Radiation therapy is one of the leading methods of antitumor treatment, based on the use of ionizing radiation. It can be used as an independent type of therapy, or as part of a combined/complex treatment (together with other methods), as radical, neo- and adjuvant, consolidative, preventive and palliative therapy.
- Types of radiation therapy
- Stages of radiation therapy
- Side effects of radiation therapy
- Chemoradiation therapy
The effectiveness of this method is based on DNA damage. There are various mechanisms that make it possible to more effectively destroy tumor cells compared to normal ones. Firstly, tumor cells divide more actively; accordingly, their DNA is more often in the “working” mode, when it is less resistant to the effects of ionizing radiation. For the same reason, most acute radiation reactions are represented by mucositis, that is, inflammation of the mucous membranes, which are also characterized by active division. Secondly, the surrounding healthy cells contribute to the restoration of damaged ones exposed to radiation. Therefore, it is important to ensure that as little healthy tissue as possible is included in the irradiation volume. Thirdly, modern equipment for radiation therapy, controlled by a team of competent specialists, makes it possible to deliver the highest possible doses directly to the target, significantly reducing the dose of ionizing radiation to surrounding healthy organs and tissues.
Types of radiation therapy
For several decades now, humanity has been studying the effects of ionizing radiation on the human body. At the same time, attention is focused on both the positive and negative effects that arise from its use. New methods are being developed that make it possible to achieve maximum therapeutic effect while reducing the negative effect on the body. Equipment for radiation therapy is being improved, and new radiation technologies are emerging.
Now the classification of radiation therapy methods is quite extensive. We will focus only on the most common methods.
Contact radiotherapy
In contact radiation therapy, the radiation source is introduced directly into the tumor or adjacent to its surface. This allows targeted irradiation of the tumor with minimal impact on the surrounding tissue.
Contact types of radiation therapy include:
- Application radiation therapy. It is used in the treatment of superficial tumors, for example, neoplasms of the skin and mucous membranes of the genitals. In this case, individually made applicators are used, which are applied directly to the surface of the tumor.
- Intracavitary radiation therapy. A source of ionizing radiation is introduced into the lumen of a hollow organ, for example, into the esophagus, bladder, rectum, uterine cavity or vagina. For irradiation, special applicators are used (they are called endostats), which are filled with radionuclides.
- Interstitial irradiation. A source of ionizing radiation is introduced directly into the tumor tissue. For this purpose, introstats are used, which can take the form of needles, balls, tubes filled with a radiation source.
In addition, there is a type of treatment called radionuclide therapy. In this case, open sources of radiation are used in the form of solutions of radionuclides (radiopharmaceuticals - radiopharmaceuticals), which, when entering the body, specifically accumulate in tumor foci and destroy them. Most often, radiopharmaceuticals are administered intravenously. The most widespread types of radionuclide therapy are:
- Radioactive iodine therapy. Used to treat a number of thyroid cancers because iodine selectively accumulates in thyroid tissue.
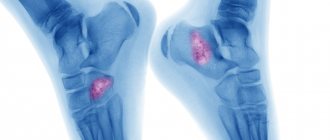
- The use of osteotropic radiopharmaceuticals is used to treat bone metastases or bone tumors.
- Radioimmunotherapy - radionuclides are attached to monoclonal antibodies to achieve targeted effects on tumor tissue.
External beam radiotherapy
With external beam radiation therapy, the radiation source is located at a distance from the patient’s body, while healthy tissues may lie in its path, which are also exposed to radiation during the therapy, which leads to the development of complications of varying severity. To minimize them, various technologies are being developed to concentrate the maximum dose of ionizing radiation directly on the target (tumor). For this purpose the following are used:
- Short focus X-ray therapy. During irradiation, X-ray radiation of low and medium power is used, which is capable of penetrating tissue to a depth of 12 mm. The method is so named because the source is located at a short distance from the irradiated surface. In this way, shallow tumors of the skin, vulva, conjunctiva and eyelids, and oral cavity are treated.
- Gamma therapy. This type of radiation has greater penetrating power, so it can be used to treat deeper tumors than X-ray therapy. However, the continued high load on surrounding organs and tissues limits the possibility of using this method in modern oncology.
