Cancer is contagious
Recently, the media have been actively refuting this myth. But for a long time it was believed that cancer is a contagious disease, i.e. A cancer patient can transmit the tumor to another person.
Any infectious process includes three main components:
- the causative agent of the disease (usually some kind of microorganism, virus, etc.);
- transmission route - the path of the pathogen from a sick person to a healthy person (the most common types of transmission are airborne, alimentary, contact);
- the presence of a susceptible human organism that can become ill.
With regard to cancer, none of these points is true: the causative agent of cancer does not exist as such, since the disease has completely different development mechanisms. But still, various infections and cancer have some relationship.
Some viruses increase the risk of developing certain cancers. For example, human papillomavirus, Einstein-Barr virus (a type of herpes virus), hepatitis B and C virus, herpes virus type eight, Helicobacter pylori.
However, there are vaccines—certain medications that increase resistance to these viruses. For example, the effectiveness of vaccines against hepatitis B and human papillomavirus has already been scientifically proven and substantiated.
Thus, cancer is not an infectious disease; it is absolutely not contagious.
Cancer and its types
HomePatientsAbout cancerYou need to knowCancer and its types
"Cancer"
– a collective concept, a common name for a huge group of diseases that share one common property – the processes of cell growth and reproduction (division) going out of control. During the development of a tumor, one of the body's cells changes and begins the endless process of reproducing its own kind. These cells further spread throughout the body (see below in the section “What is metastasis”). The 10 most common types of cancer are: eight affect organs, two affect the lymphatic and circulatory systems.
What types of cancer are there?
Today, more than 100 types of malignant tumors are known. As a rule, they are named after the organ from which they originate, for example, a primary tumor of the lung would be called “lung cancer”. Sometimes additional clarifications are used, depending on the specific type of tissue from which the tumor originated. For example, “squamous cell lung cancer” is a subtype of lung cancer that develops from the squamous epithelium lining the lumen of the bronchi. This can be important when choosing a treatment method.
In addition, tumors can be divided into solid (“solid”), the cells of which form a tumor mass, and tumors of the hematopoietic and lymphatic system (hemoblastosis), which initially occur as systemic diseases, i.e. involving more than one organ. For example, in leukemia, tumors originate from bone marrow cells, enter the bloodstream and circulate throughout the body with the bloodstream.
Classically, the word “cancer” refers to tumors arising from the epithelium of the skin or mucous membranes. Tumors originating from other types of tissue, such as muscles, tendons, nerves, fat, bones, etc. called "sarcomas". Malignant tumors also include:
- leukemia and multiple myeloma (primary bone marrow tumors);
- lymphomas are tumors originating from peripheral organs of the immune system, for example, lymph nodes;
- melanoma is a tumor that develops from melanocytes, special cells that normally protect the body from the harmful effects of sunlight, they also form “moles”;
- neuroendocrine and carcinoid tumors are tumors that have hormonal activity.
What is the difference between malignant and benign tumors?
It is necessary to distinguish between benign and malignant tumors; their main differences are presented in Table 1. It should be noted that in some cases benign tumors can reach significant sizes. Benign tumors, as a rule, do not pose an immediate threat to the patient's life, with the exception of tumors growing in the brain and spinal cord - these tumors can compress critical structures in these organs and lead to death or cause irreparable harm to the patient's health.
| Table 1. Main differences between malignant and benign tumors | ||
| Benign tumors | Malignant tumors | |
| Growth pattern | “Push back” surrounding tissues | Surrounding tissues grow |
| Capacity for vascular invasion | No | Yes |
| Ability to metastasize | No | Yes |
| Growth form | Regular (for example, round) | Incorrect |
| Relapses | No | Yes |
How does cancer occur and how do tumor cells differ from normal cells?
Many normal cells have the ability to divide, but these processes occur in concert and stop or slow down when the need for the formation of new cells ceases. For example, wounding the skin stimulates the acceleration of cell division processes that form the skin. Once the wound heals, the rate of cell division slows down again to the level necessary only to renew senescent cells.
