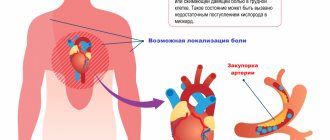
The heart is a muscular pump that ensures continuous movement of blood through the vessels. Together, the heart and blood vessels make up the cardiovascular system. This system consists of the systemic and pulmonary circulation. From the left side of the heart, blood first moves through the aorta, then through large and small arteries, arterioles, and capillaries. In the capillaries, oxygen and other substances necessary for the body enter the organs and tissues, and from there carbon dioxide, metabolic products, are removed. After this, the blood turns from arterial to venous and again begins to move towards the heart. First along the venules, then through smaller and larger veins. Through the inferior and superior vena cava, blood again enters the heart, only this time into the right atrium. A large circle of blood circulation is formed.
Venous blood from the right side of the heart is sent through the pulmonary arteries to the lungs, where it is enriched with oxygen, and returns to the heart again - this is the pulmonary circulation.
Inside, the heart is divided by partitions into four chambers. The two atria are divided by the interatrial septum into the left and right atria. The left and right ventricles of the heart are separated by the interventricular septum. Normally, the left and right parts of the heart are completely separate. The atria and ventricles have different functions. The atria store blood that flows into the heart. When the volume of this blood is sufficient, it is pushed into the ventricles. And the ventricles push blood into the arteries, through which it moves throughout the body. The ventricles have to do more hard work, so the muscle layer in the ventricles is much thicker than in the atria. The atria and ventricles on each side of the heart are connected by the atrioventricular orifice. Blood moves through the heart in only one direction. In the systemic circle of blood circulation from the left side of the heart (left atrium and left ventricle) to the right, and in the small circle from the right to the left.
The correct direction of blood flow is ensured by the valve apparatus of the heart:
Valves:
- tricuspid
- pulmonary
- mitral
- aortic
They open at the right time and close, preventing blood flow in the opposite direction.
How does your heart work?
The heart is a unique muscular organ located in the middle of the chest. The heart pumps blood throughout the body, saturating cells with oxygen and nutrients. The muscular septum divides the heart longitudinally into left and right halves. The valves divide each half into two chambers: the upper (atrium) and the lower (ventricle).
As the heart muscle contracts, it pushes blood first through the atria and then through the ventricles. In the lungs, the blood is saturated with oxygen and through the pulmonary veins enters the left atrium, then into the left ventricle and from it, through the aorta and arterial vessels branching from it, it is distributed throughout the body.
Having given up oxygen, the blood collects in the vena cava, and through them into the right atrium and right ventricle. From there, through the pulmonary artery, the blood enters the lungs, where it is again enriched with oxygen. The main indicator of the heart's performance is the amount of blood it must pump in 1 minute. Usually for an adult this is at least 5.0 liters (300 liters per hour, 7200 liters per day).
The heart beats more than 100,000 times a day, pumping blood through the 20,000 km of veins and arteries that make up the human circulatory system.
When an adult is at rest, the heart beats 60 to 80 times per minute. During physical activity, at a time of stress or excitement, the heart rate can increase to 200 beats per minute.
Cardiac cycle
Adequate blood supply to the body is ensured by the coordinated contraction of the muscle fibers of the heart wall, which determine the organ’s work cycle.
There are two main phases:
- systole – contraction;
- diastole – relaxation.
The different speeds of impulse conduction through atypical cardiomyocytes with the presence of a delay in the atrioventricular node ensure the coordinated functioning of the organ: during atrial systole, blood penetrates into the ventricles. The latter are in the relaxation phase, which forms a sufficient volume to be filled with liquid (up to 100 ml on the left).
During contraction of the ventricles, the valves of the aorta and pulmonary artery open, the valves of the atrioventricular connections are closed - blood flows into the circulation. The pulse is determined in the peripheral vessels, and the heartbeat is determined in the chest area.
At this time, the atria are in the diastole phase and are filled with blood from the hollow (right sections) and pulmonary veins (left).
There is a statement that the heart works half its life and rests half of its life, since the duration of systole and diastole is the same (0.4 seconds each).
