Chronic obstructive pulmonary disease ranks 4th in the list of causes of death on our planet (data from the World Health Organization).
Unfortunately, it remains incurable today. However, modern medicine can slow the progression of the disease, reduce symptoms and improve quality of life.
In this article you will learn about modern scientifically proven methods of prolonging the life of patients, which are today recommended by leading pulmonologists in our country and around the world.
Fragment of the TV show “Live Healthy.” COPD The rights to the video belong to
OJSC “Channel One”. The full version of the TV show is available at this link.
Chronic obstructive pulmonary disease (COPD) is a multicomponent disease, which is based on chronic inflammation and narrowing of the small airways (bronchi) with the destruction of lung tissue (alveoli), the formation of its “overinflation”, which leads to cough, progressive shortness of breath and fatigue. . COPD is a serious disease that progresses over many years, accompanied by a lack of oxygen in the body. In the absence of necessary treatment, the consequences of COPD are disability and death.
Why might I develop COPD?
The most common cause of the development of this disease is smoking (cigarettes, hookah and other smoking mixtures). The smoke you inhale when smoking damages the bronchi and lung tissue (alveoli). Moreover, the damage is irreversible! The longer you smoke, the more pronounced changes occur in the respiratory system. It is very important to understand that passive smoking leads to the same consequences as active smoking.
Other reasons may be:
- work in hazardous production conditions (miners, welders, metallurgical and chemical industry workers);
- prolonged inhalation of smoke generated by the combustion of biofuels (wood, coal for stove heating);
- living in environmentally unfavorable conditions.
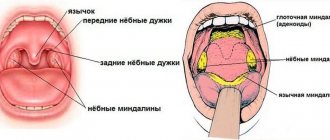
How does the respiratory system work?
The respiratory system consists of the airways and lungs. The supply of oxygen to the body's cells occurs through its transfer to the alveoli of the lungs and then into the blood.
Alveoli are the structural part of the lungs. They are thin-walled bubbles with a diameter of 0.2 mm, braided by a network of capillaries. The lungs contain about 500 million alveoli. Through capillaries, oxygen enters the blood and is distributed throughout all systems of the body. And also through capillaries, the waste product - carbon dioxide - is delivered from the body to the alveoli.
The lower respiratory tract is the trachea and bronchi. When you inhale, oxygen is transported through them into the lungs with air, and when you exhale, carbon dioxide is released.
The bronchi are a paired organ that branches from the trachea to the right and left lungs. They are an extensive network of tubes that fill the entire volume of the lungs. The thin tips of the bronchi end in many alveoli.
In addition to the transport function, the bronchi have another important one – protective. The air passing through them is warmed, disinfected and filtered.
The protective function works due to the structure of the epithelium of the inner walls of the bronchi and the bactericidal mucous secretion that is produced in the bronchi.
Global Alliance to Fight Chronic Respiratory Diseases
The Global Alliance Against Chronic Respiratory Diseases (GARD) promotes WHO's work to prevent and control chronic respiratory diseases. GARD is a broad voluntary alliance of national and international organizations and institutions working towards the common goal of reducing the global burden of chronic respiratory diseases.
Bibliography
1. WHO Global Health Estimates
2. Assessing national capacity for the prevention and control of noncommunicable diseases: report of the 2021 global survey. Geneva: World Health Organization; 2021. License: CC BY-NC-SA 3.0 IGO
COPD - what kind of disease is it?
For various reasons, the body's protective barrier does not always work. The mucous membranes are damaged, and then an immune response occurs in the tissues - inflammation. This can happen due to allergens, inhalation of harmful substances, pathogenic bacteria and viruses.
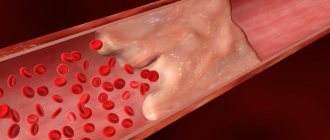
With inflammation of the bronchi (bronchitis), the tissues swell, turn red, the amount of mucus increases sharply, and it becomes viscous. If the diameter of the bronchi narrows, their ability to conduct air correspondingly deteriorates. This phenomenon is called obstruction. With obstruction, the patient experiences difficulty breathing, shortness of breath, and possible spasm. If inflammation affects the alveoli, pneumonia occurs.
