.e., caused by the effects of diphtheria exotoxin (infectious-toxic shock, toxic myocardial damage, polyneuropathy, toxic liver damage), and nonspecific, developing due to the addition of secondary bacterial flora (pneumonia, peritonsillar abscess). Infectious-toxic shock develops on the 2nd day from the onset of the disease in the hypertoxic form and on the 3rd - 4th day in toxic diphtheria of III severity. Death occurs from the consequences of progressive shock and disseminated intravascular coagulation syndrome, more pronounced in one of the shock organs: with the phenomena of edema and swelling of the brain, acute insufficiency of the adrenal glands, kidneys, and pulmonary edema. The most common complication of severe forms of diphtheria is toxic damage to the heart, traditionally defined as myocarditis. Diphtheria toxin causes a specific disorder of myocardial metabolism, accompanied by inflammation. As a result, myocardial contractility decreases, conductivity and excitability are impaired. These changes are detected most early by echocardiography and determination of the level of cardiac-specific enzymes (aspartate aminotransferase, creatine phosphokinase, HBD). Pathological changes on the ECG often precede clinical manifestations. ECG changes indicate severe diffuse and focal damage to the myocardium and conduction system of the heart. Increased activity of lactate dehydrogenase, creatine phosphokinase, and transaminases correlates with the depth of damage to the heart muscle. Clinically, this is manifested by progressive weakness, adynamia, severe pallor, and tachycardia. The boundaries of the heart quickly expand, the sounds become dull. In severe cases, a rhythm disturbance appears: tachyarrhythmia, bradyarrhythmia, gallop rhythm, atrial fibrillation, etc. Symptoms of heart failure quickly increase, which in some cases causes death. Some patients develop a clinical picture of cardiogenic shock - a sharp decrease in blood pressure (BP), oliguria, and impaired peripheral hemodynamics. The presence of this triad is a prognostically unfavorable sign. The earlier myocarditis develops, the more severe its course and the higher the risk of death. With a favorable outcome, the duration of severe myocarditis ranges from 4 to 6 months. Myocarditis of mild and moderate severity develops in patients with both toxic diphtheria and widespread and localized diphtheria of the oropharynx in untreated cases at 2-3 weeks of illness; their duration ranges from 1 - 2 to 1.5 - 3 months. A common complication of toxic diphtheria is toxic nephrosis. It is detected in the acute period of the disease (according to the results of a urine test). Albuminuria, hyaline and granular casts, a moderate number of erythrocytes and leukocytes, and an increase in the relative density of urine are detected. As a rule, blood pressure does not increase, and there is no edema. The severity and duration of nephrotic changes correspond to the severity of diphtheria. Sometimes acute pyelonephritis develops, but more often the symptoms of nephrosis disappear on their own after 2 - 3 weeks, and often earlier. Polyradiculoneuropathy is a complication that appears later than others. However, in mild forms of the disease and as the first phase in severe forms, monoparesis of the cranial nerves can develop. Mild paresis in patients with localized or widespread diphtheria is detected no earlier than the 2nd week (usually later) from the onset of the disease and lasts 2-3 weeks. Monoparesis in patients with toxic diphtheria occurs earlier, in the 2nd week, and usually represents the first phase of widespread neuropathy. Diphtheria neuropathy is the result of toxic damage to peripheral nerves and roots. It is characterized by the appearance of flaccid paresis with muscle atrophy, weakening of tendon reflexes, sensitivity disorder and radicular pain. In severe cases, death may occur due to paralysis of the intercostal muscles and diaphragm. The prognosis of the disease worsens significantly if pneumonia is added.
Differential diagnosis
Carrying out differential diagnosis of diphtheria without specifying the form can cause gross diagnostic errors. Localized diphtheria of the oropharynx is differentiated from tonsillitis of coccal and viral-bacterial etiology. Common diphtheria of the oropharynx should be differentiated, in addition to tonsillitis, with stomatitis, burns, the toxic form - with peritonsillar abscess, infectious mononucleosis, blood disease, mumps.