Heart rhythm and conduction disorders
The normal heart rhythm is called sinus rhythm.
The heart has its own electrical (conducting) system, consisting of an electrical impulse generator - the main pacemaker - and conductive pathways connecting the entire electrical circuit. The main pacemaker, located in the right atrium, generates regular electrical impulses at a certain frequency, like a metronome. In response to each impulse, the chambers of the heart contract in strict sequence.
First, a wave of electrical excitation covers the atria, as a result of which they simultaneously contract, throwing blood into the ventricles. Having passed through the atria, the wave does not immediately pass to the ventricles, since they are separated from the atria by tissue that is unable to conduct electrical impulses. In only one small area, a single “bundle of wires” passes through this tissue, through which, after a short delay, the electrical impulse can travel to the ventricles and cause the same wave-like contraction as in the atria. This bundle is called the atrioventricular junction (AV node), and the delay between the contraction of the atria and ventricles is necessary so that the atria have time to “push” blood into the ventricles before the latter begin to contract.
Normally, the atrioventricular junction is the only place in the heart where the transfer of electrical excitation to the ventricles occurs. After this, the electrical impulse spreads through both ventricles, causing them to contract. At the same time, the blood is pushed out of them into the arteries, providing blood supply to all organs of the body and the heart itself.
Thus, a normal heart rhythm differs from an abnormal one in two main features: regularity and a certain frequency. Any disturbance in heart rhythm is always a consequence of dysfunction of the conduction system.
What is circadian rhythm
We live in accordance with the rhythms of nature: after night, day inevitably comes, darkness is necessarily replaced by light. And, in order to adapt to this regular alternation of conditions set by the external environment, our body has developed a very complex and as yet not yet fully understood mechanism of the internal clock - our “built-in chronometer,” which physiologists call the daily or circadian (circadian) rhythm. If literally translated from Latin, “circa” means about, and dia means “day”. That is, the circadian rhythm is a rhythm with a period of about a day. Why was this prefix “about” needed? The fact is that the time of completion of the full cycle of our “built-in chronometer” is still controversial among scientists, since the internal regularity of the body does not fit exactly into the 24 hours that make up our astronomical day.
In 1962, physiologist-researcher Aschoff, as an experiment, sent his sons to a sound- and light-proof bunker, where they lived, focusing only on their internal rhythms, and not on the alternation of light day and dark night. This study showed that the internal chronometers of regular variability in human physiological functions are actually tuned to a 25-hour rhythm [1]. But there is another opinion. For example, the results of an experiment led by the famous speleologist Michel Cifra demonstrated that participants imprisoned in a cave for several months experienced a gradual transition from 24-hour rhythms to 48-hour ones: a person needed 36 hours to be awake and 12 to sleep [2 ].
But, one way or another, there is no doubt that an internal biological clock operates in our body, and it works, as genetic research in recent years has revealed, in every cell of our body. The genetic nature of biological rhythms began to be revealed in 1971, when for the first time in the world the clock gene Per was found in the Drosophila fly - it was called an abbreviation for the word “period” [3]. It was observed that a mutation in this gene caused deviations in the periodicity of the circadian rhythm in flies. These studies laid the foundation for a number of discoveries, as a result of which the modern understanding of the molecular structure of the biological clock was formed.
Bradycardia. Slow heart rate
Your heart rate usually beats between 60 and 80 beats per minute.
A reading below 60 beats per minute is called bradycardia. For many people in good physical shape, or if such a rhythm occurs during rest and sleep, then such a rhythm is normal. A distinctive feature of such bradycardia is that with increasing physical activity, the heart rate begins to accelerate, covering the body’s needs with its frequency.
We talk about bradycardia as a disease when the rhythm has a very low frequency, does not respond by increasing frequency to physical activity, or large pauses occur in the rhythmic contraction, which can reach or even exceed more than 2 seconds. Such disturbances lead to fatigue, dizziness and loss of consciousness.
The most common cause of a slow heart rate is:
• Sinus node dysfunction (SU).
• Impaired conduction of the electrical signal from the atria to the ventricles through the atrioventricular node (AV).
