Legionellosis ranges in severity from a mild febrile illness to a serious and sometimes fatal form of pneumonia and is caused by exposure to a variety of Legionella bacteria that is found in water and soil mixtures.
Cases of Legionnaires' disease are often classified based on the type of exposure (community-acquired, travel-acquired, or hospital-acquired).
The most common cause of illness, including outbreaks, is the bacterium Legionella pneumophila. Legionella pneumophila and related species are commonly found in lakes, rivers, streams, hot springs, and other bodies of water. Other species, including L. longbeachae, can be found in potting mixes.
The bacterium L. pneumophila was first identified in 1977. It was the cause of an outbreak of severe pneumonia at a convention center in the United States in 1976. It has since been associated with outbreaks associated with poor maintenance of man-made water systems, particularly in cooling towers and evaporative condensers used in air conditioning and industrial refrigeration systems, hot and cold water systems in public and private buildings, and in hot tubs. .
The dose of infection is unknown, but in susceptible individuals it can be assumed to be low because symptoms appear after short exposure and at distances of 3 km or more from the source of outbreaks. The likelihood of disease depends on the concentration of Legionella in the water source, the production and spread of aerosols, characteristics of the infected person such as age and pre-existing health status, and the virulence of the particular strain of Legionella. In most cases of infection, the disease does not manifest itself.
Cause
The causative factors are Legionella bacteria found in water or soil mixtures. The most common cause of the disease is the freshwater species L. pneumophila, which is found in natural aquatic environments throughout the world. However, the most likely source of the disease is artificial water systems, which create conditions conducive to the growth and spread of Legionella.
These bacteria live and multiply in water systems at temperatures of 20-50 degrees Celsius (optimal temperature is 35 degrees Celsius). Legionella can survive and reproduce as parasites in single-celled protozoans and biofilms that form in aquatic systems. They can cause infection by infecting human cells, a mechanism similar to that of protozoan infections.
Epidemiology of Legionnaires' disease
The natural habitat of bacteria is freshwater bodies of water and soil. They multiply intensively at a temperature of 35-40 degrees in protozoa, for example, in amoebas, which protect them from the effects of negative factors for them, including high concentrations of chlorine. Due to their high adaptive properties, Legionella successfully colonizes compressor devices, cooling systems, swimming pools, shower installations, decorative fountains, etc. Moreover, in artificial structures the conditions for the survival of bacteria are usually more favorable than in natural habitats.
A person infected with Legionnaires' disease is not a source of the infectious agent, even if they have close contact with it.
The main mechanism of transmission of bacteria is aerosol, i.e. infection occurs when a person inhales aqueous aerosol from contaminated sources. Infection is also possible through airborne dust (by inhaling soil particles containing bacteria), for example, during construction or excavation work.
Legionellosis is widespread, but the incidence is higher in economically developed countries. Hotel residents and medical workers are more likely to get sick. Among the population, outbreaks usually occur in the summer and autumn months (infected through drinking water).
Broadcast
The most common form of transmission of Legionella is through inhalation of contaminated aerosols. Sources of aerosols that have been associated with transmission of Legionella include air conditioning cooling towers, hot and cold water systems, humidifiers, and hot tubs. Infection—especially among vulnerable hospital patients—can also occur through aspiration of contaminated water and ice, and when newborn babies are exposed to the bacterium during water births. The infection is not transmitted directly from person to person.
The causative agent of Legionnaires' disease
Legionellosis has been known since 1976. Then the disease manifested itself in the form of an outbreak of acute respiratory viral infection, accompanied by severe pneumonia and a high percentage of deaths among participants in the American Legion convention in Philadelphia. 4,400 people took part in the congress, 182 of them fell ill, and 29 died. It was then that this infection was called “legionnaires’ disease.”
The causative agent of this disease was isolated from the lung tissue of one of the deceased a year later by D. McDade and K. Shepard - it was named Legionella pneumophilia.
The clinical and immunological similarities of this disease with some other cases of infection reported in the United States and Spain were later studied. Based on these studies, the term “legionellosis” was introduced into practice in 1982 - it united all diseases caused by various types of legionella.
