Cardiopulmonary failure is a decompensated stage of cor pulmonale, which occurs with acute or chronic right ventricular heart failure. The occurrence of pathology is associated with impaired blood circulation in the vessels of the lungs, which is accompanied by a decrease in blood oxygen saturation.
There are two main forms of cardiopulmonary failure - acute and chronic. The acute form in most cases occurs as a result of asthma, emphysema or massive thromboembolism. Clinical signs appear several hours after a sharp increase in arterial pressure. The chronic form is characterized by slow development with an increasing clinical picture (it can develop over several months or years).
There are several types of cardiac pulmonary failure, which differ in their characteristic symptoms. Among them: cerebral, anginal, respiratory, abdominal and collaptoid type of pathology. The cerebral type is characterized by signs of encephalopathy (for example, drowsiness and lethargy or, on the contrary, excitability and aggressiveness). Some patients complain of headaches and dizziness.
The anginal type is characterized by the appearance of severe pain in the area (with no irradiation) and a feeling of lack of oxygen. The progression of the respiratory type is accompanied by the appearance of shortness of breath, cough and cyanosis of the skin. The abdominal type is characterized by painful sensations and a feeling of nausea. Without further treatment, stomach ulcers may occur. The collaptoid type is accompanied by a persistent increase in blood pressure, tachycardia and general weakness. In this case, patients experience pallor of the skin.
Circulatory failure depends on two main factors: a decrease in the contractile force of the muscular membrane of peripheral vessels and a decrease in the contractility of the muscular organ. If the first factor significantly predominates, then we are talking about vascular circulatory failure, and if the second predominates, we are talking about chronic heart failure.
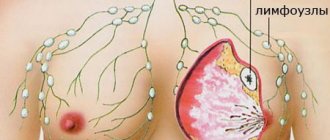
The left and right sections of the muscular organ are responsible for blood circulation. When one of these sections is damaged, isolated or predominant lesions appear, respectively, on the left or right half of the muscular organ. Based on this, left ventricular failure and right ventricular failure are distinguished.
From an anatomical and functional point of view, the lungs and heart have a close relationship. This explains the fact that when one organ is damaged, negative consequences subsequently affect the other. Depending on which of these organs is more affected, pulmonary-cardiac and cardiopulmonary failure are distinguished.
There are two main phases – compensation and decompensation. In the compensation stage, the muscular organ is able to cope with its load and work. But this does not always happen: over time, a period comes when its internal reserves are completely exhausted, resulting in a decompensation phase. In this phase, the muscular organ is no longer able to cope with the load.
First aid for pulmonary edema
Unlike the chronic form, the acute form of the pathology requires immediate assistance during an attack. A person is not able to help himself, so he needs help from the outside. First of all, you should call an emergency team. While waiting for her, the person should be seated on a chair and given a Nitroglycerin tablet. If the attack occurs indoors, be sure to open all windows to provide fresh air flow.
If a person gets worse, cardiopulmonary resuscitation methods are required. To do this, rhythmically press on the chest area or do 30 presses and mouth-to-mouth breathing (alternating these actions). The main goals of these measures are to normalize blood circulation and restore respiratory function. If you lack the skills, you can simply massage the sternum.
Prevention[edit]
It is necessary to prevent or reduce the risk of developing lung disease. Patients in the last stages of emphysema or chronic obstructive pulmonary disease always develop cor pulmonale. In cases where people work in extremely dusty conditions, it is necessary to reduce the dust concentration to a safe level, or transfer them to another non-dusty job.
The employer is required to effectively monitor the degree of air pollution using personal samplers. To this end, US legislation obliges all companies conducting underground coal mining to use (since February 2016) personal PDM dust meters operating in real time[4]. This allows for timely detection of exceeding MPCs and taking adequate corrective measures.
In Soviet and Russian literature on occupational diseases, mine ventilation and occupational safety, the use of respirators has been recommended for many decades. But numerous studies of their effectiveness in real production conditions have shown that this is not only the latest, but also the most unreliable means of protection, and in the USA and the EU the employer is obliged to take all possible measures to reduce dust getting into the air, automate hazardous types of work, use remote control and isolated cabins, effective local ventilation suction and general ventilation, air showers[5], etc., and only after that - use sufficiently effective RPE.
A study of the morbidity rates of workers who used RPE in various industries of the USSR and the Russian Federation showed that, given the customary choice and use of respirators, preserving the health of workers is extremely rarely achieved [6].