When bradycardia is confirmed diagnostically and such a rhythm is the only manifestation, then such a rhythm is effectively corrected by a pacemaker. ICDs can also be used for bradycardia, but only if there are appropriate indications for ICD implantation (life-threatening cardiac arrhythmias).
Loss of synchronization and disease progression
As experiments show, synchronization of all internal rhythms is an extremely important condition for maintaining health and life expectancy. When scientists study the relationship between a malfunctioning biological clock and heart disease, the obvious question that arises is what comes first: a breakdown in the internal clock causes heart disease, or is it the heart pathology itself that causes the malfunction of our built-in chronometers? In an attempt to answer this question, at least two opposing hypotheses have been put forward.
In support of the hypothesis that the loss of synchronization of internal rhythms is primary in the onset of the disease, a number of interesting experiments were conducted. Researcher Tami Martino analyzed the lifespan of golden hamsters with a specific mutation in the tau gene, which reduces the period of the circadian rhythm in the peripheral clock to 22 hours (Figure 2). In other words, the internal clock of this line of cheeky rodents is very fast. It turned out that the overall life expectancy of hamsters with the mutation is reduced by 20%, and they die at an early age from serious myocardial diseases - fibrosis and cardiomyopathies [6].
Figure 2. Golden hamster with a mutation in the tau gene: the hamster's internal clock is fast by two hours a day. The lack of synchronization of internal and external rhythms led to the fact that the rodent developed serious health problems - myocardial hypertrophy.
However, when artificial conditions were created for such hamsters so that the period of alternating light and darkness was 22 hours, the cardiac pathology was replaced by normal functioning of the heart. Moreover, removal of the suprachiasmatic nucleus, the main clock of the body, also had a preventive effect: myocardial hypertrophy did not develop in golden hamsters after the operation. What is the reason for such a miraculous healing?
The results obtained indicate that it is not so much damage to the peripheral clock as loss of synchronization between the central and peripheral pacemakers that leads to the occurrence of cardiovascular pathology. In mutant hamsters, there was a mismatch between the 22-hour period of the peripheral clock and the 24-hour period of the central clock. When a rhythm of 22 o'clock was imposed on the central chronometer through changes in external conditions (light/dark), it was synchronized with the peripheral clock, and cardiac pathology did not develop. And when the suprachiasmatic nucleus was removed, then again nothing prevented the peripheral clock from freely implementing its own rhythm, and the hamster’s heart was again saved.
On the other hand, the disease itself can disrupt the coherence of internal biorhythms. For example, during acute myocardial infarction, damaged cells undergo a phase shift in the circadian clock relative to healthy tissues. This loss of synchronization is very dangerous and can cause life-threatening arrhythmia attacks.
Restoring the coherence of heart cell rhythms with the natural cycles of other organs and tissues and with cyclical changes in environmental conditions may be a promising strategy in the fight against cardiovascular diseases. But to implement this direction, very deep knowledge about the patterns of functioning of biorhythms is required. Interestingly, even in healthy people, the circadian rhythm of the cells in the inner lining of the veins varies depending on their anatomical location. Further research is needed to identify all the zeitgebers in the body as accurately as possible, and to use this knowledge to repair our built-in chronometers if they fail.
Tachycardia
If your heart rate exceeds 100 beats per minute, it is called tachycardia. Tachycardia can be sinus and belong to normal, physiological tachycardia. Tachycardias with a high frequency, which exceed 180 beats per minute, arising in connection with frequent, group extrasystole, additional conduction pathways are classified as a group of non-normal fast heart rhythms.
Physical activity, emotional stress, and certain diseases can cause an accelerated heart rate that exceeds 100 beats per minute.
When your heart rhythm is very fast or your heart beats for no reason at a high frequency and irregularly, it is called tachyarrhythmia.
Pathological tachycardia is harmful for several reasons. Firstly, with a rapid heartbeat, the efficiency of the heart decreases, since the ventricles do not have time to fill with blood, as a result of which blood pressure drops and blood flow to the organs decreases. Secondly, the conditions of the blood supply to the heart itself worsen, since it does more work per unit of time and requires more oxygen, and poor conditions of the blood supply to the heart increase the risk of coronary disease and subsequent heart attack.