- Photon therapy. It is this type of radiation that is used to treat most cancer patients in the modern world. Sufficiently high penetrating ability in combination with high-tech methods of dose delivery (IMRT and VMAT), fairly advanced planning systems make it possible to very effectively use this type of radiation to treat patients with acceptable toxicity indicators.
- Application of corpuscular radiation (electrons, protons, neutrons). These elementary nuclear particles are produced in cyclotrons or linear accelerators. Electron radiation is used to treat shallow tumors. Great hopes are placed on proton therapy, with the help of which it is possible to deliver high doses of radiation as precisely as possible to deep-lying tumors with minimal damage to healthy tissue due to the release of a radiation dose at a certain distance of the particle path, but so far these types of radiation play a relatively small role in the treatment of cancer due to its high cost and a number of not fully resolved technological aspects of implementing the method.
Stages of radiation therapy
The entire process of radiation therapy is divided into three stages:
- Pre-radiation preparation (CT simulation), the stage of selecting irradiation volumes and critical structures, the stage of dosimetric planning, verification of the radiation therapy plan.
- Irradiation stage.
- Post-radiation stage.
Planning stage
Typically, the planning stage takes several days. At this time, additional studies are carried out to enable the doctor to more accurately assess the boundaries of the tumor, as well as the condition of the tissues surrounding it. This may affect the choice of the type of radiation therapy, fractionation regimen, single and total focal doses. The basis of this stage is the implementation of the so-called CT simulation, that is, computed tomography of the required volume with certain parameters and in a certain position of the patient’s body. During the CT simulation, special marks are applied to the patient's skin and/or individual fixation devices to help position the patient correctly in the future, as well as to facilitate navigation during radiation sessions.
Then the radiotherapist draws the volumes of radiation and critical structures (those for which dose restrictions will be prescribed) on the obtained CT slices, taking into account data from other diagnostic modalities (MRI, PET). Next, a task is formed for the medical physicist, including determining the doses that should be delivered to the target, targets or its individual parts, as well as those that should not be exceeded in the volume of healthy organs and tissues. The medical physicist develops a dosimetric plan in accordance with the specified parameters, subject to which and successful verification of this plan on a phantom, the patient can be considered ready for radiation therapy.
At the stage of preparation for radiation therapy, the patient is recommended to adhere to several rules:
- Avoid products that irritate the skin.
- If there are lesions or rashes on the skin at the site of exposure, you should consult a doctor.
- If radiation therapy is expected in the maxillofacial area, sanitation of the oral cavity is required.
- Avoid sunbathing.
- The main rule at any stage: discuss all the nuances of the upcoming preparation and treatment with the attending radiotherapist and strictly adhere to the recommendations received!
Irradiation stage
The radiation stage will depend on the chosen method of radiation therapy.
External beam radiotherapy
The duration of the course of external beam radiotherapy depends on the selected fractionation regimen, as well as the purpose of treatment. Palliative courses, as a rule, are shorter than neoadjuvant and adjuvant ones, and those, in turn, are shorter than radical ones. However, it is possible to administer a radical dose in one or several sessions, depending on the clinical situation. In this case, the course of external beam radiation therapy is called stereotactic radiotherapy or radiosurgery. The frequency of sessions per day and per week also varies: schemes with five sessions per week are most often used, but 2-3 sessions per day (hyperfractionation) and schemes with 1-4 and 6 sessions per week can be offered.
During irradiation, the patient in the vast majority of cases lies down on a table in a special installation. It is absolutely necessary to remain completely still during the radiation session. To achieve this, special fixation devices and immobilization systems can be used.
Before turning on the installation, the medical staff leaves the room, and further observation is carried out through monitors or a window. Communication with the patient is carried out via speakerphone. During the session, parts of the apparatus and the table with the patient move along a given trajectory. This can create noise and anxiety for the patient. However, you should not be afraid of this, since the entire procedure is controlled.
The radiation therapy session itself can last 5-10 or 60-120 minutes, more often 15-30 minutes. The exposure to ionizing radiation itself does not cause any physical sensations. However, if the patient’s well-being worsens during the session (severe pain, cramps, nausea, panic), the medical staff should be called in a pre-agreed manner; the installation will be turned off immediately and the necessary assistance will be provided.