Diagnostics
The preliminary diagnosis is based mainly on clinical data and determines the decision on hospitalization and isolation of the patient, the need for treatment with anti-diphtheria serum (ADS) or the possibility of monitoring the patient without serotherapy. The diagnosis is confirmed by bacteriological examination of smears taken from the affected area. In typical cases, the lack of bacteriological confirmation is not a reason to cancel the clinical diagnosis of diphtheria. In case of an atypical course of the disease, rare localizations of the process, bacteriological confirmation of the diagnosis is mandatory. Patients with tonsillitis identified in epidemic foci, regardless of the results of bacteriological examination, are regarded as patients with diphtheria, unless it is possible to prove a different etiology.
Treatment
All patients with diphtheria or suspected of having it, as well as carriers of toxigenic corynebacteria, are subject to hospitalization. The main thing in the treatment of all forms of diphtheria, except for bacterial carriage, is the neutralization of diphtheria toxin by introducing an antitoxic PDS. If localized diphtheria is suspected, the administration of PDS can be delayed until the diagnosis is clarified, subject to observation of the patient in a hospital. If toxic diphtheria is suspected, the administration of PDS should be started immediately. The dose of PDS is determined by the severity of the disease. It is administered intramuscularly (IM) or intravenously (IV). IV administration (30 - 50% of a single dose) is recommended for toxic diphtheria of II and III severity and in the hypertoxic form.
In 1995, the Ministry of Health of the Russian Federation recommended the following doses of PDS (in thousand IU):
localized diphtheria of the oropharynx, nose, genitals, eyes, skin 15 - 30 IM widespread diphtheria of the oropharynx 30 - 40 IM subtoxic diphtheria 50 - 60 IM toxic diphtheria I degree of severity 60 - 80 IM II ' ' 80 - 100 IV or IM III ' ' 100 - 120 IV or IM hypertoxic 120 - 150 IV or IM croup localized 15 - 20 IM croup widespread and descending 30 - 40 IM
It should be noted that WHO recommends administering PDS in a dose not exceeding 60,000 IU for the most severe forms of diphtheria (the minimum dose for mild forms is 5,000 - 10,000 IU). A single injection of serum in the indicated doses guarantees a protective level of antitoxic antibodies for a long time. For localized and widespread forms of diphtheria, in addition to PDS, desensitizing therapy is indicated, as well as ascorbic acid for 3 to 5 days. It is recommended to rinse the oropharynx with a disinfectant solution. The administration of antibacterial agents does not have a significant effect on the course of the disease. For toxic diphtheria, simultaneously with the administration of PDS, antibiotics are prescribed for 5-7 days, which have an antibacterial effect on the accompanying microflora, which aggravates the course of the disease. For the purpose of detoxification and correction of hemodynamic disorders, albumin, plasma, rheopolyglucin, a glucose-potassium mixture with insulin, polyionic solutions, ascorbic acid, corticosteroids (prednisolone) are prescribed at the rate of 2.5 - 5 mg per 1 kg of body weight per day parenterally until swallowing is restored , and then 30-40 mg orally, followed by a dose reduction over 7-10 days. In the case of a toxic form, a positive effect in terms of detoxification is achieved by plasmapheresis with plasma exfusion from 60 to 100% of the volume of circulating plasma, followed by replacement with cryogenic plasma. A promising method of pathogenetic therapy is laser therapy. Treatment of complications of diphtheria involves the appointment of appropriate pathogenic therapy.
Treatment of bacteria carriers.
Of particular importance is the identification and treatment of chronic pathogenetic therapy. Treatment of ENT organs. When corynebacteria are repeatedly isolated, broad-spectrum antibiotics (erythromycin, tetracycline, rifampicin) are prescribed in medium therapeutic doses (course 5 - 7 days). It is advisable to irrigate the oropharynx with octenisept. For persistent carriage, the Codivak vaccine, created at the NIIEM, is used. G.N. Gabrichevsky. For adults, the vaccine is administered subcutaneously in the scapula area: on day 1 - 2 doses (6 mg), on days 2 - 3 - 1 dose (3 mg), on day 10 - 1 dose (3 mg). Medical examination of those who have recovered from the disease is carried out in the clinic by a local doctor together with an infectious disease specialist.