Tachycardia is not a disease, but a symptom, since it can occur as a manifestation of many different diseases. The most common causes of tachycardia are disorders of the autonomic nervous system, endocrine system disorders, hemodynamic disorders and various forms of arrhythmia.
Hierarchy of internal biological clocks
So, how does our internal clock work? Recent studies indicate that the internal pacemakers in our body are organized according to the laws of hierarchy: there are the most important clocks and subordinate clocks. The main center of the circadian clock is the suprachiasmatic nucleus in the brain, a dense cluster of about 20 thousand neurons, and it is located just next to the center that regulates the production of hormones in the body. As for the subordinate clocks, as analysis of gene expression in the cells of internal organs has shown, genes responsible for circadian rhythms are expressed in every cell of the body, including even connective tissue. This led scientists to believe that each organ has its own internal clock. The internal clock system of the internal organs was called the peripheral clock, and the suprachiasmatic nucleus that controls them was called the central clock (Fig. 1). The liver, blood vessels, heart, and kidneys have their own chronometer. But for the body to function effectively, it is extremely important that all clock mechanisms are tuned to work harmoniously in the same rhythm - synchronized.
Figure 1. Hierarchy of the internal biological clock: the main center of the circadian clock is the suprachiasmatic nucleus in the brain, which sets the rhythm of all cells of the body through the autonomic nervous system, specialized hormones and various factors. Subordinate clocks in the cells of internal organs are called peripheral.
The phases of internal chronometers can shift under the influence of certain stimuli that can impose their own rhythm. Such stimuli are called zeitgebers (from German Zeit - “time” and geben - “give”) or pacemakers. Each watch is capable of responding to its own specific pacemakers. For example, light sets the rhythm of the central clock in the suprachiasmatic nucleus, while it does not directly affect the peripheral clock. Zeitgebers can be not only external influences, but also behavioral patterns: physical activity regimen, sleep-wake cycle, and even diet. For example, it has been clearly shown that the internal clock of the liver is more tuned to the rhythm of food intake than to the rhythms of the light and dark periods of the day [4].
The main physiological synchronizer of all peripheral clocks is the suprachiasmatic nucleus. Thanks to their connections with the light-sensitive cells of the retina, the neurons of the suprachiasmatic nucleus are able to receive information about the photoperiod from the outside and adjust the internal rhythms of the body to external conditions. Synchronization of peripheral clock systems is carried out through the autonomic nervous system by special hormones and, possibly, other, as yet poorly understood, pathways. Every year, scientists discover and describe in detail more and more new factors that influence the regulation of internal rhythms [5].
Tachyarrhythmia
This is an abnormally fast heart rate (usually 100 to 400 beats per minute, which occurs either in the upper chambers of the heart (atrial fibrillation, supraventricular tachycardia) or in the lower chambers (ventricular fibrillation, ventricular tachycardia)).
Causes of tachyarrhythmia:
• Heart diseases such as high blood pressure, coronary artery disease (atherosclerosis), heart valve disease, heart failure, cardiomyopathy, tumors and infections.
• Other medical conditions, such as thyroid disease, some lung diseases, electrolyte imbalances, and alcohol and drug abuse.
• Caused by abnormal accessory pathways or extrasystoles.
Tachyarrhythmias occur when the impulse contracting the heart muscle arrives earlier than normal heart rhythm would suggest. Tachyarrhythmias can begin in the upper or lower chambers of the heart.
Tachyarrhythmia includes various types of cardiac arrhythmias:
• Supraventricular tachycardia.
• Ventricular tachycardia (VT).
• Ventricular fibrillation (VF).
Physiology - the principle of operation of the human heart
Let's take a closer look at the principles and patterns of heart function.
Cardiac cycle
When an adult is calm, his heart beats in the range of approximately 70-80 cycles per minute. One pulse beat equals one cardiac cycle. At this speed of contraction, one cycle is completed in approximately 0.8 seconds. Of which, the contraction time of the atria is 0.1 seconds, the ventricles are 0.3 seconds, and the relaxation period is 0.4 seconds.