Causes of cardiopulmonary failure
Cardiopulmonary failure never occurs without a reason. As a rule, several reasons lead to its development. There are three main groups of causes that can provoke pathology:
1. Bronchopulmonary diseases. According to statistics, they act as a provoking factor in more than 70% of all cases. Among the most common diseases are bronchial asthma, pulmonary tuberculosis, chronic bronchitis and other severe disorders of the respiratory system (for example, cystic fibrosis).
2. Thoradiaphragmatic diseases. They are directly related to pronounced deformation of the chest and limited mobility of the diaphragm. The appearance is caused by severe curvatures of the spinal column (in particular, kyphoscoliosis), ankylosing spondylitis, and restrictions on the expansion of the lungs (pleuritis).
3. Vascular diseases. This group includes diseases that affect lesions of the pulmonary bed. These include sickle cell anemia, pulmonary vasculitis, compression of the pulmonary veins and arteries by neoplasms.
4. Vascular diseases. Often, the development of cardiopulmonary failure is provoked by aneurysms, atherosclerosis and blood clots in the arteries of the lungs.
Notes[edit]
- N. M. Mukharlyamov, V. D. Topolyansky;
V. N. Galankin (pat. an.), I. X. Rabkin (rent.). Pulmonary heart / ed. Petrovsky B.V. — Great medical encyclopedia. - Moscow: Publishing House "Soviet Encyclopedia", 1980. - T. 12. - 536 p. — 150,000 copies. - ↑ 2.02.1 American Medical Network - Pulmonary Heart Disease, Retrieved on 2010-01-25.
- Pulmonary Heart Disease Information, Retrieved on 2010-01-25.
- Jon C. Volkwein, Robert P. Vinson, Steven J. Page, Linda J. McWilliams, Gerald J. Joy, Steven E. Mischler and Donald P. Tuchman
Laboratory and Field Performance of a Continuously Measuring Personal Respirable Dust Monitor. - Pittsburgh, PA: National Institute for Occupational Safety and Health, 2006. - 55 p. — (DHHS (NIOSH) Publication No. 2006-145). There is a translation: PDF Wiki - NIOSH Report on the Development of an Air Shower to Protect Miners from Dust, 2012
- Kaptsov V.A., Chirkin A.V.
On the effectiveness of personal respiratory protection as a means of disease prevention (review) //
Federal Budgetary Institution “Russian Register of Potentially Hazardous Chemical and Biological Substances” of Rospotrebnadzor
Toxicological Bulletin. — Moscow: 2021. — No. 2 (149). — P. 2-6. — ISSN 0869-7922. - Disorders caused by decreased contractility of the heart muscle. Death from acute heart failure is possible, especially if medical care is not provided. Chronic heart failure is usually a terminal disease ( borderline between life and death
)
Diagnosis of pathology
The diagnosis of cardiopulmonary failure is established based on the results of a comprehensive examination. During the initial examination, the doctor collects anamnesis (listens about symptoms, chronic pathologies in the patient and immediate family), performs a visual examination (possible swelling of the feet and legs), conducts a physical examination and standard measures (measuring blood pressure, listening to breathing using a phonendoscope). Upon palpation, a cardiac impulse is detected, and upon percussion, an expansion of the boundaries of the region of the muscular organ, which is partially covered by the lungs, is detected.
Among the laboratory diagnostic methods for making a diagnosis, an analysis of the gas composition of arterial blood is required. If there are problems, patients experience a decrease in P02 and SAO2 P02, and an increase in PC02. Additionally, a general blood test is prescribed to detect an infectious process in the body (by increasing the level of leukocytes). The most informative ways to detect cardiopulmonary failure are instrumental diagnostic methods. Depending on the symptoms, the patient may be prescribed:
- study of respiratory function (external respiration function). With the help of this examination, it is possible to establish the nature and severity of pulmonary ventilation impairment;
- electrocardiography (ECG). This is an accessible method that does not require additional preparation from the patient. The essence of electrocardiography is to record the electrical potentials of a muscle organ, which makes it possible to detect changes in rhythm and electrolyte deficiency. If the disease occurs in an acute form, it is possible to detect signs of overload in the right parts of the muscular organ. If the disease is chronic, it is possible to detect markers (both direct and indirect) of right ventricular hypertrophy;
- echocardiography (EchoCG). It is often prescribed in addition to an ECG, since the information content of this examination regarding cardiopulmonary failure is very high. This is the main non-invasive method with which it is possible to assess intracardiac hemodynamics, determine the size of the cavities of the muscular organ and the degree of pulmonary hypertension. EchoCG allows you to detect a number of possible disturbances in the functioning of the heart, differentiate it from heart disease and other pathologies;
- chest x-ray. This is a simple technique with which it is possible to assess the condition of the respiratory system (detect damage to the internal organ and notice signs of pulmonary hypertension);
- transbronchial lung biopsy. These methods are rarely resorted to, in particularly advanced clinical cases. A puncture biopsy of the lung is performed under ultrasound or X-ray guidance using a local anesthetic.