How does diphtheria manifest itself?
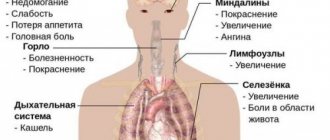
It is not for nothing that this disease is often compared to a sore throat. In the first one or two days, their symptoms actually coincide in many ways: inflamed tonsils, sore throat, fever, enlarged lymph nodes.
- Plaque on the tonsils. In the early stages, plaque covers them with a thin layer, similar to a cobweb, and is easily separated. But after 2–3 days, a dense, glossy, gray-white film forms on the tonsils. It is not removed from the tonsils, and when trying to artificially separate it, a bleeding surface opens.
- Heat. If in the first 1–2 days the temperature rarely rises above 38.5 degrees, then with the onset of intoxication it can reach 40 degrees and above.
- General intoxication. This condition develops quite quickly and can be severe. In addition to high temperature, general weakness, lethargy, pale skin, and lack of appetite are noted.
Due to the fact that the early signs of diphtheria are in many ways similar to a sore throat, any inflammation of the tonsils requires consultation with a doctor. If you miss the onset of diphtheria, there is a high probability of complications.
Symptoms and complications
Diphtheria can occur in different forms. In some cases, the patient experiences the formation of white filmy plaques, which then become gray and later turn slightly yellow. In other cases, there are no films; this is a catarrhal (atypical) form of diphtheria. Most often, doctors have to deal with diphtheria of the pharynx. It is manifested by dry mouth and pale skin of the patient; children may feel abdominal pain and nausea, which leads to repeated vomiting. The toxic form of pharynx diphtheria is accompanied by swelling in the neck or chest.
A person with diphtheria can face serious consequences: cardiovascular failure, paralysis of the respiratory muscles, or asphyxia due to diphtheria of the respiratory tract. If a disease in any form is detected, the patient must be hospitalized in the infectious diseases department of the hospital.
How dangerous is diphtheria?
The toxin produced by corynebacteria has a detrimental effect on all tissues of the body, but primarily the heart muscle and nervous tissue suffer because of it. Therefore, in the second week of the disease, myocarditis often begins, as well as disorders of the nervous system: partial paralysis of individual muscles, involuntary twitching, spasms, sensory disturbances, muscle weakness, and so on.
Along with general intoxication, the most dangerous complication of diphtheria is true croup. It occurs when inflammation from the tonsils spreads to the larynx. At first the voice changes, it becomes hoarse, hissing, and gradually disappears altogether. At the same time, a rough barking cough appears without sputum production.
With true croup, two conditions develop simultaneously: the lumen of the larynx is covered with diphtheria films, and also narrows due to tissue edema. The latter can be noticed by the increase in neck volume.
Without immediate treatment, croup can lead to respiratory failure and death due to suffocation.
Diagnostics
Diphtheria is diagnosed based on examination of the patient and test results. Upon examination, the diagnosis of diphtheria is indicated by the following signs: the presence of characteristic films, as well as difficulty breathing and a whistling noise when inhaling, not characteristic of a sore throat, a barking cough. The diagnosis of diphtheria based on characteristic clinical signs in a mild form of the disease is more difficult to make.
Analyzes:
- A general blood test shows signs of an acute inflammatory process.
- Examination of a smear under a microscope (bacterioscopy) - identification of the characteristic bacteria Corynebacterium diphteriae.
- Bacteriological research is the inoculation of biological material on a special nutrient medium and the cultivation of colonies of microorganisms.
- Determination of the level (titer) of antitoxic antibodies (a high titer of 0.05 IU/ml and above allows diphtheria to be excluded).
- Serological study - determination of specific antibodies in blood serum using the methods of RPGA, ELISA, etc.