Obstruction is characteristic of bronchial asthma, a complicated form of acute and chronic bronchitis (obstructive bronchitis).
But what is COPD and how does it differ from these diseases? The fact is that obstruction can be reversible. In asthma, the cause of obstruction is bronchospasm, when the bronchial muscles contract, leading to a narrowing of the lumen of the bronchi. The use of antispasmodics and bronchodilators relieves the attack.
In acute bronchitis, after recovery, the tissue heals and restores its functions.
Chronic obstructive disease is characterized by irreversible processes in the tissues of the bronchi and alveoli. In this case, changes occur at the organic level, and the obstruction is difficult to eliminate with drugs. As a result, the respiratory system can no longer cope with its tasks, and the person experiences chronic respiratory failure.
The body's tissues chronically lack oxygen, and carbon dioxide is not eliminated properly. In addition, the altered mucous membrane cannot cope with microbes and viruses, and the patient begins to suffer from infectious diseases. Chronic obstruction tends to progress.
The disease affects the bronchi and lungs, and includes chronic obstructive bronchitis and pulmonary emphysema. Most patients have signs of both diseases.
Causes of obstructive disease
The main cause of the development of pathology is chronic smoking. There are a number of other factors that can trigger the onset of COPD:
- abundance of exhaust gases, smoke, dust;
- air pollution from industrial waste;
- work in hazardous conditions (coal mine, hot shop, chemical industry);
- climatic features (dampness, constantly high humidity);
- infectious microorganisms (influenza virus, pneumococcus, mycoplasma bacteria and others);
- development of concomitant pathologies of the bronchi and lungs, especially bronchial asthma (including inherited).
How does COPD develop?
The disease develops gradually. Its mechanism is triggered by unfavorable external influences that provoke an inflammatory process in the organs of the respiratory system. Another important factor is genetic predisposition, which causes an imbalance in the destruction and synthesis of healthy tissue.
During inflammation, pulmonary proteases are released - enzymes that break down the molecules of the mucous tissue of the bronchi and lungs. Normally, this process is balanced by the work of antiproteases, which are “responsible” for the restoration of molecules. One of the proteases is alpha-1-antitrypsin. In some cases, people with COPD have a deficiency of alpha-1 antitrypsin. This means that the activity of antiproteases is reduced, and the process of tissue destruction prevails over the restoration process.
If the healthy structure of the bronchial mucosa does not have time to recover, it is replaced by fibrous connective tissue, like scar tissue. If the harmful effects do not stop, this rough tissue gradually grows, thickening the walls of the bronchi and narrowing their diameter. Also, during the inflammatory process, hypersecretion of mucus occurs, which clogs the passage of the bronchi. After some time, the process becomes irreversible and begins to progress even if the harmful factors are eliminated.
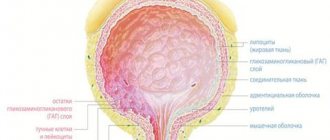
If the bronchi thicken when damaged, the walls of the alveoli, on the contrary, are destroyed. As a result, a pathological expansion of the air spaces occurs, the parenchyma becomes more weakly attached to the respiratory tract, which leads to difficulty in the release of air during exhalation. Destroyed alveoli can form bullae (air cysts) with a diameter of more than 1 cm. Such pathologies lead to loss of elastic strength of the lungs and their hyperairiness.
What factors lead to the development of the disease?
Smoking
According to statistics, about 75% of COPD cases are caused by heavy smoking. Smoking 20 cigarettes a day for more than 20 years or longer is highly likely to lead to a clinically established diagnosis. If you regularly smoke passively for about 20 hours a week, your risk of getting sick doubles.
Adverse Occupational Exposures
Work in conditions of increased gas, dust and chemical contamination - that is, when inhaling substances that damage the mucous membrane of the respiratory tract, for example, in asbestos, gypsum factories, mines.
The risk of disease increases if work or living conditions involve inhalation of tars resulting from the combustion of wood, coal and other biofuels, with insufficient ventilation of the room.
Severe bronchial asthma
If asthma continues for a long time with severe attacks, bronchial obstruction gradually ceases to be reversible and becomes chronic. This is especially likely if the diagnosis was established in childhood.
