Rhinopharyngitis is an inflammatory process that affects the mucous membranes of the nose and pharynx, most often of infectious etiology. The peak of the disease usually occurs in childhood, especially preschool age. As a rule, inflammatory diseases of the nasopharynx are viral in nature. The course of nasopharyngitis is quite favorable, the disease resolves within 7-10 days. However, if it is repeated frequently, it causes serious discomfort.
The main etiological agents that cause inflammation of the nasopharynx include viruses. Although there are more than 200 viruses that have a causal relationship with the occurrence of nasopharyngitis, the most common types are the following:
- Coronavirus
- Respiratory syncytial virus
- Adenovirus
- Rhinovirus
- Influenza virus
- Parainfluenza virus
- Enterovirus
Causes of nasopharyngitis
Rhinopharyngitis is predominantly an infectious disease. In more than 80% of cases, especially in the autumn-winter period, it is caused by viruses - rhinovirus, adenoviruses, influenza viruses, etc. Bacterial nasopharyngitis occurs slightly less frequently. In this case, the causative agents of the disease are chlamydia, mycoplasma, streptococcus and staphylococcus.
Separately, we can distinguish allergic rhinopharyngitis, which develops under the influence of allergens that penetrate the upper respiratory tract - plant pollen, animal hair, tobacco smoke, household chemicals, etc.
Risk factors for developing a runny nose: hypothermia, weak immunity, the presence of chronic ENT diseases or pathologies of internal organs.
Prevention
By following simple recommendations from doctors, you can avoid nasopharyngitis and its many complications.
Advice from an otolaryngologist:
- timely treatment of viral and infectious diseases;
- rational nutrition and drinking regime;
- preventive intake of vitamin-mineral complexes in the spring-autumn period;
- flu vaccination;
- use of oxolinic ointment in winter;
- compliance with personal hygiene rules;
- strengthening the immune system.
Related services: Pediatric otolaryngologist ENT combine
Symptoms of nasopharyngitis
The disease develops acutely:
- the nasal mucosa swells;
- copious watery or mucous discharge appears;
- nasal breathing becomes difficult;
- there is a burning and itching sensation in the nose;
- your throat starts to hurt;
- body temperature rises.
Swelling of the mucous membrane contributes to nasal congestion, which leads to a decrease or loss of smell, a change in the timbre of the voice (a specific nasal sound appears). The patient often sneezes and his head begins to hurt. The mucus formed in the nose flows down the back wall of the throat, causing a reflex cough. Lymph nodes in the neck may become enlarged.
Rhinopharyngitis in children has a similar clinical picture. In addition, children are often capricious and refuse to eat.
If left untreated, chronic nasopharyngitis develops. Nasal congestion occurs periodically, most often it occurs on the half of the nose on the side of which the person is lying (left - on the left side and vice versa). When lying on your back, nasal breathing becomes completely difficult. Other symptoms characteristic of the acute form of the disease are usually absent. If atrophic rhinitis develops, patients complain of dryness and itching in the nasal cavity, and crusts with an unpleasant odor form in the nose. In the case of hypertrophic chronic rhinitis, the nose is constantly blocked.
Sore throat, rhinitis, tonsillitis, sinusitis, pharyngitis, laryngitis
Sore throat is an acute general infectious disease with a predominant lesion of the palatine tonsils. The inflammatory process can also develop in other accumulations of lymphadenoid tissue of the pharynx and larynx - in the lingual, laryngeal, nasopharyngeal, tonsils. Then, accordingly, they speak of lingual, laryngeal or nasopharyngeal sore throat. Infection can be from the outside or from one’s own microbes. There are two possible routes of infection transmission: airborne and foodborne. But most often, internal infection occurs from the oral cavity or pharynx (chronic inflammation of the tonsils, carious teeth, etc.). The source of infection can also be purulent diseases of the nose and paranasal sinuses.
The most common causative agents of infection are staphylococcus, streptococcus, and pneumococcus. There is information about the possibility of viral sore throats. Predisposing factors: local and general cooling, decreased body resistance. Sore throat most often affects children of preschool and school age and adults under 35-40 years of age, especially in the autumn and spring periods.