Diphtheria of the pharynx must be differentiated from acute tonsillitis (follicular and lacunar forms), Simanovsky-Vincent angina (fungal infection), syphilitic angina, pseudofilm angina with infectious mononucleosis, paratonsillar abscess, mumps, leukemia. In children, the diagnosis of false croup should be avoided.
How is diphtheria diagnosed?
At any, even the slightest suspicion of this condition, the doctor recommends undergoing minimal diagnostics. As a rule, to establish the presence of a pathogen, it is enough to take a swab from the throat and nose. In the laboratory, it is examined under a microscope and, if pathogens are found in it, the necessary treatment is prescribed.
In addition to smear bacterioscopy, other diagnostic methods may be required, primarily bacteriological culture. It gives a more accurate result, and also allows you to determine the number of pathogens, and therefore the severity of the disease or the effectiveness of treatment.
Not only potential patients with diphtheria, but also all people who have been in contact with them need to undergo diagnostics. This often makes it possible to detect bacteria carriers, which means preventing further spread of the infection.
Preparation
All types of vaccines, both domestic and imported, containing diphtheria toxoid, are administered intramuscularly. Before vaccination, it is not recommended to introduce new complementary foods into the diet, or visit crowded places.
The doctor will tell you about all the features and limitations of the post-vaccination period at your appointment. The Miracle Doctor clinic provides immunization against diphtheria with a preliminary examination by a specialist using vaccines from leading foreign manufacturers.
Sign up for a consultation by phone or on the clinic’s website.
How can you avoid diphtheria?
The only specific method of preventing this disease is timely and complete immunization. The course of vaccinations is recommended to begin at 3 months after birth. It consists of several blocks:
- 3 vaccinations with an interval of 1.5 months: at 3 months from birth, at 4.5 and 6;
- buffer vaccinations to maintain immunity: at 1.5 years, at 4–5 and 14–15 years;
- lifelong periodic immunization every 10 years.
Do not think that diphtheria is a purely childhood disease, and adults do not need protection from it. You can get infected at any age, and it is always severe, although, indeed, it poses the greatest danger to children.
Important! Even previous diphtheria does not guarantee protection from re-infection. To exclude it, you should complete the course of immunization. In this case, the disease suffered is considered the first vaccination.
It's never too late to get vaccinated against diphtheria. If the child did not receive them at the right time in childhood, if the scheme was violated or too much time has passed since the last one, the course is started from scratch at any age. Up to 7 years of age, a “children’s” scheme is used, adjusted for age; adults receive several vaccinations: upon application, after a month and after a year.
Vaccines
Vaccines against diphtheria contain the main component that forms the body's immune response, but does not cause disease - diphtheria toxoid. Today, combination vaccines are effective. They contribute to the development of stable immunity to several infectious diseases at once. The combination of diphtheria toxoid and other components in such vaccines is immunologically substantiated and favorable. Thanks to this, the number of injections is reduced, and the effectiveness of immunization becomes higher.
- DTP (vaccine against whooping cough, diphtheria and tetanus). It is a standard vaccine that is administered to children from infancy. It contains inactivated cells of the causative agent of whooping cough, diphtheria bacillus and tetanus toxoids.
- DDT (diphtheria and tetanus vaccine). The drug is classified as bivalent, as it successfully copes with immunization against two infections and is used for revaccination. This immunobiological drug is used for children who have already had whooping cough or who are contraindicated for the DTP vaccine for one reason or another.
- ADS-M (vaccine against diphtheria and tetanus). Children over 6 years of age and adults need a smaller dose of toxoids to produce the same lasting immunity, and this makes the vaccine more tolerable.
The emergence of imported polyvalent (multicomponent) vaccines makes it possible to effectively and safely vaccinate children against dangerous infections, including diphtheria. Diphtheria toxoid is included in the vaccines Pentaxim, Infanrix, Infanrix Hexa, Adasel.
At your appointment, a pediatrician, therapist or immunologist can explain in detail the differences and benefits of different combination vaccines and create an immunization schedule for diphtheria and other infectious diseases.