- Causes of pulmonary edema
- What diseases are there a risk of edema?
- Types of pathology
- Symptoms of pulmonary edema
- Diagnostics
- Treatment of pulmonary edema
- Predictions and prevention
Pulmonary edema is a condition in which gas exchange is disrupted and respiratory failure develops. Swelling occurs due to an imbalance of pressure in the pulmonary capillaries and the release of a large amount of edematous fluid into the lung tissue without its reabsorption.
Causes of pulmonary edema
A mixture of edematous fluid (transudate) and a liquid substance that “lines” the alveoli of the lungs from the inside (it is called “pulmonary surfactant”) enters the lumen of the alveoli, where it combines with air. This leads to the formation of foam, which creates an obstacle to the flow of oxygen. Lack of oxygen provokes the development of shortness of breath, due to which the pressure inside the chest decreases and blood flow to the right side of the heart increases.
Pulmonary edema causes infiltration of the alveoli and is manifested by symptoms that indicate oxygen starvation, which is dangerous for tissues. The patient requires emergency care due to the high risk of death due to suffocation.
What diseases are there a risk of edema?
Pathology indicates a complication of the underlying disease, increases its duration and worsens the prognosis of treatment. The most dangerous from the point of view of pulmonary edema include:
- Heart diseases. Respiratory failure often occurs against the background of pathologies of the heart and blood vessels. Cardiogenic pulmonary edema is a life-threatening complication that develops with myocardial infarction, aneurysm, endocarditis and myocarditis, severe hypertension, and pathological conditions caused by congenital or acquired heart defects.
- Pulmonary diseases. At risk are patients with injuries and severe diseases of the respiratory tract. Respiratory edema develops against the background of exacerbation of chronic bronchitis and bronchial asthma, tuberculosis, and lobar pneumonia. The risk is increased by tumor lesions of the lung tissue, pleurisy, and chest injuries, which are accompanied by pneumothorax. If a person is connected to a ventilator for a long time and receives a mixture with a high concentration of oxygen, this also leads to an imbalance of pressure in the pulmonary capillaries and the release of exudate.
- Infectious diseases. In severe cases or inadequate treatment of whooping cough, scarlet fever, influenza, diphtheria and other infectious diseases, edema develops, followed by acute pulmonary failure. In young children, this clinical syndrome can cause acute laryngitis and the proliferation of adenoids.
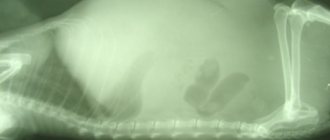
- Pathologies of intrauterine development and difficult childbirth. Severe pregnancy, prematurity, oxygen hypoxia, fetal bronchopulmonary dysplasia - these factors increase the risk of developing pulmonary failure in newborns. In pregnant women, pulmonary failure can develop due to eclampsia. The same phenomenon occurs with ovarian hyperstimulation syndrome against the background of stimulation of ovulation by hormonal drugs.
- Foreign bodies entering the respiratory tract. Mechanical asphyxia is one of the possible causes of acute respiratory failure. Pathology occurs when foreign objects enter the respiratory tract, after drowning or attempted hanging, or blockage of the respiratory tract with vomit.
- Diseases of the urinary system and gastrointestinal tract. Nephrogenic pulmonary edema can be complicated by acute inflammatory diseases, which are accompanied by renal dysfunction and the development of severe renal failure. In gastroenterology, patients with liver cirrhosis, severe pancreatitis, and intestinal obstruction have to deal with respiratory failure.
- Neurological diseases. Traumatic brain injuries, meningitis, encephalitis, neoplasms, cerebral hemorrhages, complications after brain surgery - all this leads to neurogenic pulmonary edema.
- Allergies, injuries, poisoning. Acute respiratory failure can be caused by the ingestion of various toxic substances into the body. Pulmonary edema is encountered by patients with alcohol and drug intoxication, poisoning with drugs, salts of heavy metals, and toxic gases. Pulmonary insufficiency is diagnosed in case of blood poisoning, burns with a large affected area, acute allergic reactions.
Main symptoms and causes of fluid accumulation in the lungs
The first signs that should alert you are:
- increased shortness of breath regardless of physical activity;
- intermittent cough with mucus production;
- nervous weakness with periods of increased anxiety;
- dizziness.
Predisposing factors for fluid accumulation in the lungs may be:
- Heart failure (dysfunction of the left ventricle of the heart).
- Frequent hypertensive crises, due to which blood begins to leak into the lungs through the walls of blood vessels.
- Pneumonia causes inflammation of the pleura.
- Oncological diseases of the lungs, genital area, gastrointestinal tract.
- Tuberculosis.
- Chest injuries, penetrating wounds.
- Diseases of internal organs, in which damage to the pleura is possible (for example, with cirrhosis of the liver).