Contact radiation therapy (brachytherapy)
Brachytherapy is carried out in several stages:
- Introduction into the irradiated area of inactive conductors - devices into which a source of ionizing radiation is then implanted. Intracavitary radiation therapy uses devices called endostats. They are installed directly into the cavity of the irradiated organ and next to it. Interstitial radiation therapy uses introstats, which are installed directly into the tumor tissue according to a pre-calculated scheme. To control their installation, as a rule, X-ray images are used.
- Moving the radiation source from storage to intro- and endostats, which will irradiate tumor tissue. The exposure time and patient behavior will depend on the type of brachytherapy and the equipment used. For example, with interstitial therapy, after installing a source of ionizing radiation, the patient can leave the clinic and come for a repeat procedure after a recommended period of time. Throughout this period, his body will contain an introstat with radionuclides that will irradiate the tumor.
The delivery of intracavitary brachytherapy will depend on the units used, which are of two types:
- Low dose rate settings. In this case, one irradiation session lasts about 2 days. Endostats are implanted under anesthesia. After checking the correctness of their installation and the introduction of radionuclides, the patient is transferred to a special room, where he will have to stay the entire time the procedure lasts, observing strict bed rest. You are only allowed to turn slightly on your side. Standing up is strictly prohibited.
- High dose rate settings. The irradiation time is several minutes. Anesthesia is not required for the installation of endostats. But during the procedure you still need to lie absolutely still. Intracavitary radiation therapy with a high-power unit is carried out in several sessions at intervals from one day to one week.
Radionuclide therapy
During radionuclide therapy, the patient takes radiopharmaceuticals orally in the form of a liquid solution, capsules, or injections. After this, he is placed in a special room with isolated sewerage and ventilation. After a certain period, when the dose rate decreases to an acceptable level, radiological monitoring is carried out, the patient takes a shower and changes into clean clothes. To monitor the results of treatment, scintigraphy is performed, after which you can leave the clinic.
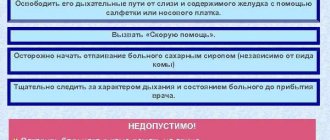
How to behave during radiation therapy
Radiation therapy is a serious stressor for the body. Many patients feel worse during this period. To minimize it, it is recommended to adhere to the following rules:
- Get more rest. Minimize physical and mental stress. Go to bed when you feel the need, even if it arises during the day.
- Try to eat a balanced and nutritious diet.
- Give up bad habits during therapy.
- Avoid tight, tight clothing that could injure your skin.
- Monitor the condition of the skin at the irradiation site. Do not rub or comb it, use hygiene products recommended by your doctor.
- Protect your skin from sun exposure by wearing wide-brimmed clothing and hats.
Diet
To prevent the occurrence of a general reaction or eliminate its manifestations, it is necessary to consume foods rich in microelements and vitamins, and drink at least 2 liters of fluid per day. These tips apply in almost all cases, but it is advisable to first discuss them with your doctor:
- avoid using spicy, fatty, fried foods, smoked foods, marinades;
- reduce salt intake or replace table salt with mineralized salt;
- cook food using vegetable oils;
- give preference to chicken and fish;
- drink only filtered water.
It is also worth considering the characteristics of individual injuries. For example, after irradiation of the abdominal organs, loose stools, nausea, and vomiting are noted. Therefore, if you have diarrhea, it is advisable to exclude dairy products from the menu. Vegetable soups, pureed porridge, mashed potatoes, boiled fish, steamed cutlets, and jelly are very healthy.
Side effects of radiation therapy
Radiation therapy, like other methods of antitumor treatment, causes a number of complications. They can be general or local, acute or chronic.
Acute (early) side effects develop during radiotherapy and in the coming weeks after it, and late (chronic) radiation damage occurs several months and even years after its completion.
General reactions
Depressed emotional state
The vast majority of patients undergoing treatment for cancer experience anxiety, fear, emotional stress, sadness and even depression. As your general condition improves, these symptoms subside. To ease them, it is recommended to communicate more often with loved ones and take part in the lives of others. If necessary, it is recommended to consult a psychologist.
Feeling tired
The feeling of fatigue begins to increase after 2-3 weeks from the start of therapy. During this time, it is recommended to optimize your daily routine so as not to be exposed to unnecessary stress. At the same time, you can’t completely distance yourself from business so as not to fall into depression.