Comprehensive systemic program for sore throat, rhinitis: Antibiotics,
Anti-inflammatory drugs,
Reducing congestion in the sinuses,
Improving the strength of blood vessels,
Improved blood circulation.
With colds and a runny nose, the mucous membrane of the pharynx usually also becomes inflamed - pharyngitis . It becomes dry, red, irritated and swollen. In this case, viruses are usually the cause. However, a secondary infection from bacteria, which manifests itself in weakened immunity, is often added here.
Along with acute inflammation of the pharynx, its chronic form is also observed. It is caused by prolonged irritation of the mucous membrane by dust, smoking, alcohol, enlarged tonsils or constant breathing through the mouth (for example, due to a deviated nasal septum, chronic inflammation of the paranasal sinuses).
Acute inflammation of the larynx - laryngitis often occurs in combination with other ailments from a cold; in this case, the pharynx usually becomes inflamed. The causative agents of the disease are viruses, less often bacteria. The disease may be of an allergic nature. Chronic inflammation occurs when the vocal cords are overstrained (teachers, singers), irritated by tobacco smoke and other toxic fumes.
Sore throat begins with pain when swallowing, malaise, and increased body temperature. Complaints of joint pain, headache, and periodic chills are common. The duration of the disease and local changes in the tonsils depend on the form of tonsillitis. With rational treatment and adherence to the regimen, angina lasts on average 5-7 days.
There are catarrhal, follicular and lacunar forms of angina. Essentially, these are different manifestations of the same inflammatory process in the palatine tonsils.
In the vast majority of cases, recurrent tonsillitis plays a major role tonsillitis As a result of repeated acute inflammatory processes, general and local changes occur that contribute to the development of chronic inflammation of the tonsils.
The development of chronic tonsillitis is facilitated by such foci of chronic inflammation as carious teeth, periodontal disease, chronic rhinitis, sinusitis, as well as a deviated nasal septum, adenoids, hypertrophy of the turbinates, which impede nasal breathing.
When you have a runny nose, inflammatory changes in the mucous membrane occur not only in the nose, but also in the sinuses; mucus accumulates in them, and if its outflow is poor, inflammation can turn into purulent discharge. This is how acute purulent sinusitis . Depending on which sinus is affected, inflammation of the frontal sinus is distinguished - frontal sinusitis , - and the maxillary sinus - sinusitis (the name of this sinus is the maxillary sinus).
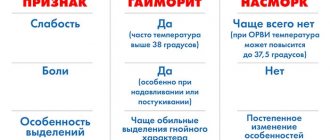
Symptoms of acute sinusitis consist of the following signs: fever, runny nose with purulent discharge, headache. The final answer about the presence and prevalence of sinusitis can be given by an X-ray of the skull; it shows which sinuses and how severely affected by the inflammatory process.
The need for mandatory treatment of sinusitis is due to the fact that the infection is prone to chronicity, and chronic sinusitis is treated much worse and takes longer than acute sinusitis. In a chronic process, there are no such acute signs of inflammation (as a rule, the temperature is normal, nasal discharge is not as abundant as in an acute one). But having a constant source of chronic inflammation in your head is like living in an apartment with a bomb. The infection can spread to neighboring parts of the skull, and in the neighborhood - the brain and eyes. So it’s not worth the risk, you definitely need to get treatment.
A runny nose, or rhinitis , is an inflammation of the nasal mucosa. There are acute and chronic runny nose. Acute runny nose can be an independent disease or a symptom of acute infectious diseases (influenza, measles, diphtheria, etc.).
The predisposing factor is mainly hypothermia; less commonly, mechanical or chemical irritations can be the cause. Acute runny nose is always bilateral.
Initially, there is a slight malaise, a feeling of dryness in the nasopharynx, and itching in the nose. Nasal breathing is difficult, sneezing and lacrimation appear, the sense of smell decreases, the timbre of the voice changes, and copious liquid discharge from the nose is observed. Subsequently, the discharge becomes mucopurulent, and if small blood vessels are damaged, it becomes bloody. Inflammation of the nasal mucosa can spread to other parts of the respiratory tract, as well as to the paranasal sinuses, nasolacrimal canal, auditory tube, and tympanic cavity. If the course is favorable, after 12-14 days, nasal congestion disappears and the sense of smell is restored.