© pondsaksit / Getty Images Fluid accumulation in the lungs, how to remove fluid from the lungs at home, how long does a person live with fluid in the lungs
Types of pathology
Depending on the cause of development, pulmonary edema can be cardiogenic or non-cardiogenic. In the first case, the cause of respiratory failure is cardiovascular disease. The second category includes all other pulmonary edema caused by diseases of the gastrointestinal tract, nervous system, and injuries.
Pulmonary edema is also classified according to the nature of its course. There are four types of pathology development:
- With fulminant development, severe respiratory failure occurs within a few minutes and leaves no chance of survival.
- Acute swelling can take up to four hours to develop. This form is considered less dangerous than the previous one, but in the absence of timely assistance, the risk of death is extremely high. Most often, acute pulmonary edema develops with myocardial infarction, traumatic brain injury, and acute allergic reactions.
- In case of intoxication, renal and liver failure, subacute pulmonary edema may occur. The intensity of symptoms is constantly changing, so continuous medical monitoring of the patient's condition is required.
- Prolonged swelling may take several days to develop. Symptoms are mild compared to the acute and subacute forms. Prolonged pulmonary edema usually occurs against the background of various chronic diseases, including heart failure.
Symptoms of pleurisy
The main symptoms of pulmonary pleurisy are
- pain in the chest, especially when inhaling,
- cough that does not bring relief
- dyspnea,
- feeling of tightness in the chest.
Depending on the nature of the pleural inflammation and location, these signs may be obvious or almost absent. With dry pleurisy, the patient feels pain in the side, which intensifies when coughing, breathing becomes difficult, weakness, sweating, and chills are possible. The temperature remains normal or increases slightly - no more than 37° C.
With exudative pleurisy, weakness and poor health are more pronounced. Fluid accumulates in the pleural cavity, compresses the lungs, and prevents them from expanding. The patient cannot breathe fully. Irritation of nerve receptors in the inner layers of the pleura (there are practically none in the lungs themselves) causes a symptomatic cough. In the future, shortness of breath and heaviness in the chest only intensify. The skin becomes pale. A large accumulation of fluid prevents the outflow of blood from the neck veins, they begin to bulge, which eventually becomes noticeable. The part of the chest affected by pleurisy is limited in movement.
With purulent pleurisy, noticeable temperature fluctuations are added to all the above symptoms: up to 39–40° in the evening and 36.6–37° in the morning. This indicates the need to urgently consult a doctor, since the purulent form is fraught with serious consequences.
Symptoms of pulmonary edema
Before the main symptoms of pulmonary failure appear, patients experience weakness and dizziness, a feeling of tightness in the chest, headache, and dry cough. A few hours after the first symptoms of the pathology, an attack of cardiac asthma develops - the first stage of pulmonary edema. It manifests itself:
- severe lack of air;
- severe dry cough;
- increased heart rate;
- hoarse breathing;
- profuse sweating;
- pale skin, blueness of nails and lips;
- feelings of fear and anxiety.
As a rule, the attack occurs at night or before dawn. In patients with cardiac diseases, cardiac asthma can be caused by physical or emotional stress and hypothermia.
As edema develops, the alveoli become involved in the pathological process. This leads to increased suffocation. The patient experiences severe shortness of breath, the face becomes burgundy-blue and puffy, the veins in the neck swell, and mental retardation appears. Breathing becomes hoarse, foam mixed with blood comes out of the mouth.
In the absence of medical care, the patient loses consciousness and falls into a coma. In this state, blood pressure decreases critically, breathing becomes shallow, and the pulse weakens. The cause of human death is asphyxia, in which the body experiences an acute lack of oxygen with an excess of carbon dioxide.
ethnoscience
You can treat effusion at home only if there is a small amount of it (as determined by x-ray), mild symptoms, and after consultation with your doctor. You can get rid of effusion in the lungs using folk remedies after eliminating the causative factor - the underlying disease that led to the complication.
To remove excess water, take 1 tbsp. spoons of parsley decoction: 500 g of fresh parsley pour 700 ml of milk, bring to a boil, cool. To speed up the process of removing phlegm, drink honey tincture. Compound:
- 200 g of dried or fresh viburnum berries;
- linden flowers, knotweed, plantain - 2 tbsp. spoons;
- coltsfoot - 1-3 sheets;
- vodka – 500 ml;
- honey – 50 ml.
Herbs and berries are poured with vodka, honey is added, stirred until the honey dissolves. Leave for 2 days in a dark place. Take 1 tbsp. spoons 3 times a day until sputum stops coming out. To get rid of a dry cough, stop an attack of bronchitis, and reduce the severity of inflammatory processes in the lungs, take anise decoction. Compound:
- flax seeds - 1 tbsp. l;
- boiling water – 200 ml;
- cognac – 1 tbsp. l;
- honey - 1 tbsp. l.