Blood change
If it is necessary to irradiate large areas, the bone marrow is exposed to radiation. This in turn leads to a decrease in the level of blood cells and the development of anemia, increasing the risk of bleeding and the development of infections. If the changes are severe, a break in irradiation may be required. In some cases, drugs that stimulate hematopoiesis (blood formation) may be prescribed.
Decreased appetite
Radiation therapy usually does not cause nausea or vomiting, but decreased appetite is common. At the same time, for a speedy recovery, a nutritious, high-calorie diet with a high protein content is required.
Local complications
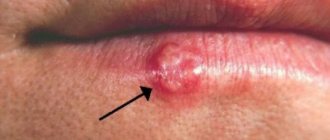
Adverse reactions from the skin
The likelihood of developing skin reactions and their intensity depend on the individual characteristics of the patient. In most cases, redness appears in the affected area after 2-3 weeks. After treatment is completed, it is replaced by pigmentation, reminiscent of a tan. To prevent excessive reactions, special creams and ointments may be prescribed and applied after the end of the session. Before starting the next one, they must be washed off with warm water. If the reaction is severe, take a break from treatment.
Reactions from the mouth and throat
If the head and neck area is irradiated, radiation stomatitis may develop, which is accompanied by pain, dry mouth, inflammation of the mucous membranes, as well as xerostomia due to dysfunction of the salivary glands. Normally, these reactions go away on their own within a month after the end of radiation therapy. Xerostomia can bother the patient for a year or more.
Breast complications
When undergoing radiation therapy for breast cancer, the following reactions and complications may occur:
- Redness of the skin of the chest.
- Breast swelling.
- Pain.
- Changes in the size and shape of the gland due to fibrosis (in some cases, these changes remain for life).
- Decreased range of motion in the shoulder joint.
- Swelling of the arm on the affected side (lymphedema).
Side effects on the chest organs
- Inflammation of the esophageal mucosa, which leads to difficulty swallowing.
- Cough.
- Sputum formation.
- Dyspnea.
The latter symptoms may indicate the development of radiation pneumonitis, so if they occur, you should immediately contact your doctor.
Adverse reactions from the rectum/intestinal loops
- Stool disorder - diarrhea or vice versa, constipation.
- Pain.
- Bloody discharge from the anus.
Side effects from the bladder
- Frequent, painful urination.
- The presence of blood in the urine can sometimes be so pronounced that the urine becomes blood-red in color.
- The presence of pathological impurities in the urine - crystals, flakes, purulent discharge, mucus.
- Reduced bladder capacity.
- Urinary incontinence.
- Development of vesicovaginal or vesicorectal fistulas.
Side effects when irradiating tumors of the retroperitoneum, liver, pancreas
- Nausea and vomiting.
- Chills after sessions.
- Epigastric pain.
Make an appointment
Sign up for onco by number. Consultation with an oncologist takes place by calling in advance. The cost is presented on our website. In our clinic you can take any tests, undergo the necessary examinations with a detailed interpretation of the results and the prescription of effective treatment. We use the most effective methods according to international standards.
Our specialists have many years of experience in the medical practice of treating oncology. We work not only on weekdays, but also on holidays and weekends. The clinic is located in Moscow, in the Central Administrative District (CAO), near the Mayakovskaya, Belorusskaya, Novoslobodskaya, Tverskaya, and Chekhovskaya metro stations.
Chemoradiation therapy
Radiation therapy is rarely performed as a stand-alone treatment. Most often it is combined with some other type of treatment: surgical, and most often with medication. This can be either the option of simultaneous or sequential chemoradiotherapy, as well as options for combining radiation therapy with immunotherapy, targeted and hormonal therapy. Such types of treatment may have significantly higher antitumor efficacy, however, the risks of joint side effects must be carefully assessed, so decisions on any volume of treatment for oncological pathology should be made by a multidisciplinary oncological council.
Book a consultation 24 hours a day
+7+7+78
Help with complications
Patients are prescribed consultations with relevant specialists, who, after examination, prescribe hematopoietic stimulants, anti-inflammatory, absorbable drugs according to indications, taking into account age and general condition. Therapy is aimed at alleviating symptoms and should be comprehensive.
In cases of tumor recurrence, the question arises about the need for an additional course of radiation. This is most often done for palliative (maintenance) purposes using low doses. Such an attempt usually ends in weak destruction of cancer cells and the formation of a trophic ulcer. Repeated palliative radiation does not provide any guarantee of success.