The causes of chronic runny nose are prolonged or recurring acute runny nose; prolonged exposure to various irritants - chemical, thermal, mechanical; irritation of the nasal mucosa with purulent secretions in diseases of the paranasal sinuses; long-term circulatory disorder in the nasal mucosa (heart defects, myocarditis, nephritis, emphysema, bronchiectasis, endocrine diseases).
With a chronic runny nose, there is periodic nasal congestion and copious mucous discharge. Patients indicate that the left half of the nose is stuffy when lying on the left side, the right half is blocked when lying on the right side, nasal breathing is difficult when lying on the back. The general condition is usually not affected.
Allergic rhinitis is also distinguished. The slightest irritation of the nerve endings of the nasal cavity (cooling, pungent odor, etc.) leads to a violent reaction of the nasal mucosa. In case of seasonal runny nose, the irritant may be cereal pollen. In the year-round form, the irritants are the so-called household allergens (cosmetics, house dust, hair and dander of pets, etc.). Symptoms of allergic rhinitis occur suddenly, nasal congestion appears with copious watery mucous discharge and sneezing.
Laryngitis, pharyngitis and tracheitis - treatment features
Laryngitis and tracheitis are diseases of the upper respiratory tract. Very often these diseases accompany each other, go “hand in hand”. The reason for this “friendship” is as follows.
Laryngitis is an inflammation of the mucous membrane of the larynx, and tracheitis is an inflammation of the mucous membrane of the trachea. Very often these diseases occur for the same reason.
And since the larynx and trachea are connected to each other, inflammation of one organ logically leads to inflammation of the other.
Sometimes their team is also accompanied by pharyngitis - inflammation of the back wall of the pharynx and uvula. What are the causes of laryngitis, tracheitis and pharyngitis?
Common causes of rhinitis, laryngitis, tracheitis, pharyngitis.
For diseases to be “neglected”, one of the reasons listed below is sufficient.
- Viral infection. If we talk about the infectious nature of diseases, then 90% of cases are viral infections (influenza, parainfluenza, adenoviral infection, etc.).
- Bacterial infection. Much less often, diseases are caused by bacteria (staphylococci, streptococci, etc.).
- Inhaling cold air. With the onset of the off-season, this reason quite often provokes diseases of the upper respiratory tract.
- Inhalation of polluted air (dust, exhaust gases, industrial emissions, etc.)
- Allergens. In some cases, if the patient is allergic to a component present in the air (pollen, chemical elements, animal hair, etc.), diseases may develop.
- Mechanical injuries of the respiratory system.
- Bad habits, in particular smoking.
Laryngitis, tracheitis, pharyngitis also have their own “individual” causes:
- laryngitis: severe stress on the vocal cords;
- tracheitis: cardiac or pulmonary pathology, as well as diseases of the gastrointestinal tract (heartburn);
- pharyngitis: caries, sinusitis, sometimes heredity.
The mechanism of development of the disease is as follows.
An external irritant enters one of the organs and begins to act on the mucous membrane of the pharynx, larynx or trachea.
Swelling of the pharyngeal mucosa appears, it turns red and pharyngitis develops.
If the mucous membrane of the larynx becomes irritated and swelling of the vocal cords occurs, then we are talking about laryngitis.
Inflammation of the tracheal mucosa provokes the development of tracheitis. Although the causes of laryngitis, tracheitis, and pharyngitis are similar, the symptoms of these diseases differ.
Symptoms of laryngitis
- Hoarseness of voice. The vocal cords swell and the voice becomes hoarse or disappears altogether.
- Dry, barking cough that gets worse with a deep breath.
- Soreness and pain in the throat, sensation of the presence of a foreign body in the larynx.
- Temperature.
- Headache.
Symptoms of tracheitis
- Dry, difficult cough, especially at night and in the morning.
- Pain behind the sternum.
- Difficult to separate sputum.
- Fever.
- General weakness.