Chronic infections
Recurrent infectious diseases of the lower respiratory tract can lead to chronicity and the development of obstruction. In turn, people with COPD often suffer from respiratory tract infections. Chronic obstruction leads to stagnation of mucus in the lower respiratory tract, which promotes the proliferation of bacteria. This in turn increases inflammation and further damage to bronchopulmonary tissue. This means it leads to faster progression of the disease.
How does COPD differ from bronchial asthma?
The symptoms of the diseases are similar, but, nevertheless, there are obvious differences that make it possible to make an accurate diagnosis and prescribe the correct treatment. COPD rarely has a direct allergic origin. Asthma is often associated with allergies. COPD is most often a disease of older people who smoke. The prognosis for treatment of this disease is determined by a special formula: the number of cigarettes that the patient smoked during the day is multiplied by the duration of smoking in years. And the higher the result, the worse the prognosis.
Asthma occurs even in young children. In addition, asthma is a paroxysmal cough that appears after contact with substances that cause an allergic reaction. In COPD, symptoms progress over several years.
Asthma is accompanied by conjunctivitis, atopic eczema, and COPD is complicated by diseases of the cardiovascular system.
Symptoms of COPD
Cough is the earliest sign of the disease. At first it is episodic, then becomes daily. A smoker's cough can be considered an early symptom of developing obstructive disease.
Sputum separation. Relatively early symptom. During the period of remission there may be no sputum.
Dyspnea. Appears approximately 10 years after the onset of the disease. At a later stage, shortness of breath appears even with minor physical exertion, up to severe respiratory failure.
Breath. Weak, whistling, shortened on exhalation. Breathing through clenched teeth.
Weight loss.
Barrel chest.
With the development of respiratory failure, the patient's skin acquires a bluish tint, swelling and puffiness of the face occur. The ends of the phalanges of the fingers thicken.
In advanced forms of the disease, a person may develop signs of carbon dioxide poisoning (usually at night).
Classification
COPD is classified according to the severity of clinical manifestations. Before describing the criteria, let us explain the meaning of key indicators:
1. Forced expiratory volume (FEV1). The indicator reflects the volume of air that the patient is able to exhale in one second at maximum speed.
2. Forced vital capacity (FVC). This is the volume of air that a patient can exhale after taking the deepest breath possible. As with FEV1, volume is measured in liters.
When classifying COPD, experts distinguish four stages4, focusing on the severity of the disease:
1. Lightweight. There is a cough and moderate sputum production. FEV1 – at least 80%, FVC – 70% of normal.
2. Average. The cough and sputum production intensify, and shortness of breath occurs during physical exertion. Episodes of exacerbations begin. FVC – 50%, FEV1 – 70%.
3. Heavy. In addition to an increasing cough with sputum, shortness of breath occurs even with slight exertion. Exacerbations are becoming more frequent. FVC – 30%, FEV1 – below 50%.
4. Extremely heavy. Shortness of breath at rest, symptoms of cor pulmonale. Chronic exacerbations begin to pose a danger to the patient's life. FEV1/FVC – less than 30%.
Exacerbations of COPD are considered chronic if they occur at least 3 times a year, despite ongoing therapy.
Figure 2. Chronic obstructive pulmonary disease: how it affects breathing. Image: brgfx/freepik.com, NIH Image Gallery/Flickr
Diagnostics
The disease develops long before the onset of functional disorders, which can be recorded instrumentally. Therefore, unfortunately, early diagnosis of COPD is almost impossible.
When diagnosing, the following methods are used:
- X-ray and CT (computed tomography) of the chest;
- study of the function of the respiratory system using spirometry and other tests;
- sputum cultures for microflora;
- determining the level of alpha-1-antitrypsin;
- ECG and echocardiography to exclude cardiac causes of shortness of breath and identify cardiac complications.
When diagnosing, it is important to differentiate COPD from diseases with a similar clinical picture - asthma, heart failure.
4. Treatment of COPD with deterioration and progression of the disease
As COPD progresses, the patient experiences increased shortness of breath and more frequent attacks of COPD. In addition to pulmonary rehabilitation aimed at maintaining daily physical activity, other treatment methods are used.