Pour boiling water over the seeds, cook over low heat for 10 minutes, cover with a lid to infuse for 15 minutes. Take 4 times a day, 1 tbsp. spoon. To strengthen the immune system and speed up the discharge of sputum, take onion juice once a day, 1 tbsp. l: one finely chopped onion sprinkled with 1-2 tbsp. l. sugar, after 10-15 minutes squeeze the juice through cheesecloth.
Important! Traditional methods of treatment can be combined with drug therapy.
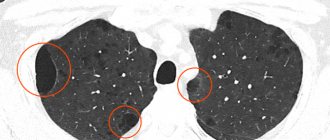
Diagnostics
A doctor can determine the development of pulmonary edema by numerous external symptoms. In addition, the patient is prescribed instrumental and laboratory examinations. Among them:
- measurement of blood oxygen levels, determination of carbon dioxide content;
- blood chemistry;
- electrocardiogram and ultrasound of the heart;
- chest x-ray to evaluate the condition of the lungs.
Inserting a catheter into the pulmonary artery allows you to determine the type of edema: cardiogenic or non-cardiogenic.
If pulmonary edema is suspected, it is important to carry out the necessary tests and examinations as soon as possible, identify the cause and type of pathology, and begin treatment. Saving the patient's life directly depends on this.
Treatment
The choice of treatment method and group of drugs depends on the causative factor. If the volume of water is more than 300 ml, pleural puncture is indicated, in which exudate is pumped out through a puncture in the chest. Groups of drugs:
- diuretics – remove excess water from the body;
- antibiotics - indicated when an infection occurs;
- bronchodilators - relieve spasm from the bronchial tree;
- immune stimulants – prescribed for viral infections;
- defoamers - to reduce the amount of foam in sputum;
- antitussive, expectorant - for dry, wet cough;
- drugs that affect cardiac activity - the choice of drug depends on the heart disease.
For oncological diseases, conservative therapy is indicated when surgical treatment is contraindicated, there is a small amount of effusion, and there is no progression of symptoms.
Water in the lungs may appear 1-2 weeks after heart surgery. To reduce the likelihood of developing edema, patients are prescribed therapeutic exercises to improve blood circulation and increase the volume of air in the lungs. When acute edema develops, oxygen masks, bronchodilators, diuretics, and drugs that increase the resistance of heart cells to oxygen starvation are prescribed. The doctor can tell you in detail how to treat water in the lungs in older people, what medications to take.
Treatment of pulmonary edema
People with acute respiratory failure are treated in the intensive care unit. First aid consists of measures that reduce venous return to the heart. To do this, the patient must take a semi-sitting position. Applying tourniquets to the limbs and hot foot baths have a positive effect.
It is imperative to monitor blood oxygen saturation levels. Oxygen therapy is used to compensate for its deficiency. If pulmonary edema has developed against the background of mechanical asphyxia, it is necessary to clear the airways of foreign objects. If it is impossible to breathe independently, the patient is connected to a ventilator.
A combination of medications is used to eliminate pulmonary edema. Among them:
- morphine and other narcotic analgesics;
- drugs to stimulate diuresis;
- nitroglycerine;
- drugs to lower blood pressure.
Depending on the underlying disease, patients with pulmonary edema are prescribed antihistamines, antibiotics, hormonal and antiarrhythmic drugs, and cardiac glycosides. The task of the resuscitator is to stop the attack and prevent acute hypoxia, which leads to cell death and death of the patient. After the symptoms of respiratory failure are relieved, treatment of the disease that caused it begins.
It is very important to eliminate the root cause that led to the clinical syndrome. Otherwise, a relapse of the disease is possible.
Treatment of fluid accumulation in the lungs
Treatment is based on the following principles:
- If the disease is not acute, then you can treat it at home under the supervision of a doctor.
- When symptoms become acute, immediate hospitalization is indicated. In a hospital setting, fluid is artificially removed using a catheter.
- In the chronic form, a complex of drugs is prescribed. In this case, treatment is determined by the underlying disease. For infectious diseases, antibiotics are used. In case of heart failure, diuretic drugs are used. Diseases caused by pathogens are treated with antibiotics.
Fluid in the lungs is an urgent symptom, so it is important to consult a doctor promptly.
Predictions and prevention
Pulmonary edema is a deadly condition; Mortality with this clinical syndrome is up to 50%. Patients with anaphylactic shock most often develop fulminant or acute pulmonary edema, which in more than 90% leads to death.
The consequences of acute pulmonary failure are no less serious than the disease itself. Many patients who have suffered pulmonary edema experience ischemic damage to internal organs, the appearance of areas of pneumosclerosis, and congestive pneumonia. This affects the functioning of the respiratory system, in the organs of which irreversible changes occur. The pathology is manifested by shortness of breath, chest pain, and cough. Pneumosclerosis and other consequences of pulmonary edema require long-term treatment, can lead to disability and shorten the patient's life expectancy.
The likelihood of a favorable prognosis and outcome of the disease with pulmonary edema increases if the diagnosis was made in a timely manner and doctors began to stop the attack at the initial stage.