Symptoms of pharyngitis
- Redness of the back wall of the pharynx, uvula.
- Sore throat and sore throat when swallowing.
- Dry cough.
- Temperature increase.
- Enlarged and painful lymph nodes in the submandibular and occipital parts.
What are the dangers of diseases?
Pharyngitis itself is not dangerous. However, if it is not treated properly, it can develop into serious complications, especially if streptococcal pharyngitis occurs.
In this case, complications can be purulent or non-purulent.
- Purulent: An abscess can form around the tonsils (peritonsillar abscess) or in the retropharyngeal space (retropharyngeal abscess).
- Non-purulent: serious complications in the kidneys (post-streptococcal glomerulonephritis) or rheumatism.
- Transition of pharyngitis into a chronic form (granular pharyngitis).
Laryngitis poses the following dangers.
- Suffocation. As described above, with this disease the vocal cords swell, which causes hoarseness. Sometimes the swelling of the ligaments can be so severe that it becomes difficult for air to enter the lungs. Laryngitis is especially dangerous for children under 2-3 years of age, because The passage of the larynx is still small and it becomes difficult for the baby to breathe.
- The transition of the disease to a chronic form, against the background of which much more dangerous diseases can develop (fibroids, cysts, polyps, laryngeal cancer).
- Inappropriate treatment of laryngitis is fraught with the appearance of various complications: neck phlegmon, lung abscess, sepsis.
Tracheitis is also particularly harmless, but this does not mean that the patient should ignore treatment. Because he makes secret threats.
- Tracheitis can acquire a recurrent form, when it occurs several times a year, and then develop into a chronic form.
- Inflammation of the trachea can also affect the lower respiratory tract. And this is already: bronchitis, pneumonia, emphysema and even bronchial asthma.
So, treatment of laryngitis, pharyngitis and tracheitis is a must!
Therapy for three diseases
Treatment of these diseases is aimed at eliminating the causes of their occurrence, as well as suppressing the symptoms of the diseases.
Eliminating the causes of upper respiratory tract diseases
- It is necessary to give up the bad habit of smoking.
- Breathe clean air.
- Eliminate allergens that cause illness
- Fighting viral infection. For this, the following drugs are used: Groprinosin, Amizon, Isoprinosine, etc. Drugs such as Tsitovir 3, Kagocel also have immunomodulatory properties, i.e. they also strengthen the patient’s immunity, which contributes to a faster recovery.
- Bacterial infection, although much less likely to cause laryngitis, tracheitis and pharyngitis, is fraught with much more serious threats. Therefore, treatment in this case involves various antibiotics, otherwise the bacterial infection will certainly cause serious complications.
Many patients, knowing what side effects antibiotics have on the body, try to stop taking them as quickly as possible, and at the first signs of recovery they put them aside.
However, it is very important to take the full course of antibiotics, even if relief occurs within a couple of days. There is a logical explanation for this:
- Antibiotics have their maximum effect only after reaching the required concentration in the body;
- Antibiotics do not instantly destroy harmful agents;
- If you stop using antibiotics before completing the course of therapy, the bacteria will develop resistance to them and the next time you get sick, these antibiotics will simply be useless.
So, when antibiotics still have to be used in treatment, let’s consider which drugs are most often and successfully used:
- pharyngitis is treated with Amoxicillin, Clindomycin, Lincomycin, Erythromycin;
- for laryngitis, antibiotics of different groups are prescribed: Amoxicillin, Augmentin, Ceftoxime, Azithromycin.
- It is believed that treatment of tracheitis is most effective with penicillin antibiotics: Flemoxin solutab, Amoxiclav, Augmentin.
It is also worth noting that in the treatment of all three diseases, topical antibiotics, for example Bioparox in the form of inhalations, give good results.
All antibiotics and their dosages should be prescribed only by a qualified ENT specialist!
What is prescribed to treat symptoms?
Laryngitis, tracheitis and pharyngitis have one common symptom - cough. In all three cases, the cough is dry, and sputum is difficult to separate.
Therefore, expectorants are prescribed: Ambroxol, Lazolvan, Gerbion. For severe and difficult coughs, antitussive drugs are prescribed, which are usually taken at night: Sinekod, Bronholitin, etc.