Signs and symptoms[edit]
Symptoms of cor pulmonale depend on the stage of the disease. In the initial stages, there may be no symptoms at all. But as the disease progresses, most people may experience symptoms:
- Shortness of breath (first - during physical activity, inhalation of cold air, and then - at rest). As the disease progresses, the nature of shortness of breath changes, it is less dependent on the weather and becomes more constant.
- Wheezing
- Chronic cough with expectoration of mucus. After coughing, the intensity and duration of shortness of breath increase, and it does not decrease after taking bronchodilators ( medicines that treat
the symptoms of the disease - dilate the bronchi
). - Performance decreases.
- Accumulation of free fluid in the abdominal cavity (ascites).
- Swelling of ankles and feet.
- Enlargement and swelling of veins in the neck and face.
- Enlarged liver.
- Blue discoloration of the skin (cyanosis, cyanosis).
- At the last stage, there is a decrease in the amount of urine excreted, disorders of the nervous system occur (headaches, dizziness, noise in the head, drowsiness, apathy), which is associated with a violation of the gas composition of the blood and the accumulation of under-oxidized products.
Patients may complain of pain in the heart of an uncertain nature, which can be combined with suffocation, and heaviness in the right hypochondrium. The causes of pain in the heart region with cor pulmonale are metabolic disorders of the myocardium, as well as relative insufficiency of coronary circulation in the enlarged right ventricle. Pain in the heart area can also be explained by the presence of a pulmonary-coronary reflex due to pulmonary hypertension and stretching of the pulmonary artery trunk.
Disease prevention
In order to prevent pathology, all risk factors that can provoke it should be eliminated. If any negative symptoms appear, it is important to consult a doctor in order to promptly diagnose and treat lung or heart disease. Also, experts recommend leading a healthy lifestyle (not smoking or drinking alcohol), engaging in moderate physical activity and eating right. The diet should be balanced with a predominance of fresh vegetables and fruits.
In order to prevent the development of acute cor pulmonale, patients diagnosed with varicose veins and atrial fibrillation are prescribed indirect anticoagulants. If there are blood clots in the veins, a vena cava filter is often installed. It is a small device that is installed into the lumen of the inferior vena cava. With its help, detached blood clots do not enter parts of the heart muscle and the pulmonary artery system.
Treatment
Treatment of pulmonary heart disease by our specialists is based, first of all, on diagnosing the disease and correct assessment of the severity of the situation. In acute forms, emergency resuscitation measures may be required. An individual approach to each case of cor pulmonale and to each patient, a comprehensive system of treatment and rehabilitation, experienced doctors and modern techniques - all this is aimed at the underlying disease, which results in cor pulmonale syndrome, and at restoring normal cardiac activity.
Modern approaches to the treatment of cor pulmonale
Cor pulmonale (CP) is hypertrophy of the right ventricle that develops in diseases affecting the function or structure of the lungs, or both, except in cases where changes in the lungs are the result of a primary lesion of the left side of the heart or congenital heart defects.
Etiology
According to the WHO classification proposed in 1960, all diseases leading to the development of drugs are divided into three groups:
1. Diseases that primarily affect the passage of air in the lungs and alveoli.
This group includes 21 nosologies: chronic bronchitis, bronchial asthma, emphysema, tuberculosis, pneumoconiosis, bronchiectasis, sarcoidosis, eosinophilic granuloma, berylliosis, chronic diffuse interstitial fibrosis, systemic lupus erythematosus, etc.
2. Diseases that primarily affect chest movements:
kyphoscoliosis and other chest deformities, pleural fibrosis, chronic neuromuscular diseases (for example, poliomyelitis), alveolar hypoventilation, including idiopathic, as well as the condition after thoracoplasty.