So, the causative agent of Legionnaires' disease is aerobic motile bacteria of the genus Legionella of the Legionellaceae family, which has more than 40 species of Legionella, 22 of which are pathogenic for humans. In 90% of cases, the causative agent is Legionella pneumophilia.
Incidence rate
The prevalence of known cases of Legionnaires' disease varies widely depending on the level of surveillance and reporting. Since many countries do not have adequate diagnostic methods for this infection or sufficiently developed surveillance systems, incidence rates are unknown. In Europe, Australia and the USA, there are about 10-15 cases per year per million inhabitants.
It is reported that 75-80% of patients are over the age of 50 years and 60-70% of them are men. Other risk factors for community-acquired legionellosis not associated with travel include: smoking, binge drinking, lung disease, impaired immunity and chronic respiratory or kidney disease.
Risk factors for hospital-acquired pneumonia include the following: recent surgery, intubation, which is the process of inserting a tube into the windpipe, mechanical ventilation, suction, presence of nasogastric tubes, and use of respiratory therapy equipment. The most susceptible subjects are patients with compromised immune systems, including organ transplant and cancer patients, and patients taking corticosteroids.
Prognostic factors for death due to Legionnaires' disease are late diagnosis and late initiation of appropriate treatment with antibiotics, advanced age and the presence of concomitant diseases.
Diagnostics
Diagnosis of legionellosis is always complex and consists of carrying out the following activities:
- listening to sounds in the lungs;
- X-ray of the lungs;
- laboratory tests: bacteriological studies of blood, sputum and pleural fluid, clinical (general) blood test, blood test to indicate pathogen antigens using ELISA and RIF methods.
When making a diagnosis, a differential diagnosis of legionellosis with the following diseases is required:
- pneumonia of various etiologies (pneumococcal, mycoplasma, staphylococcal, provoked by Pseudomonas aeruginosa, klebsiella, etc.);
- ARVI;
- psittacosis;
- Q fever and other pulmonary pathologies.
Symptoms
Legionellosis is a general term that describes pulmonary and non-pulmonary forms of Legionella infection.
The nonpulmonary form (Pontiac disease) is an acute, self-limiting influenza-like illness that usually lasts 2 to 5 days. The incubation period ranges from several hours to 48 hours. Main symptoms: fever, chills, headache, malaise and muscle pain (myalgia). This type of infection is not fatal.
The incubation period for the pulmonary form of Legionnaires' disease ranges from 2 to 10 days (however, in a number of outbreaks that have occurred, it has been up to 16 days). Symptoms initially include fever, loss of appetite, headache, malaise and lethargy. Some patients may experience muscle pain, diarrhea, and confusion. A mild cough is also common, but up to 50% of patients may produce sputum. Bloody sputum or hemoptysis may occur in approximately one third of patients. The severity of this illness ranges from a mild cough to a rapidly fatal pneumonia. Death occurs as a result of progressive pneumonia with respiratory distress and/or arrest and multiple organ failure.
If Legionnaires' disease is left untreated, it usually gets worse within the first week. Like other risk factors for severe pneumonia, the most common complications of Legionnaires' disease are pulmonary failure, shock, and acute kidney and other organ failure. Restoration of function in all cases requires treatment with antibiotics and usually takes several weeks or months. In rare cases, severe progressive pneumonia or ineffective treatment of pneumonia can cause complications in the brain.
Mortality rates from Legionnaires' disease depend on the severity of the disease, the adequacy of initial antimicrobial treatment, the site of Legionella infection, and the characteristics of the patient (meaning that the disease tends to be more severe in immunocompromised patients). The mortality rate can be as high as 40-80% in patients who are not treated for immunocompromised conditions, and can be reduced to 5-30% through appropriate management and depending on the severity of clinical indications and symptoms. Overall, the mortality rate is usually 5–10%.
Treatment
Patients with severe legionellosis must be hospitalized. In the future, treatment tactics are determined individually.
For Pontiac fever, therapy may be limited to symptomatic medications without antibiotic therapy. The patient may be prescribed:
- antipyretic and anti-inflammatory drugs;
- nasal drops;
- expectorants;
- multivitamin preparations;
- drinking plenty of fluids.