Cough treatment is very effective using inhalation through a nebulizer.
The following medications are used for this: Chlorophyllipt, Lazolvan, ACC, alkaline solutions.
Pain and sore throat are treated with antiseptics and local antimicrobials: Ingalipt, Hexoral, Strepsils, Lugol, Travisil, etc.
If the disease is of an allergic nature, in addition to the fact that the allergen must be eliminated, antihistamines are prescribed: Suprastin, Cetrin, etc. At elevated body temperatures, antipyretics are prescribed: Paracetamol, Ibuprofen, etc.
Important! Treatment, medications and their dosages are prescribed only by a doctor!
For a speedy recovery, basic treatment can be successfully supplemented with folk remedies, as well as strengthening the immune system.
To do this, you need to lead a healthy lifestyle, give up bad habits, follow diets, eat fresh vegetables and fruits, and spend a lot of time outdoors.
And then any disease will recede. Listen to our advice and be healthy!
Rhinitis and pharyngitis symptoms and treatment
Treatment of nasopharyngitis
As the name suggests, nasopharyngitis is a combination of two very unpleasant diseases: rhinitis and pharyngitis (we have already written about its common and different features with laryngitis). Therefore, the treatment of nasopharyngitis is inextricably linked with the treatment of each of these two diseases. Because if any of them is not cured completely, there is a danger that nasopharyngitis will go into a chronic stage, which is difficult to treat.
But before we move on to considering the issue of treating rhinopharyngitis, it is necessary to briefly recall what rhinitis itself is and what pharyngitis is.
What is rhinitis?
It is very simple to answer the question: “What is rhinitis?” Rhinitis is simply a runny nose, or inflammation of the nasal mucosa. In its development, rhinitis goes through several stages, which are characterized by certain symptoms.
Stage 1 – symptoms of rhinitis: sneezing, aching, slight increase in temperature, coughing, sore throat, headache.
Stage 2 – symptoms of rhinitis: liquid discharge from the nose, constantly, almost without interruption, slightly elevated temperature, unclear head, stuffy nose.
Stage 3 – symptoms of rhinitis: thick nasal discharge, nasal congestion.
Usually, if there are no complications, rhinitis goes away within 7 to 10 days.
What is pharyngitis?
Pharyngitis is an inflammation of the mucous membrane of the pharynx. It usually happens after viral diseases, such as acute respiratory infections, acute respiratory viral infections, etc. But sometimes it is caused by bacteria, as with a sore throat.
Symptoms of pharyngitis are: cough, sore throat, constant sore throat.
What is rhinopharyngitis?
Imagine the situation: after a poorly treated runny nose (rhinitis), you suddenly felt a sore throat, and then severe pain in this area. The temperature rises, the ears may become blocked, as if wax plugs have formed in them. It hurts to swallow, and my nose is running again.
This combination will be called nasopharyngitis. And most often, the appearance of a runny nose will be inextricably linked with the appearance of pain in the pharynx area. Because mucus, entering the pharynx area, causes a painful reaction in this area. Redness of the pharynx is observed, and sometimes ulcers appear.
Symptoms of nasopharyngitis
Symptoms of nasopharyngitis are a mixture of symptoms of rhinitis and pharyngitis:
The first 1-2 days: nasal congestion, slight fever, lethargy, weakness, weakness, sore throat, sneezing, buzzing or pain in the head, pain when swallowing.
Then 2-4 days of heavy runny discharge from the nose, cough, slight fever, lack of appetite, difficulty breathing, stuffy nose and ears, sore throat.
Remaining time of illness: gradual transition of nasal discharge into a thick form, until complete disappearance, gradual relief of inflammation of the nasopharynx, residual congestion in the nose and ears, gradual disappearance of cough.
Treatment of nasopharyngitis
Treatment of nasopharyngitis is a combined process of treating the nasopharynx completely, i.e. and the nasal area (runny nose) and the pharynx area (sore throat).
Because Rhinopharyngitis is not a cold in the generally accepted sense, then simply warming up the body with foot baths and mustard plasters will not help.