Oxygen therapy, methylxtantines, or oral corticosteroids may relieve symptoms. A separate direction in the treatment of COPD is surgery
.
For severe COPD, different types of surgery may be performed. For example, lung reduction surgery
(removing part of one or both lungs) helps the remaining lungs function better.
Lung transplantation
is the replacement of a lung with donor material.
A bullectomy
is an operation during which bullae are removed from the lungs (it is usually performed in patients with pulmonary emphysema). Bullae form when the tiny air sacs in the lungs become too large. Sometimes so much so that they interfere with breathing.
It is important that over time, doctors develop more and more new methods of treating COPD. And therapy prescribed by a qualified doctor will help prolong life, minimize the symptoms of COPD and prevent severe attacks of the disease. Therefore, it is important to find a competent and qualified specialist for the treatment of COPD.
Treatment
The strategic goal in the treatment of stable obstructive disease is to prevent exacerbations and increase the functionality of the respiratory system.
For this purpose, a set of measures is used:
- Quitting smoking. Is crucial in therapy.
- Inhaled bronchodilators are drugs that dilate the bronchi.
- Inhaled corticosteroids – reduce inflammation and relieve symptoms.
- Phosphodiesterase-4 inhibitors have anti-inflammatory and bronchodilatory effects.
- Oxygen therapy is treatment with oxygen.
- Normalization of nutrition.
- Physiotherapy.
- In some cases, surgery is indicated.
Patients with COPD are advised to get vaccinated against influenza to avoid complications and sudden progression of the disease.
What is the optimal duration of antibiotic therapy for exacerbation of COPD?
The possibility of using 5-day courses of ABT was demonstrated in RCTs for drugs such as AMK, cefditoren, levofloxacin, moxifloxacin, gemifloxacin [37, 38].
Short courses of ABT (about 5 days) compared to “traditional” long courses guarantee higher patient adherence to therapy, especially in an outpatient setting [29]. For patients taking ABT, skipping a dose or unplanned interruption of the course of therapy means not only a decrease in the effectiveness of therapy, but also an increased likelihood of “selection” of resistant microorganisms [29]. Numerous studies show that the longer the duration of treatment, the fewer patients complete this treatment [39]. A single dose of the drug during the day also significantly improves patient adherence to therapy [39].
The ME Falagas meta-analysis, based on 7 RCTs (3083 COPD patients), compared treatment with the same antibiotic at the same doses but with different durations of therapy (5 days versus 7–10 days) [38]. The meta-analysis showed no differences between the compared treatment groups in terms of achieving clinical success (OR = 0.99; 95% CI - 0.95–1.03), however, short courses of ABT turned out to be safer, since they were accompanied by significantly less number of adverse drug reactions (OR = 0.84; 95% CI – 0.72–0.97) [38].
These results should be extrapolated with caution to hospitalized COPD patients with severe exacerbations. Today there is no exact answer to the question about the duration of ABT for severe exacerbation of COPD. Determining the duration of antibiotic therapy in COPD patients with severe exacerbations can be based on monitoring the levels of inflammatory biomarkers [40].
Complications
The course of COPD is characterized by the following complications:
- Respiratory failure.
- Recurrent respiratory tract infections.
- Pulmonary hypertension (increased pressure in the pulmonary circulation).
- Failure of the right ventricle of the heart (cor pulmonale).
- Pneumothorax (accumulation of air in the pleural cavity).
- Lungs' cancer.
- Cardiac ischemia.
- Anxiety and depressive disorders.
- Weight loss.
The complicated course of the disease ends in death in 50% of cases within 10 years after diagnosis. The prognosis largely depends on whether the patient managed to quit smoking and how long he had as a smoker before.
Prevention of influenza and pneumococcal pneumonia
Because pulmonary infection is common in patients with COPD and can lead to deterioration of lung function and respiratory failure, annual influenza vaccination is recommended for patients who are not allergic to egg whites. Its effectiveness reaches 60-80%. Unvaccinated patients at high risk of influenza A and at an early stage are prescribed amantadine. For patients over 50 years of age, a single immunization with the pneumococcal vaccine is also recommended. Revaccination is now carried out after five or more years, if at the time of vaccination the patient’s age did not exceed 65 years.