3. Diseases that primarily affect the pulmonary vessels:
primary pulmonary hypertension (PPH), polyarteritis nodosa, other arteritis, thrombosis and embolism (including parasitic) of the pulmonary vessels, compression of the pulmonary artery trunk and pulmonary veins by mediastinal tumors, aneurysm, etc.
Pathogenesis
The main link in the pathogenesis of LS is a decrease in the total cross-section of the pulmonary vessels.
Moreover, in patients belonging to groups 1 and 2 of diseases according to the WHO classification, this occurs due to
spasm of small pulmonary arteries
in response to alveolar hypoxia.
This phenomenon was first described in 1946 by Von Euler and Liliestrand. In patients belonging to group 3, narrowing of the pulmonary arteries occurs not only due to vasospasm, which is not preceded by alveolar hypoxia, but also due to narrowing or blockage of their lumen as a result of thrombosis and embolism
, necrotizing arteritis (PLH, systemic vasculitis).
A decrease in the total cross-section of the pulmonary vessels leads to an increase in the total pulmonary vascular resistance and an increase in pressure in the pulmonary circulation.
Under these conditions, the right parts of the heart and, first of all, the right ventricle, experience pressure overload, and subsequently, with the development of tricuspid valve insufficiency, volume overload.
This leads to hypertrophy and dilatation of the right heart
.
As the disease progresses, compensation may fail— right ventricular failure
, which is the terminal stage of this condition.
Diagnostics
Diagnostics of drugs
, as a rule, does not present any difficulties and
consists in identifying hypertrophy and dilatation of the right heart in patients with the listed diseases.
The main methods to determine the enlargement of the right heart are electrocardiography, chest radiography, echocardiography (EchoCG).
Treatment
Treatment of patients with LS is complex.
It is aimed at reducing pressure in the pulmonary artery (PA), eliminating pulmonary and heart failure, which can be achieved by timely and adequate treatment of the disease leading to its occurrence.
Treatment of specific diseases complicated by the development of drugs is described in more detail in the corresponding monographs. This article will discuss approaches to the treatment of drugs themselves.
General recommendations
General recommendations for patients with drugs include adherence to a work and rest schedule
with the exception of excessive physical activity, especially in patients with signs of circulatory failure.
Colds and, above all, flu should be avoided,
which can lead to a significant deterioration in the clinical condition of patients with chronic bronchopulmonary diseases and PLH. Staying at high altitudes can also lead to a worsening of the condition, as it increases vasoconstriction in response to alveolar hypoxia that develops in the mountains. When choosing a method of contraception, women with PLH should keep in mind that birth control pills can cause pro-coagulative changes in the blood coagulation system and, as a result, lead to aggravation of the condition.
Calcium antagonists
This group of drugs is one of the main ones in the treatment of patients with pulmonary hypertension (PH) and drugs. The main purpose of prescribing vasodilators is to reduce pressure in the pulmonary circulation and prevent circulatory failure. First of all, drugs from the group of a-blockers (phentolamine, prazosin) were used in patients with drugs, then hydralazine, sodium nitroprusside, nitroglycerin. All of these drugs led to a significant decrease in pulmonary arterial pressure and total pulmonary vascular resistance, and an increase in cardiac output.
However, a number of reasons have limited the widespread use of these drugs in patients with LS.
First of all, this is the systemic arterial hypotension they cause, which does not allow prescribing high doses of drugs necessary to adequately reduce pressure in the pulmonary circulation. In addition, with long-term administration of some vasodilators (for example, sodium nitroprusside), tolerance develops, requiring a constant increase in their dose. This group of drugs is one of the main ones in the treatment of patients with pulmonary hypertension (PH) and drugs.
It is obvious that the “ideal” vasodilating drug for the treatment of PH should reduce the resistance of the vessels of the pulmonary circulation much more actively than the large one.
These requirements are best met by
calcium antagonists
from the dihydropyridine group.
The first representative of this class of drugs, nifedipine
, when compared with hydralazine and the phosphodiesterase inhibitor amrinone, most significantly reduced pressure in the PA without causing such a pronounced drop in systemic pressure (S. Rich et al., 1983).
This allowed the authors to suggest that nifedipine may cause selective dilatation of pulmonary vessels.
Later Prof.