As the tumor develops, everything changes. Its cells divide almost independently of external signals (autonomously); as mutations accumulate, they become less and less similar to normal ones, their previous functions are lost, and instead only one remains - reproduction. Tumor cells begin to actively absorb nutrients, grow and multiply. Over time, they begin to displace normal cells and acquire the ability for invasive growth (which means germination into other tissues and blood vessels) and metastasis (spread throughout the body through the blood, lymph, along blood vessels and nerves, and so on).
The cause of the appearance of tumor cells (oncogenesis) is the appearance of certain mutations in DNA - disturbances in the genetic code of the cell that arise under the influence of external factors (for example, carcinogenic substances, oncogenic viruses, and so on - see below) or during the process of natural cell division.
There are many mechanisms in the body that block the formation and growth of tumor cells. So, in any cell there are special controller proteins that monitor the process of its division and, if something goes wrong, they stop further reproduction of the cell and start the process of its natural death (apoptosis). The cell can receive a similar signal from the external environment, for example, from other cells of the body. In a tumor cell, the mechanisms of death when damaged are “switched off” and they do not respond to such stimuli and continue to divide.
The immune system also carries out continuous surveillance of such cells, recognizing and destroying those cells that may pose a danger to the body. However, in some cases, the tumor may acquire the ability to “deceive” the immune system and escape its influence.
With a combination of the above factors, in the absence of control over the integrity of the genetic code, the accumulation of mutations continues in the tumor, as a result of which over time it becomes less and less similar to a normal cell and acquires malignant features.
Thus, cancer is a genetic disease, which means that it occurs as a consequence of the development of damage in certain genes. These damages can be inherited from parents—modern oncology knows cases of familial cancer of the breast, ovaries, colon, and so on. However, most often they occur by chance (“sporadic mutations”) during a person’s life. Many environmental factors have a damaging effect on the cell and its genetic code, including:
- smoking;
- occupational hazards, for example, constant contact with asbestos, coal dust, a number of dyes, and so on;
- chronic infections caused by viruses, bacteria and parasites. Thus, in most cases, cervical cancer develops against the background of chronic infection caused by the human papillomavirus (HPV);
- exposure to radioactive radiation.
Be sure to tell your doctor if your relatives have had cases of developing cancer, including those that are different from yours. This can have a big impact on your treatment. Ask your family and friends if you are not sure or don’t know.
Under the influence of these and other factors, cell DNA is constantly damaged. Normally, these disorders are eliminated by special proteins that eliminate such damage (repair system). However, if critical structures are damaged, such damage can lead to malignant degeneration of the cell. Such structures include:
- Proto-oncogenes are structures that are responsible for normal cell growth and division. With certain damage, they can become hyperactive, allowing the cell to survive in conditions in which it would normally die;
- Genes that suppress tumor growth (tumor growth suppressors), like proto-oncogenes, are responsible for the processes of cell growth and reproduction, but unlike the former, they suppress these processes. When the functions of these genes are disrupted, the cell acquires the ability to grow and reproduce uncontrollably;
- Genes responsible for the normal functioning of the repair system. If they do not fulfill their tasks, mutations accumulate in the cell, which over time can lead to its malignant transformation.
What is metastasis?
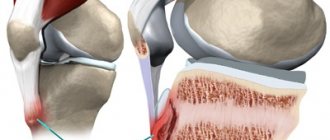
As the tumor mass grows, its cells change and genetic “damages” accumulate in them. Over time, the tumor grows into the blood and lymphatic vessels. Cells that enter the vessels are carried throughout the body through the blood or lymph flow, ending up in distant organs or nearby lymph nodes, where secondary (metastatic) tumors are formed.
This process is called the process of metastasis; it occurs differently in tumors of different localizations and depends on the characteristics of the blood supply to the tumor and some of its biological properties. For example, distant metastases of colon cancer are most often found in the liver, lungs and brain, while prostate cancer most often metastasizes to the skeletal bones. This is the most advanced stage of the tumor process (IV), which is characterized by the least favorable prognosis. However, the achievements of modern medicine in some cases make it possible to significantly prolong and improve the quality of life in patients with metastatic tumors.