The most important thing to do with rhinopharyngitis is to free the nasal area from the mucus that constantly accumulates there during illness. Getting rid of mucus in the nose is simply necessary because this mucus flows down the back wall of the pharynx, causing inflammation in the pharynx area - pharyngitis. Therefore, it turns out that by freeing the nose from mucus, we thereby get rid of the cause of pharyngitis.
How to get rid of mucus? All kinds of nasopharyngeal rinsing, inhalation, and warming help very well with this. Oil drops in the nose or nasal sprays, such as Rinonorm, work very well. For the pharynx, we can recommend gargling with decoctions of sage, chamomile, and furatsilin. You can also use inhalation.
In general, any remedy that leads to a gradual reduction and disappearance of mucus in the nose (rhinitis) will, accordingly, lead to relief from pharyngitis. But not vice versa, because It is rhinitis that is responsible for sore throat in nasopharyngitis. Therefore, it is precisely to get rid of rhinitis (runny nose) that the main attention and treatment should be directed.
Rhinopharyngitis, as a disease of the entire nasopharynx, requires treatment of both the nose and throat. But in order to accurately determine the causes of the disease, it is advisable not to self-medicate, but to undergo examination by a specialist, an otolaryngologist (ENT). In this case, you will receive all the necessary recommendations on how to cure a sore throat as soon as possible, and most importantly, how to ensure that nasopharyngitis does not become chronic.
Treatment of pharyngitis and laryngitis.
Treatment with pharmaceuticals
You can resort to using the following drugs:
- Collargol drops will help get rid of a runny nose. There are solutions for adults and for children, 5% and 2%, respectively. They are used up to three to four times a day. You can drop 3 to 5 drops into one nostril at a time. You can also instill "Protargol";
- Lapis solution 0.25%. It is instilled for several days using the same system to relieve inflammation, if any. Otherwise, it may not be used;
- When the temperature rises, antipyretic and antibacterial agents are prescribed. It is better to find out what exactly to take from your doctor, since he will select a remedy that suits the individual case and prescribe the correct dosage. This is especially important if you are allergic to medications.
Treatment with traditional medicine
Traditional medicine suggests using the following remedies:
- Freshly squeezed beet juice. Using it as drops will perfectly help relieve inflammation of the nasopharynx. It should be used, like a medicine, three times a day, five drops;
- Kalanchoe juice. Also serves to relieve inflammatory processes. It is sold in a pharmacy and used as regular drops;
Herbal decoction. If the disease is accompanied by a symptom such as excessive sputum, then treatment with a decoction of several herbs - coltsfoot, licorice, eucalyptus and elecampane - will help. They are mixed in a ratio of 2:2:1:1. Pour 250 ml of boiling water over a tablespoon of the resulting mixture and leave for 10-15 minutes. The strained solution is used three times a day, half a glass. Sometimes in pharmacies you can find a ready-made mixture, packaged like tea for ease of use.
General treatment
Whatever treatment method you choose, there are a list of tips that you should follow to not only reduce the symptoms of the disease, but also promote faster healing.
Warming the soles of your feet will help clear your airways and make breathing easier.
Warming the nose will facilitate the easier flow of mucus, which will prevent microscopic ruptures of blood vessels.
Bed rest for up to 4 days and plenty of drinking are required - up to 3 liters for adults and about 2 liters for children.
Effective prevention of throat and nose diseases.
The initial appearance or exacerbation of each of these diseases is possible in people of any age and at almost any time of the year. All of the above diseases can be prevented if you follow these simple recommendations:
- Maintain hand hygiene.
- Avoid hypothermia. In the cold season, try to close your throat, breathe through your nose, not your mouth .
- Monitor the cleanliness of the room and the air in it.
- Avoid exposure to any aggressive proteins (allergens).
- Check the cleanliness of filters in air conditioners and humidifiers installed in residential premises.
- Increase overall immunity.
- Follow the general rules of diet in your diet.
- During periods of exacerbation of diseases, try to avoid contact with carriers of diseases as much as possible . If you have to visit crowded places, then you need to use a gauze bandage in public places.