V.Yu. Mareev et al. (1990) found similar results. In a comparative study of the effect of short-term administration of nifedipine, nitroglycerin, prostaglandin E1, captopril and prazosin on central hemodynamic parameters in patients with PLH, it was revealed that nefidipine significantly reduces pressure in the PA
, acting on the vessels of the pulmonary circulation to a greater extent than on the vessels of the systemic circulation. circle.
In further work (S. Rich, 1985) it was shown that the use of nifedipine is effective not only with short-term administration, but also with long-term therapy - up to 2 years or more.
Prescription of nifedipine in the maximum tolerated dose (up to 240 mg/day) led to a significant decrease in PA pressure in half of the patients with PLH, who are considered the least promising group in terms of treatment.
In 1992, data from a prospective observation of 64 patients with PLH for 5 years were published (S. Rich et al.): 23% of patients were on constant therapy with high doses of nifedipine throughout the entire period. At the same time, there was a significant improvement in their clinical status and survival (94% remained alive at the end of the observation period) in comparison with “non-responders” and those who responded to nifedipine therapy but were not treated (only 36% of patients from this group remained alive at the end of the observation period). end of the observation period).
The main mechanism of action of nifedipine is the relaxation of vascular smooth muscle due to a decrease in the intracellular movement of calcium ions during contraction.
Nifedipine is available in various forms. In addition to short-acting nifedipine, which is currently used extremely rarely - for carrying out acute tests, stopping hypertensive crises, its prolonged forms have been created, in which a gradual slow release of the drug occurs over 24 hours. This makes it possible to prevent or at least significantly reduce the severity of such adverse reactions as tachycardia, systemic hypotension, redness of the face, legs, swelling of the feet, which limits the use of the drug in adequate doses.
In addition to dihydropyridine calcium antagonists, which include nifedipine, benzothiazepines (diltiazem) can be used to treat patients with drugs. The advantages of the drugs include the absence of tachycardia when used, the disadvantages are a weaker vasodilator effect compared to dihydropyridines.
In recent years, new calcium antagonists – amlodipine and isradipine – have been introduced into clinical practice. The drugs have proven themselves to be highly effective drugs for the treatment of both systemic hypertension and PH.
It should be noted that the tactics of prescribing calcium antagonists in patients with LS are somewhat different from those in the treatment of other diseases
and consists in observing the basic four rules.
Rule one:
the dose of drugs should be “titrated”, starting with small dosages and gradually increasing them, bringing them to the maximum tolerated.
For nifedipine, initial doses are 20–40 mg/day; every 3–5 days the dose is increased by 20 mg/day.
Isradipine: initial dosage 2.5–5 mg/day, every 3–5 days the dose is increased by 2.5–5 mg/day.
Diltiazem: initial dose 30–60 mg/day, every 3–5 days the dose is increased by 30 mg/day.
Rule two:
select the dose of the drug taking into account the level of pressure in the PA: with systolic pressure in the pulmonary artery (SPAP), determined during catheterization of the right heart or echocardiography study, less than 50 mm Hg: nifedipine - 40-60 mg / day, isradipine - 7 .5–10 mg/day, diltiazem – 120–180 mg/day; with MPAP from 50 to 100 mm Hg: nifedipine – 80–120 mg/day, isradipine – 10–12.5 mg/day, diltiazem – 180–240 mg/day; with MPAP more than 100 mm Hg. Art.: nifedipine – 120–180 mg/day, isradipine – 12.5–15 mg/day, diltiazem – 240–360 mg/day.
Rule three:
take a differentiated approach to emerging side effects when prescribing calcium antagonists: while systemic hypotension and severe tachycardia can be considered serious adverse reactions requiring dose adjustment, side effects such as redness of the extremities, face, feeling of heat, swelling of the ankles should not cause panic from attending physicians.
Rule four: do not expect an immediate effect from calcium antagonists, since only in a quarter of cases can rapid improvement be observed, developing within a few days from the start of therapy; in other cases, noticeable clinical improvement is observed, as a rule, only after 3-4 weeks.
There are a number of reports on the effective administration of long-acting nitrates in patients with drugs. Most often these are patients with chronic obstructive pulmonary diseases and concomitant ischemic heart disease. The disadvantages of drugs, in addition to frequent headaches, include rapidly developing tolerance to them. Molsidomine does not have this undesirable effect.