The frequency of the cycle is set by the cardiac pacemaker (the area of the heart muscle in which impulses arise that regulate the heart rate).
The following concepts are distinguished:
- Systole (contraction) - this concept almost always means contraction of the ventricles of the heart, which leads to a push of blood through the arterial bed and maximization of pressure in the arteries.
- Diastole (pause) is a period when the heart muscle is in the stage of relaxation. At this moment, the chambers of the heart fill with blood and the pressure in the arteries decreases.
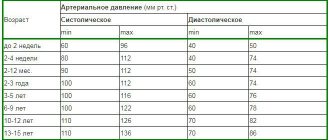
So, when measuring blood pressure, two indicators are always recorded. Let's take the numbers 110/70 as an example, what do they mean?
- 110 is the top number (systolic pressure), that is, the pressure of the blood in the arteries at the moment of heart contraction.
- 70 is the lower number (diastolic pressure), that is, this is the pressure of the blood in the arteries at the moment the heart relaxes.
A simple description of the cardiac cycle:
- Cardiac cycle (animation)
At the moment of relaxation of the heart, the atria, and even the ventricles (through open valves), fill with blood.
- Atrial systole (contraction) occurs, allowing blood to completely move from the atria to the ventricles. Contraction of the atria begins at the point where the veins flow into it, which guarantees initial compression of their mouths and the inability of blood to flow back into the veins.
- The atria relax, and the valves separating the atria from the ventricles (tricuspid and mitral) close. Ventricular systole occurs.
- Ventricular systole pushes blood into the aorta through the left ventricle and into the pulmonary artery through the right ventricle.
- This is followed by a pause (diastole). The cycle repeats.
Conventionally, for one pulse beat there are two heart contractions (two systoles) - first the atria contract, and then the ventricles. In addition to ventricular systole, there is atrial systole. Contraction of the atria is of no value when the heart is working steadily, since in this case the time of relaxation (diastole) is enough to fill the ventricles with blood. However, once the heart starts beating faster, atrial systole becomes crucial - without it, the ventricles simply would not have time to fill with blood.
The push of blood through the arteries occurs only when the ventricles contract; it is these push-contractions that are called the pulse.
Heart muscle
The uniqueness of the heart muscle lies in its ability to perform rhythmic automatic contractions, alternating with relaxations, which occur continuously throughout life. The myocardium (the middle muscular layer of the heart) of the atria and ventricles is divided, which allows them to contract separately from each other.
Cardiomyocytes are muscle cells of the heart with a special structure that allows them to transmit a wave of excitation in a particularly coordinated manner. So there are two types of cardiomyocytes:
- ordinary workers (99% of the total number of cardiac muscle cells) - designed to receive a signal from the pacemaker through conducting cardiomyocytes.
- special conducting (1% of the total number of cardiac muscle cells) cardiomyocytes - form the conducting system. In their function they resemble neurons.
Like skeletal muscles, the heart muscle can increase in volume and increase its efficiency. The heart capacity of endurance athletes can be 40% larger than that of the average person! We are talking about beneficial hypertrophy of the heart, when it stretches and is able to pump more blood in one beat. There is another hypertrophy called “athletic heart” or “bull heart”.
The bottom line is that in some athletes the mass of the muscle itself increases, and not its ability to stretch and push large volumes of blood. The reason for this is irresponsibly designed training programs. Absolutely any physical exercise, especially strength training, should be based on cardio training. Otherwise, excessive physical stress on an unprepared heart causes myocardial dystrophy, which will lead to early death.
Conduction system of the heart
The conduction system of the heart is a group of special formations consisting of non-standard muscle fibers (conducting cardiomyocytes) and serving as a mechanism for ensuring the coordinated functioning of the parts of the heart.
Pulse path
This system ensures automatism of the heart - excitation of impulses generated in cardiomyocytes without an external stimulus. In a healthy heart, the main source of impulses is the sinoatrial (sinus) node. He is the leader and blocks the impulses from all other pacemakers. But if any disease occurs that leads to sick sinus syndrome, then other parts of the heart take over its function. Thus, the atrioventricular node (automatic center of the second order) and the His bundle (AC of the third order) are able to activate when the sinus node is weak. There are cases when secondary nodes enhance their own automaticity even during normal operation of the sinus node.