Secondary tumors, as a rule, have the same histological picture as the primary lesion and similar molecular genetic disorders. It follows that metastases of rectal cancer to the liver are treated in the same way as rectal cancer itself, not like liver cancer.
Eating sugar leads to cancer
Sugar is vital for cells - both tumor and healthy ones. In the human body, healthy cells try to use sugar as efficiently as possible for energy. One gram of glucose produces 38 molecules.
but tumor cells use a different mechanism, which results in the formation of only two molecules. That is, tumor cells, compared to healthy ones, receive 19 times less energy from one gram of glucose. The most popular theory explains this fact by genetic changes in the structure of the tumor.
Yes, sugar is necessary for the human body. But its excess can lead to obesity. Excess body weight increases the risk of developing certain malignant tumors.
Thus, obese people have an increased risk of developing
- uterine cancer 7 times;
- esophageal cancer 2 times;
- colon cancer 1.3 times;
- pancreatic cancer 1.5 times;
- kidney cancer 2 times;
- breast cancer 1.3 times;
Thus, sugar itself does not cause malignant tumors, but it may increase the likelihood of some of them.
Diagnosis of cancer
Diagnosis of cancer can be based on history and examination, but requires confirmation by biopsy and histopathological examination. Sometimes the first sign is an abnormal laboratory test result (for example, anemia due to colon cancer).
A full history and physical examination may reveal unexpected signs of early cancer.
Therapists should be aware of predisposing factors and, when obtaining a medical history, pay particular attention to questions about family history of cancer, lifestyle (including smoking), and past or present medical conditions (eg, immune disorders, previous immunosuppressant therapy, hepatitis B or C, HIV infection, positive Pap test, infection with human papillomavirus). You should also pay attention to newly emerging symptoms such as constipation that cannot be corrected by diet and medications, decreased hemoglobin, weight loss, and others.
In addition to a complete history and physical examination, cancer diagnostic procedures may include one or more of the following:
- Complete blood test.
This test helps identify abnormal cells that may indicate cancer.
- Biopsy, bone marrow aspiration, or both tests.
This procedure involves taking a small amount of fluid from the bone marrow (aspiration) and/or solid bone marrow tissue (called a core biopsy), usually from the back of the hip joint, to examine various blood counts or abnormal cells.
- Lumbar puncture.
This procedure helps evaluate the fluid around the spine and brain for pressure and/or infection and looks for any abnormal cells. A special needle is placed in the lower back, in the spinal canal (the area around the spinal cord). The pressure in the spinal canal and brain can then be measured. A small amount of cerebrospinal fluid may be removed and sent for testing to determine if there is an infection or other problem.
- Lymphangiography (LAG).
This is a test that can detect cancer cells or abnormalities in the lymphatic system and structures. To do this, a special radioactive tracer dye is injected into the lymphatic system.
- Ultrasound (sonography).
This technique uses high-frequency sound waves and a computer to create images of blood vessels, tissues and organs. Ultrasound is used to view internal organs, how they function, and to evaluate blood flow through various vessels. Tumors in the stomach, liver and kidneys can often be seen using this test.
- Tumor biopsy.
This is a procedure in which a tissue sample is taken from the tumor and examined under a microscope. A biopsy is necessary for diagnosis as it provides the most accurate tissue analysis.
- Bone scan.
After injecting a radioactive dye that is absorbed by the bone tissue, a picture or x-ray of the bone is taken. These scans are used to detect tumors and bone abnormalities.
- X-ray.
These tests use invisible electromagnetic energy beams (X-rays) to produce images of internal tissue, bones, and organs on film. X-rays can be taken from any part of the body to detect a tumor (or cancer).
- CT scan.
This is a test that uses X-rays and a computer to create detailed images of the body. A CT scan shows details of bones, muscles, fat and organs.
- Positron emission tomography and CT (PET-CT).
As mentioned above, a CT scan provides detailed images of tissues and organs, while a PET scan shows any abnormal activity. A more complete picture is provided by combining these two tests.