, which can be successfully used in this group of patients. The dose of the drug for the treatment of patients with drugs is 8–16 mg/day.
Prostaglandins
Another group of drugs used in patients with drugs are prostaglandins.
The prerequisite for their introduction into clinical practice was research carried out in the 70s, which showed that prostaglandins play an important role in maintaining vascular tone both under normal conditions and in various forms of PH.
The first prostaglandin proposed for the treatment of PH was prostaglandin E1
, which is a short-acting vasodilating agent.
Reports of its use began to appear in the early 80s, and initially this drug was used primarily for conducting an “acute” test to determine the possibility of further therapy with vasodilators. Theoretically, prostaglandin E1 is an ideal drug for these purposes.
It has a short half-life of about 3 minutes, which allows you to quickly titrate the dose of the drug to the desired value and, if necessary, stop the test almost immediately. Unfortunately, a clear relationship between the “response” to the administration of prostaglandin E1 and the effect of therapy with other vasodilating drugs (for example, calcium channel blockers, hydralazine) was not identified. A number of patients who had a significant decrease in PA pressure in the acute test did not respond to long-term therapy with other vasodilators and, conversely, “non-responders” to the use of prostaglandin E1 “responded” to therapy with other vasodilating drugs. This allowed the study authors to conclude that the mechanism of action of prostaglandin E1 and other vasodilators is somewhat different.
Since the mid-80s, prostaglandin E1 has been used to treat patients with PH. A positive quality of the drug is that 70% of it is inactivated in the lungs and, when administered intravenously, the drug enters the systemic circulation in a negligible amount, without causing noticeable systemic hypotension. In addition, the drug has a pronounced antiplatelet effect, which makes it even more attractive for the treatment of patients with drugs and PH
, many of which are prone to thrombosis. At the same time, a significant disadvantage of prostaglandin E1 is the need for its constant intravenous administration to maintain vasodilation.
Therefore, for long-term infusion, a special portable pump is used, connected to a Hickman catheter, which is located in the jugular or subclavian vein. Complications with long-term administration of prostaglandin E1 are usually associated with disruption of the infusion system (for example, thrombosis or infection of the catheter), damage to the pump, or interruption of the infusion due to a variety of reasons. Doses of the drug
, used in patients with PH, range from 5 ng/kg/min to 100 ng/kg/min.
The Russian Cardiology Research and Production Complex uses the following drug dosage regimen: the initial dose is 5–10 ng/kg/min, then gradually increases to 30 ng/kg/min
. With this prescription, maximum pulmonary vasodilation can be achieved with a minimum number of adverse reactions, which include systemic hypotension, cardiac pain of an unspecified nature, headaches and abdominal pain, redness of the face and extremities, nausea.
It should be noted that prostaglandin E1 is prescribed to patients with PH, as a rule, only as monotherapy.
At the same time, its
combination with other vasodilators
, in particular calcium antagonists, may be justified, given the difference in the mechanisms of their vasodilating effect.
We have proposed a regimen of course use of prostaglandin E1
, administered in a daily dose of 60 mcg against the background of constant use of calcium antagonists. When this combination was used for 21 days, more than half of the patients experienced an improvement in clinical status. At the same time, adverse reactions (in particular, systemic hypotension) were mild and did not lead to drug discontinuation.
Recently, another drug from the group of prostaglandins has been used - prostacyclin.
.
Recommended doses are 2–24 ng/kg/min. It is a slightly more active vasodilator than prostaglandin E1, having almost the same advantages and disadvantages as the latter. But the exorbitant cost of prostacyclin does not allow its widespread use. In general, prostaglandins are currently used in patients with drugs who are intolerant to calcium antagonists or when they are ineffective.
Some authors call prostaglandin therapy a “bridge” to transplantation. There are cases where the constant administration of prostaglandins lasted up to 5 years, although on average the maximum period of their continuous use does not exceed several months.
Nitric oxide (II)
Recently, nitric oxide (II) (NO) has been introduced into clinical practice for the treatment of PH. Its vasodilating effect is based on the activation of guanylate cyclase in the smooth muscle cells of the pulmonary vessels, which leads to an increase in the level of cyclo-GMP and a decrease in intracellular calcium levels.
NO is used in the form of inhalations. With this method of administration, this substance quickly combines with hemoglobin, which prevents NO from entering the systemic circulation and the development of arterial hypotension. Therefore, NO can be considered a selective vasodilator, acting exclusively on the vessels of the pulmonary circulation.