The sinus node is located in the upper posterior wall of the right atrium in close proximity to the mouth of the superior vena cava. This node initiates pulses with a frequency of approximately 80-100 times per minute.
The atrioventricular node (AV) is located in the lower part of the right atrium in the atrioventricular septum. This septum prevents the impulse from propagating directly into the ventricles, bypassing the AV node. If the sinus node is weakened, then the atrioventricular node will take over its function and begin to transmit impulses to the heart muscle at a frequency of 40-60 contractions per minute.
Next, the atrioventricular node passes into the His bundle (the atrioventricular bundle is divided into two legs). The right leg rushes towards the right ventricle. The left leg is divided into two more halves.
The situation with the left bundle branch has not been fully studied. It is believed that the left leg with fibers from the anterior branch rushes to the anterior and lateral wall of the left ventricle, and the posterior branch supplies fibers to the posterior wall of the left ventricle and the lower parts of the lateral wall.
In case of weakness of the sinus node and atrioventricular block, the His bundle is capable of creating impulses at a speed of 30-40 per minute.
The conduction system deepens and further branches into smaller branches, eventually passing into Purkinje fibers, which penetrate the entire myocardium and serve as a transmission mechanism for contraction of the ventricular muscles. Purkinje fibers are capable of initiating impulses at a frequency of 15-20 per minute.
Exceptionally trained athletes can have a normal resting heart rate down to the lowest recorded figure of just 28 beats per minute! However, for the average person, even one leading a very active lifestyle, a heart rate below 50 beats per minute may be a sign of bradycardia. If your heart rate is this low, you should be examined by a cardiologist.
Heartbeat
A newborn's heart rate may be around 120 beats per minute. As a person gets older, the pulse stabilizes between 60 and 100 beats per minute. Well-trained athletes (we are talking about people with well-trained cardiovascular and respiratory systems) have a heart rate of 40 to 100 beats per minute.
The rhythm of the heart is controlled by the nervous system - the sympathetic strengthens contractions, and the parasympathetic weakens.
Cardiac activity, to a certain extent, depends on the content of calcium and potassium ions in the blood. Other biologically active substances also contribute to the regulation of heart rhythm. Our heart may begin to beat faster under the influence of endorphins and hormones released when listening to our favorite music or kissing.
In addition, the endocrine system can have a significant impact on the heart rhythm - both the frequency of contractions and their strength. For example, the release of the well-known adrenaline by the adrenal glands causes an increase in heart rate. The hormone with the opposite effect is acetylcholine.
Heart sounds
One of the simplest methods for diagnosing heart disease is to listen to the chest using a stethoscope (auscultation).
In a healthy heart, during standard auscultation, only two heart sounds are heard - they are called S1 and S2:
- S1 is the sound heard when the atrioventricular (mitral and tricuspid) valves close during ventricular systole (contraction).
- S2 - the sound heard when the semilunar (aortic and pulmonary) valves close during diastole (relaxation) of the ventricles.
Each sound consists of two components, but to the human ear they merge into one due to the very short period of time between them. If, under normal conditions of auscultation, additional tones become audible, this may indicate some kind of disease of the cardiovascular system.
Sometimes additional abnormal sounds may be heard in the heart, called a heart murmur. As a rule, the presence of murmurs indicates some kind of heart pathology. For example, noise can cause blood to flow back in the opposite direction (regurgitation) due to malfunction or damage to a valve. However, noise is not always a symptom of a disease. To clarify the reasons for the appearance of additional sounds in the heart, it is worth doing echocardiography (ultrasound of the heart).
Supraventricular tachyarrhythmias
Rhythm disorders involving the atria are called supraventricular (supraventricular) arrhythmias. This group of rhythm disturbances is the most common, and it is the one that doctors and patients have to deal with most often. There are 5 main types of supraventricular arrhythmias:
• atrioventricular nodal tachycardia;
• Wolff-Parkinson-White syndrome;
• intraatrial tachycardia;
• atrial flutter;
• atrial fibrillation.