- Magnetic resonance imaging (MRI).
MRI uses a combination of large magnets, radio frequencies and a computer to produce detailed images of organs and various structures inside the body. This test is performed without the use of X-rays.
- Blood analysis.
It is used to evaluate electrolytes, liver and kidney function, the presence of infection, and tumor markers (chemicals released by the tumor).
- Surgical diagnosis.
Surgery may be needed to perform a biopsy, remove tumors or entire organs affected by the disease, or look for tumors that may not be detected by other tests.
Frequent use of mobile phones affects the development of tumors
Why did such a myth arise? The researchers explain:
- radio waves are absorbed by biological tissues, i.e. radiation affects the cells of our body;
- the number of mobile phones is increasing every year;
- The time spent using mobile phones is increasing as communications have become more accessible, widespread and cheaper;
- the number and duration of calls increases.
The researchers had the idea to test experimentally whether the occurrence of brain tumors is really associated with the use of mobile phones.
The INTERPHONE study involved more than 5 thousand people with brain tumors. Experts collected data on the frequency of use of mobile phones by patients. It turned out that there is no cause-and-effect relationship between the occurrence of a brain tumor and the use of a mobile phone.
Leading organizations in the world such as the American Cancer Society, National Institute of Environmental Health Sciences, Food and Drug Administration (FDA), CDC (Department of Health and Human Services, USA) have expressed their opinion that mobile phones are completely safe.
Thus, the occurrence of brain tumors is not associated with the use of mobile phones; gadgets do not even increase the risk of cancer.
Liver cancer
There are primary and secondary liver cancer. Primary liver cancer is a malignant neoplasm that forms from organ cells - hepatocytes. Factors in the development of the disease are cirrhosis of the liver, chronic viral hepatitis B and C, alcohol abuse, parasitic liver infections, long-term use of anabolic steroids, consumption of aphlotokissins (contained in molds that attack grains and nuts).
Secondary liver cancer is damage to the liver by metastases from a tumor in another organ. This type of disease is more common, since metastasis of tumors to the liver is a common consequence of late diagnosis of cancer of various organs: stomach, lung, uterus, colon, prostate.
The following symptoms are typical for liver cancer:
- discomfort in the abdomen, aching pain in the right side;
- indigestion, weak appetite;
- fatigue, malaise;
- sudden weight loss.
Cancer is a death sentence
The outcome of treatment and the speed of rehabilitation of a cancer patient are influenced by various factors.
These include:
- biological type of tumor (different tumors have different prognosis),
- localization, prevalence and size of the tumor,
- presence and characteristics of concomitant diseases,
- tumor treatment methods,
- patient's age.
There is also such a thing as stages of cancer. The stage determines only survival, i.e. probability of living for a certain period of time. The higher the stage, the lower this probability.
As a rule, when treating malignant tumors, oncologists use an indicator such as five-year survival rate.
According to global data, the average five-year survival rate for major cancers (lung, breast, colon, prostate, skin cancer) is 60%. This is a fairly high figure.
Survival depends on the type of tumor. One of the lowest survival rates is observed for pancreatic cancer, and one of the highest for skin cancer (basal cell).
Thus, cancer is not always a death sentence for a person. With the development of technology, most types of cancer are curable.
Lung cancer
Unfortunately, the specialist notes, lung cancer is a fairly common cancer in Russia. It is one of the ten most common among both men and women. The main risk factor, in addition to heredity, is smoking. “Despite the measures taken by the Ministry of Health to combat this bad habit, a fairly large percentage of the population in our country still smokes, increasing their chances of getting lung cancer at least twice,” says the oncologist.
Lung cancer is divided into two subgroups: non-small cell and small cell. “The latter is considered much more dangerous, because it immediately has a greater prevalence throughout the body, that is, there is not just one tumor, but many at once. As a rule, they are small in size, but they are capable of metastasizing, even if the tumor is less than 1 cm. Because of this, surgical treatment of small cell lung cancer is usually not performed; the patient is mainly offered chemotherapy. It can slow down the development of the disease, but for a fairly limited period, because the prognosis for the course of the disease is unfavorable. The only encouraging thing here is that small cell lung cancer is three times less common than non-small cell lung cancer,” explains oncologist Glukhov.