- At the first suspicion of pharyngitis, laryngitis or tonsillitis, you should consult a doctor.
It should be remembered that incorrect diagnosis leads to incorrect treatment. The consequence of this is complications, which will then take a long time to get rid of.
Good health and well-being to you and your family!
Otorhinolaryngologist
Doctor of the highest qualification category A.V. Sokolyansky.
How to treat nasopharyngitis?
Considering the main symptom of nasopharyngitis, treatment is almost always accompanied by the use of vasoconstrictor drops or sprays that relieve swelling and normalize nasal breathing. These drugs contain mainly oxymetazoline, phenylephrine, naphazoline or xylometazoline as active substances - Galazolin, Nazik, Snoop, Xilen, Sanorin, Tizin, Nazivin, DLYANOS, Babyfrin, etc. Depending on the dosage, the drugs can be used for the treatment of acute nasopharyngitis in children and adults.
If the disease is caused by a viral infection, it is recommended to use interferon-based nasal agents - Nazoferon, Grippferon, Genferon light. The drug based on the natural components of ARVI Active has an immunostimulating and indirect local antiviral effect.
If the disease is bacterial in nature, the doctor prescribes antibacterial drugs for nasopharyngitis, taking into account the type of pathogen and its sensitivity to the antibiotic.
If rhinorrhea is caused by allergies, antihistamines such as loratadine, suprastin, fexofenadine, levocetirizine or cetirizine are required.
To eliminate pain and sore throat, antiseptic medications for nasopharyngitis are used - Ingalipt, Grammidin, Agisept, Strepsils.
Traditional treatment
Treatment with folk remedies will help improve your condition and maintain your health.
- Using a humidifier. To thin out secretions, it is recommended to humidify the surrounding air and maintain the room temperature to 19 degrees.
- Inhalation of eucalyptus essential oils.
It is necessary to do inhalations so that it has a decongestant effect, helping to clear a stuffy nose. Essential oils can also be used in chest massage. But remember that treating colds with essential oils is contraindicated for children, pregnant or lactating women, patients with asthma or epilepsy. Consult your doctor before use. - Elder. Has antipyretic and anti-edematous effects. This plant can be used as an herbal tea (let steep for at least 10 minutes) or as a gargle (with cooled herbal tea) several times a day.
- Chamomile. For children, a runny nose can be very uncomfortable because it prevents them from breathing, causing them to be irritable and may lose their appetite. In these cases, it is best to resort to homemade solutions prepared with the addition of salt or chamomile.
Rhinopharyngitis can be treated well with folk remedies if you follow the above steps and know how to treat it.
Complications
If acute nasopharyngitis is not treated, it can become chronic.
There is also a risk of developing the following complications:
- addition of a bacterial infection;
- laryngitis;
- sinusitis;
- sinusitis;
- tracheitis;
- inflammation of the middle ear (which can lead to hearing loss);
- bronchitis;
- pneumonia.
Respiratory infections can cause exacerbation of existing chronic diseases, such as bronchial asthma.
Diagnosis of tracheitis
It is important to be able to distinguish inflammation in the trachea from diseases with similar symptoms: whooping cough, bronchitis, pneumonia, diphtheria, false croup, tuberculosis, lung cancer. A foreign body stuck in the larynx can also give similar symptoms.
Therefore, wait-and-see tactics or self-medication with folk remedies for tracheitis is unacceptable!
In case of a prolonged severe cough, it is necessary to consult a therapist, who, during the first examination, will listen to the chest with a phonendoscope, assess breathing, the condition of the mucous membranes, and collect an anamnesis (patient complaints).
Further diagnosis of the disease may require consultation with an otolaryngologist or pulmonologist, as well as comprehensive instrumental and laboratory testing.
:
- laryngotracheoscopy – examination of the larynx using special instruments;
- tracheobronchoscopy - examination of the bronchi and trachea with an endoscope to detect swelling of the mucous membrane, its thickening;
- general blood and urine analysis - to identify the inflammatory process;
- swabs from the throat and nose - to determine the causative agents of the disease;
- in some cases - x-ray.
If you suspect the allergic nature of the disease, appropriate tests will be required with consultation from an allergist.