Peripheral clocks in vascular muscle cells
The smooth muscle cells of blood vessels - myocytes - also have their own peripheral clock. Takishige Kunieda studied the circadian system in aging vascular myocytes. He found that in these cells, the loss of circadian rhythmicity is associated with telomere shortening. The introduction of telomerase prevented problems with the expression of clock genes. These studies suggest that telomerase regulation may be one of the therapeutic options for age-related circadian rhythm disorders [11].
Atrial fibrillation (AF)
Atrial fibrillation is the most common arrhythmia, usually a manifestation of other heart diseases (coronary heart disease, valvular disease, myocarditis, etc.) or metabolic disorders (thyrotoxicosis, electrolyte imbalance, etc.). Sometimes it occurs without an obvious cause, and then it is called idiopathic.
The mechanisms of development of atrial fibrillation are still not fully understood. In some patients, it occurs due to the presence of many chaotic circular waves of electrical excitation in the atria.
Atrial fibrillation is usually treated with medications that maintain a normal rhythm or prevent the heart rate from getting too fast. A prerequisite for atrial fibrillation is the use of anticoagulant therapy. It is used to thin the blood to prevent the formation of blood clots.
For the surgical treatment of atrial fibrillation, the method of radiofrequency ablation (RFA) is used, which is used to slow down the heart rate (RFA of the AV junction) or RFA “isolation of the pulmonary veins” is performed to restore sinus rhythm.
Ventricular tachycardia (VT)
VT refers to an abnormally rapid heartbeat. The source of such a rhythm may be an ectopic focus in the myocardium of the right or left ventricle. Typically, the cause of ventricular abnormal pacemakers is diseases of the heart muscle (coronary heart disease, arrhythmogenic dysplasia of the right ventricle, etc.). In VT, the heart does not pump blood as efficiently as it does in normal sinus rhythm. The rapid rhythm of contractions prevents the ventricles from filling completely between individual heartbeats. As a result, the volume of blood circulation in the body decreases.
With VT, symptoms such as dizziness, fainting, presyncope, and loss of consciousness occur. For most patients, VT is considered a very dangerous rhythm, which can lead to the death of the patient.
Ventricular fibrillation (VF)
VF is a very fast, irregular heart rhythm that occurs in the right or left ventricle of the heart. VF is a more serious pathology than VT because the electrical system of the heart and the heartbeat cycle are completely disorganized. The ventricles tremble and the body receives only a small amount of pumped blood or none at all.
When the heart does not pump blood, the body quickly begins to experience oxygen starvation and sudden cardiac arrest occurs.
Symptoms develop immediately: first the pulse disappears, then consciousness, then the ability to breathe. If sudden cardiac arrest occurs, cardiopulmonary resuscitation (CPR) is required to keep the blood circulating until an external defibrillator can be used to restore the heart rhythm. Defibrillation can be performed by a doctor or emergency medical personnel using an external defibrillator by discharging an electric current through plates located on the chest. If the patient has an ICD implanted, defibrillation will occur automatically after a few seconds of VF onset.
Synchronization of the molecular clock of cardiac muscle cells with lipid metabolism
We have already talked about how important it is to synchronize heart rhythms with the cycles of other physiological systems of the body. It is equally important to note that some internal cycles are capable of imposing their rhythm on the heart clock. One of these master cycles is the daily rhythm of the circulation of fatty acids and lipid levels, which is tightly linked to the circadian one. Fatty acids are the primary “heart fuel”: 70% of them are utilized by the heart. With an excess of fatty acids, the contractile function of the heart is suppressed, and the heart responds to these changes in the internal environment by activating both oxidative (mitochondrial) and non-oxidative metabolism. In this way, the heart reduces cellular toxicity caused by fatty acid loading. And this process is also associated with the daily rhythms of gene expression.
American researcher Molly Bray studied circadian clock genes using DNA microarray technology. She was able to identify 548 genes that regulate the clock in atrial cardiomyocytes and 176 genes associated with the circadian rhythm of ventricular muscle cells. These included genes involved in lipogenesis and lipid binding proteins; all of them showed diurnal expression [8].