The second type of tumor can be treated surgically, says Evgeny Glukhov. If detected in the early stages, it can have a very favorable prognosis. “But the main problem is that in the early stages it is usually not found. Even if the patient regularly undergoes fluorography, it may not show formations smaller than 2 cm in diameter. The most effective in this regard is CT, but a person who feels acceptable will not rush out of the blue to do a CT scan of the lungs every six months. But I would recommend that at least smokers undergo a CT scan periodically, taking into account their risks,” the specialist emphasizes.
Victory will be for the nano. How new cancer drugs work Read more
If there were no cases of cancer in the family, then I won’t have it either.
About 95% of malignant tumors are sporadic, i.e. they do not depend on whether blood relatives have had cancer or not.
But there are certain risk factors that increase the likelihood of developing cancer. First of all, it's age. Age is the only risk factor that we cannot influence. Risk factors also include alcohol consumption, smoking, long-term chronic inflammatory diseases and so-called carcinogenic factors.
But all of them only increase the likelihood of occurrence - nothing more, i.e. the presence of these factors will not necessarily lead to the development of a tumor in a person.
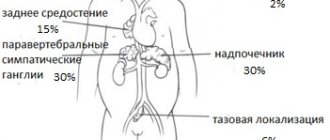
But in 5% of cases there are hereditary tumors, hereditary cancer syndromes: Cowden syndrome, Lynch syndrome, Gardner syndrome, Li-Fraumeni syndrome, multiple endocrine neoplasia syndrome and some others.
If a person has any of these inherited syndromes, then they need to undergo screening programs several years or even decades earlier than others.
Thus, only in 5% of cases can cancer be inherited, and in most cases the presence of cancer has nothing to do with heredity.
What are the symptoms of cancer?
Oncological diseases in their initial stages affect one organ. But since the affected cells have the ability to rapidly divide, the disease affects not only the functioning of a particular organ or organ system, but also the body as a whole.
General symptoms of the disease:
- deterioration of the person’s general condition – appetite decreases, the person loses weight, feels weak;
- anemia – the color of the skin changes to paler, dizziness and fainting are observed;
- immunity decreases as the body fights cancer cells, which is why it cannot resist other infections and viruses;
- pain occurs, but this symptom appears in later stages of cancer;
- in case of serious diseases, liver function is disrupted, which is why the skin may turn yellow;
- inflammatory processes that are accompanied by high temperature;
- lymph nodes enlarge, as they are responsible for cleansing the body, but this symptom can occur both on the first and second
- last stage of cancer.
Treatment for cancer is worse than the disease itself
There is a myth that living with cancer is physically easier for the patient compared to treating the tumor.
Today, three main methods of treating malignant tumors are used: surgery, chemotherapy and radiation therapy. As a rule, all three methods are used in combination.
There are many undesirable consequences of cancer treatment, including baldness, weakness, nausea, cardiotoxicity and many others.
The consequences of cancer treatment affect the quality of life, but with the availability of a wide range of medications, they are much easier to tolerate.
An oncologist has two global goals: to increase the patient’s life expectancy and to improve his quality of life. In this situation, it can be difficult to strike a balance.
Cancer patients want to know as much as possible about their diagnosis, causes, possible consequences and proposed treatment methods. Most often, patients trust the method recommended by the doctor. Experts try to minimize the negative consequences of therapy.
Thus, treatment of a malignant tumor in most cases is no worse than living with this disease.
Squamous cell carcinoma
It is less common than basal cell carcinoma, the second most common type of skin cancer, and has a slightly less favorable prognosis. However, it should be noted that the course of the disease much less malignant than that of melanoma.
Metastases occur relatively rarely - on average in 16% of cases [1]. In patients with squamous cell skin cancer less than 2 cm in size, the 5-year survival rate is about 90%; for larger sizes and tumor invasion into the underlying tissue, it is less than 50% [1].