NO is the gold standard for acute testing to identify responders and nonresponders to vasodilator therapy.
It compares favorably with prostaglandins in its shorter period of action, ease of administration (inhalation through a face mask or nasal catheter), almost complete absence of side effects, and low cost. To carry out an acute test, inhalation of NO in increasing concentrations is used. As a rule, the maximum drop in pressure in the LA is observed after the initial dose is applied after 2 minutes.
Long-term administration of NO is also being introduced into clinical practice.
. For this purpose, special portable inhalation systems have been created. Treatment is carried out over several weeks, but there are reports of longer-term administration of the drug - up to 1-2 years.
It should be noted that only 25–50% of patients with PH “respond” to vasodilator therapy, that is, they can achieve a decrease in PA pressure and an increase in cardiac output without significant systemic hypotension.
There are the following criteria for “response” to vasodilating therapy during acute tests:
:
• more than 20% reduction in pulmonary vascular resistance;
• more than 20% decrease in pulmonary vascular resistance, accompanied by a drop in the ratio of pulmonary vascular resistance to total vascular resistance;
• increased cardiac output (>10%) together with a decrease in mean pulmonary artery pressure;
• more than 30% reduction in pulmonary vascular resistance combined with more than 10% reduction in pulmonary artery pressure.
Of course, conducting an acute test has some limitations, which were already mentioned earlier, but nevertheless, with its help it is possible to predict quite accurately whether it would be advisable to prescribe vasodilators in a particular patient.
It is currently impossible to say definitively what causes the “non-response” to vasodilating therapy in patients with LS. The most reasonable are two points of view.
According to the first, refractoriness to vasodilators occurs in cases where irreversible changes in small pulmonary vessels predominate, such as intimal fibrosis, plexogenic and dilated lesions.
The second point of view, confirmed by our research data, is that “non-response” to vasodilating therapy can occur in patients with severe disturbances in the hemostatic system, when procoagulative changes come to the fore, and vasospasm does not play a leading role.
Most often these are patients with pulmonary artery thrombosis and PPH. In such patients, it seems advisable to add anticoagulants to the basic therapy with vasodilators. Literature
1. Belenkov Yu.N., Chazova I.E., Samko A.N. and others. The use of the calcium antagonist isradipine in patients with primary pulmonary hypertension // Cardiology. – 1995; (7): 9–13.
1. Belenkov Yu.N., Chazova I.E., Samko A.N. and others. The use of the calcium antagonist isradipine in patients with primary pulmonary hypertension // Cardiology. – 1995; (7): 9–13.
2. Mukharlyamov N.M. Pulmonary heart. – M. Medicine, 1973; 264.
3. Chazova I.E., Zhdanov V.S., Veselova S.P., Mareev V.Yu. Pathology of primary pulmonary hypertension // Arch. pathology. 1993; (3): 77–80.
4. Chazova I.E., Mareev V.Yu. Primary pulmonary hypertension: questions that require answers // Ter. archive. 1994; (3): 77–80.
5. Bardsley P., Evely R., Howard P. Hypoxic cor pulmonale. A review // Herz. 1986; (11): 155–68.
6. Pulmonary circulation / Ed. A. Fishman. – USA. Philidelphia: Univ. Pennsylvania press, 1990; 551.
7. Pulmonary hypertension / Eds. E. K. Weir, J. T. Reeves. – USA, NY, Futura, 1984; 442.
8. Rubin L. Primary pulmonary hypertension // Chest. 1993; (104): 236–50.
9. Vender R. Chronic hypoxic pulmonary hypertension. Cell biology to pathophysiology // Chest. 1994; (106): 236–43.
Nifedipine –
Corinfar (trade name)
(ASTA Medica)
| Applications to the article |
| Rules for prescribing calcium antagonists in patients with cor pulmonale: • drugs should be prescribed from a small dose, gradually increasing it, bringing it to the maximum tolerated; • select the dose of drugs taking into account the level of pressure in the pulmonary artery; • differentiated approach to emerging side effects; • immediate effects should not be expected from calcium antagonists. |
| The main purpose of prescribing vasodilators for cor pulmonale is to reduce pressure in the pulmonary circulation |
| Drugs of choice for the treatment of cor pulmonale: • calcium antagonists; • prostaglandins; • nitric oxide (II) (NO) in the form of inhalations. |