For other forms of legionellosis, the patient is prescribed macrolide antibiotics. The most effective is Erythromycin. It can be administered intramuscularly or intravenously (stream or drip). In the absence of positive dynamics, the patient is additionally prescribed Rifampicin. The course of antibiotic therapy is usually about 2-3 weeks. If necessary, the effect is secured by prescribing Pefloxacin or Ofloxacin.
Treatment aimed at eliminating the pathogen is complemented by measures to combat intoxication, the development of bleeding, respiratory, cardiac and renal failure. To eliminate gas exchange disorders, oxygen therapy and artificial ventilation are often performed. If necessary, anti-shock measures are provided.
First aid for suspected legionellosis
Legionellosis is recommended to be treated in a hospital setting due to the likely occurrence of acute respiratory failure, so if you suspect this infection, you should consult a doctor. At home, it is allowed to use antipyretics containing paracetamol and nimesulide (for example, Coldrex, Fervex, Nise and others), warm, abundant drinks (tea, fruit drinks, juices, water) and small meals, and it is advisable to serve meals at room temperature.
It is necessary to provide the patient with comfortable living conditions, with ventilation, wet cleaning with disinfectants. It is recommended to change bed and underwear regularly, using only products made from natural fabrics.
It is not advisable to wrap the patient so as not to cause an even greater temperature reaction in the body.
When is it not Legionnaires' disease?
Legionnaires' pneumonia does not have any characteristic signs unique to it, and proceeds like ordinary bacterial pneumonia. Only a doctor can distinguish and prescribe the correct treatment in time. The information below is intended to show the range of diseases that can mimic legionellosis.
Infectious pathology
In the autumn-winter period, you can encounter outbreaks of severe pneumonia, mainly among young people in organized groups. These pneumonias also often require hospitalization, but are caused not by Legionella, but by mycoplasmas. You should also clarify information about constant or short-term contact with birds (ornithosis), tick ingestion (Q fever), and the presence of HIV infection (pneumocystis pulmonary disease).
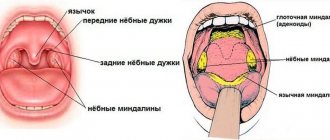
Massive diseases in the autumn-winter season with manifestations of damage to the nasopharynx (runny nose, nasal congestion, sore throat), high fever can also be complicated by pneumonia that is not related to Legionella (influenza, ARVI). We should not forget about the possibility of tuberculous (caseous) pneumonia, therefore the presence of tuberculosis in the family and in the patient should be clarified.
Therapeutic diseases
Legionella pneumonia differs little from ordinary pneumonia and does not have specific symptoms. However, in the presence of hypothermia and an adequate response to the standard antibiotics used, the diagnosis of legionellosis is questionable.
Which doctor should I contact?
If you have a cough and fever, it is best to consult a pulmonologist. However, at the first stage, both a therapist and a family doctor can help the patient. After clarifying the diagnosis, you will probably need to consult an infectious disease specialist. If organs other than the lungs are affected, the patient is examined by a cardiologist, neurologist, ophthalmologist, gastroenterologist, nephrologist. If infectious-toxic shock develops, treatment is carried out by a resuscitator.
Rating: (votes - 1 , average: 5.00 out of 5)
How does the disease develop?
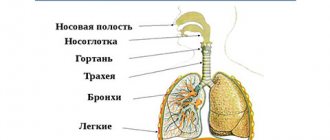
Legionella enters the human body through the respiratory tract. The pathogen is fixed in different parts of the respiratory system (including in the lung tissue). The depth of its penetration depends on the size of aerosol infected particles, their dose and breathing patterns. Microorganisms can also enter the human body along with protozoa infected by them and during certain surgical and other medical procedures. It is possible that they will be introduced into the body along with contaminated drinking water.
Through the bloodstream, the pathogen can enter various systems and organs. The lungs, liver, kidneys, nerve tissues and bone marrow are most often affected. With a high level of Legionella in the blood, the disease can develop as a septic type and be accompanied by the appearance of secondary purulent foci or septic endocarditis.