It can occur on any part of the body, including the genitals and mucous membranes, but most often in places exposed to sunlight.
Symptoms and signs
What squamous cell skin cancer looks like depends largely on the clinical form of the disease.
The keratinizing form is a raised or flat surface covered with horny scales that can grow and fall off. If damaged, it may bleed.
Keratinizing form of squamous cell skin cancer
It must be remembered that it is the keratinizing form of squamous cell carcinoma that may be hiding under the mask of the cutaneous horn . In this regard, such formations should always be removed only with histological examination:
The cutaneous horn should be removed with histology - a keratinizing form of squamous cell carcinoma may be hidden under its mask
Non-keratinizing endophytic form (growing towards surrounding tissues). Most often it looks like a long-term non-healing wound or ulcer, which can deepen and expand over time.
Non-keratinizing endophytic form of squamous cell skin cancer
The exophytic non-keratinizing form of squamous cell skin cancer appears as a nodule that rises above the level of the skin. The surface of the node may be eroded or wet.
Exophytic nonkeratinizing form of squamous cell skin cancer
Photos in the initial stage
The initial stage of squamous cell carcinoma refers to a condition when the malignant process is limited to the epidermis - the outermost layer of the skin. It is referred to in the diagnosis as in situ or intraepidermal squamous cell carcinoma. This disease is not life-threatening if completely removed.
There are 2 forms of this phase of the disease:
Bowen's disease
Most often it is represented by single flat plaques, with clear boundaries, an asymmetrical shape, and uneven edges. The size reaches 7–8 mm. The formation may gradually increase, and peeling or crusting is often observed on the surface.
The color is red or brown, located on any part of the body. [3]
On my own behalf, I will add that in my practice, histologically confirmed Bowen’s disease occurred only once. It looked like a small (3 x 4 x 3 mm) flesh-colored lump with a smooth surface on the skin of the shaft of the penis in a 43-year-old man.
Bowen's disease
Erythroplasia Keira
The second form of early-stage skin cancer, which develops most often on the skin of the foreskin of the penis or the glans. Much less commonly, the disease affects the female external genitalia.
The most common appearance of Queyre's erythroplasia is a bright red spot with clear boundaries and a moist, shiny surface [3].
Erythroplasia Keira
Treatment of squamous cell skin cancer (NCCN, 2018)
As in the case of basal cell carcinoma, squamous cell carcinoma is divided into groups of high and low risks of recurrence and metastasis.
Area H: Facial mask (including eyelids, eyebrows, skin around eyes, nose, lips [skin and red border of lips], chin, lower jaw, skin/grooves in front and behind the auricle, temples, ears), genitals, palms and feet .
Area M: cheeks, forehead, scalp, neck and legs
Region L: trunk and limbs (excluding shins, palms, feet, nails and ankles)
Notes
- The rim of hyperemia should be taken into account when measuring size.
- Excisional biopsy is preferred over incisional biopsy.
- The modified Breslow thickness measurement should exclude parakeratosis and crusting and should be taken from the base of the ulcer, if present.
- Localization, regardless of size, may be a sign of high risk.
- Area H implies high risk regardless of size.
The basic principles and methods of treatment for squamous cell carcinoma are the same as for basal cell carcinoma.
The main goal is to maintain functionality and cosmetic qualities. method is considered to be removal of the tumor, including 4–6 mm of healthy tissue with a low risk of recurrence and metastasis. For high-risk tumors, Mohs micrographic surgery or wider excision is recommended than for low-risk tumors.
Radiation therapy is useful in cases where other methods cannot be used. Platinum drugs (cisplatin, carboplatin) as well as EGFR inhibitors (cetuximab) can be used in chemotherapy for squamous cell carcinoma.
Depression contributes to cancer
There is a misconception that negative emotions and severe depression can lead to cancer.
A study was conducted in which people with severe forms of depression took part. As a result, it was proven that the risk of developing a malignant tumor in people with depressive disorders is exactly the same as in people without such disorders.
Thus, a bad mood has absolutely no effect on the occurrence and development of a tumor and is not even a risk factor for its development.
Melanoma
Traditionally, melanoma is considered one of the most dangerous tumors, because its mortality statistics are one of the highest, says Evgeny Glukhov. However, the specialist notes that it does not occur so often - in about 4% of cases.
“In approximately 10% of patients, the disease is hereditary. The main risk factor is ultraviolet radiation. The source of this radiation does not matter - it can be artificial or natural. For example, it has already been proven that solariums are not nearly as safe as the beauty industry is trying to present. I would say that sunbathing is harmful in principle, and excessive sunbathing is already dangerous,” says the oncologist.
So you should treat your health more carefully and not subject it to tests in the form of excess sun (natural or artificial), unhealthy food and bad habits. This will minimize risks. Those who have a family history of cancer should be especially careful. If any alarming symptoms develop, you should not self-medicate and persuade yourself that it will go away on its own, it is better to undergo an examination and eliminate potential risks. After all, in the case of cancer, time is the most valuable resource, and treatment started as early as possible has a more positive effect.
Will vaccinations and a healthy lifestyle protect you from cancer? How to protect yourself from head and neck tumors Read more
GMOs cause cancer
GMO (genetically modified organism) is an organism whose genotype has been artificially changed. People have been breeding GMOs for quite a long time. One of the main methods for obtaining GMOs is selection.
At the moment, there are no studies that the consumption of GMOs leads to the development of cancer.
Thus, GMOs do not lead to the development of cancer; science has not proven otherwise.
Types of breast cancer by tumor shape
Based on the structure of neoplasms, doctors distinguish two forms:
- nodular - is an isolated malignant compaction, with a degree of hardness comparable to a stone. Sometimes it adheres to the skin or other organ structures, causing deformation of the circumference or nipple. If the tumor is formed from one node, it is unicentric, when from several - multicentric;
- diffuse - much less common than nodular. It has no clear boundaries, “spreads” throughout the entire organ, grows quickly, and metastasizes. The primary lesion enlarges, becomes covered with a network of blood vessels, and swells. The skin becomes lumpy and rough. This type is typical for young patients and may appear during pregnancy or breastfeeding.
Standing apart in the general classification is a rare, atypical form of malignant pathology - Paget's disease, in which altered cells are concentrated under the nipple. The main sign of cancer is deformation of this part of the breast (retraction, ulceration, swelling).
Other symptoms include:
- weeping, flaky areas on the areola;
- itching;
- burning;
- minor tingling sensations;
- redness of the skin over the tumor.
Experts do not have a consensus on this disease. Some doctors classify it as a precancerous condition, since cell malignancy occurs only in 3-5% of cases. The period of rebirth sometimes takes 10 years or longer. Then the damage can spread to the organ itself, the axillary lymph nodes.
People with dark skin do not get skin cancer
Statistically, skin cancer occurs more often in people with fair skin.
The main cause of skin cancer is exposure to ultraviolet rays. Protection against them is provided by melanin, which is less in people with fair skin.
A study by scientists has confirmed that skin cancer occurs in people with dark skin. But the survival rate of such dark-skinned patients is much lower than that of lighter-skinned patients. This is due to the difficulty of detection and the frequency of detection, since it is more difficult to detect a neoplasm on dark skin than on light skin.
One notable example is reggae musician Bob Marley, who died at the age of thirty-six from late-diagnosed acral melanoma, a melanoma that develops on the skin of the nails.
Thus, skin color has no effect on the risk of skin cancer, and people with dark skin can also be diagnosed with it.
Types of skin cancer
There are 3 types of common malignant skin tumors. They differ both in incidence (i.e., the chance of getting sick) and in the degree of danger to life - basal cell carcinoma, squamous cell carcinoma and melanoma.
Melanoma is one of the rare and dangerous skin tumors. It accounts for only 4% of the total number of malignant skin tumors, but is the cause of almost 80% of deaths in this localization. You can read more about melanoma here.
Sign up for the webinar “Carcinogens in cosmetics: truth, lies and... marketing”
Antiperspirant use leads to breast cancer
A study was conducted in which 813 women aged 20 to 74 years with breast cancer took part.
According to this study, the use of antiperspirants is absolutely not associated with the development of breast cancer.
Subsequently, several more studies were conducted that similarly confirmed the absence of a cause-and-effect relationship between the occurrence of breast cancer and the use of antiperspirants.
Thus, there is currently no evidence linking the use of antiperspirants and the occurrence of breast cancer.
Why does cancer appear?
Ordinary cells become cancerous due to damage to DNA
, which carries hereditary information. Typically, if DNA is damaged, special structures in the cell repair it, or the cell dies. But in cancer cells, the DNA remains damaged, but the cell continues to live and becomes immortal. In addition, it actively divides and produces new immortal cells with the same damaged DNA. The body does not need such cells, since they are not able to perform the functions originally inherent in them.
Breast implants lead to breast cancer
In fact, women who have and those who do not have implants are equally at risk for breast cancer.
But there is a very rare disease - anaplastic large cell lymphoma of the breast. This is not a disease of the breast tissue, but of the lymph nodes. And it is the presence of breast implants that influences the development of this disease.
The basic risk of developing this disease is three per 100,000,000 cases, and the risk of development in the presence of implants is already 203 per 100,000,000 cases, i.e. the risk increases by 67 times. However, the absolute incidence of this disease is extremely small.
Thus, breast implants are not associated with breast cancer, but do increase the risk of breast lymphoma.
What is cancer?
Normal cells in the body grow, divide, and die in an orderly manner.
During childhood, cells divide and grow rapidly. As a person gets older, the process of division and growth slows down and cells multiply only to repair damage and replace worn out or dying cells. Cancer Prevention
What can you do to minimize your risk of developing cancer? Find out in the material “Prevention of Oncological Diseases.”
All types of cancer begin
when cells in the body begin to grow out of control
.
Instead of dying, cancer cells continue to grow and multiply. Cancer cells, unlike normal cells, have the ability to invade other tissues
, gradually increasing the size of the tumor.
How to protect yourself from misconceptions?
In order not to succumb to common misconceptions, it is necessary to develop critical thinking.
A critical assessment of any information that comes to you can remove many contradictions and protect against misconceptions and myths in matters of health.
Good advice for doctors would be to use recommendations and methods of evidence-based medicine, which suggests relying only on scientifically proven actions that are safe for the patient’s health.
There is a certain decision-making algorithm that doctors try to follow:
- Select the question you want answered.
- Get the best evidence, the best answers.
- Critically evaluate the best answers and evidence.
- Use the information you have critically read and comprehended in relation to your clinical practice.
Also, at any stage, it is necessary to pay attention to the use of reliable sources of information.
The need to divide cancer diseases into stages
Dividing cancer into stages is necessary to solve many problems: planning treatment, determining the prognosis for the patient, since each stage has certain statistical indicators of survival, remission and the possibility of relapses in the future, monitoring the course of the disease and the effectiveness of the therapy used, ensuring continuity in the provision of care by oncologists . After all, a universal classification erases the boundaries between the different languages of the world spoken by doctors.
Who is to blame and what to do
“The main cause of melanoma is ultraviolet radiation. People who spend most of the year at home and in the office, and then go on vacation to the open sun or regularly use the services of solariums, expose themselves to great risk,” says Andrey Pylev.
You need to be very careful with the daylight. People who live in sunny countries all year round are well aware of this.
Despite the fact that the skin of the inhabitants of these regions contains more melanin, and therefore is better protected from ultraviolet radiation, most often they wear light, loose clothing that completely covers the body, a hat that protects the head and face, and use sun creams.
Many people use umbrellas. Residents of the middle zone should follow their example in this regard and not try to tan in four to five hours while being in the open sun in the middle of the day.
The cause of melanoma is a defect in the DNA molecule of the pigment cell, which ensures the storage and transmission of genetic information. If, under the influence of UV rays or other unfavorable factors, a breakdown occurs in the melanocyte, it mutates.
Melanoma can develop in anyone, but women with weakened immune systems are more susceptible to it, as well as people who have undergone organ transplants or other complex interventions in the immune system.