28.06.2017
Diseases of the genitourinary system | Kidneys
The name of this disease, formed by a combination of Greek and Latin terms, contains:
- its character is inflammation (Latin “it”);
- target organ - kidney (Greek "nephros");
- intraorgan localization of primary damage is the glomerulus (Latin “glomus”).
The renal glomerulus is a component of the working unit of the kidney - the nephron (there are about a million of them in each kidney). Here the first stage of blood purification is carried out and the so-called. primary urine. For further “inspection” and return of useful components to the body, it is sent to the nephron canalicular apparatus and gradually turns into something that the body is ready to part with - the so-called. secondary urine.
Acute glomerulonephritis
Inflammatory damage to the renal glomeruli (and subsequently to other components of the organ) is of an immune nature. Immune mechanisms play a special role at the onset of the disease (later, non-immune factors are also involved in its development). Compounds formed in response to the introduction of a “foreigner” (especially repeated) with the aim of neutralizing it (so-called immune complexes) settle in the kidneys, triggering a cascade of inflammatory reactions. Their result is a morphological and functional change in the nephrons, their gradual depletion and death. As a result, the kidneys cease to adequately cope with the role assigned to them. And the body, on the one hand, loses what it needs (for example, proteins and blood cells), and is forced to coexist with what it wants and should get rid of (toxic metabolic products).
Acute inflammation of the glomerular apparatus, as a rule, is characterized by an acute onset with pronounced symptoms (see below). There is also the so-called latent type with subtle signs, mainly detected through laboratory tests.
The acute nature of the disease is more characteristic of young people (children and adolescents) and has a favorable prognosis. In 20% of patients the disease becomes chronic.
Chronic glomerulonephritis
The scenario for the development of pathological changes in renal tissue is similar to the acute type (a combination of immune and non-immune factors). The course is long. Exacerbations are possible. The prognosis is determined by the stage of the process at the time of detection (compensated, decompensated, terminal - severe renal failure), the clinical form of the pathology (nephrotic, hypertensive, hematuric, latent, mixed). Most often we are talking about improving the quality of life and delaying the onset of renal failure. Sometimes complete remission occurs.
Membranous glomerulonephritis
Morphological type (identified by analysis of biopsy material) of acute and chronic damage to the glomerular apparatus of the kidneys.
Glomerulonephritis in children
It accounts for about half of the indications for the use of hemodialysis and subsequent kidney transplantation. The symptoms and mechanism of development of the disease are similar to the “adult” version.
Features of the disease
In the classification of glomerulonephritis, the following forms are distinguished:
- nephrotic, with a predominance of urinary symptoms;
- hypertensive, with increased blood pressure and mild urinary syndrome;
- hematuric, when the main symptom is red blood cells in the urine;
- latent, with mild manifestations of the disease;
- mixed, in which hypertensive and urinary syndromes are equally pronounced.
In children, glomerulonephritis is the second most common disease after urinary tract infections. Among adults, the disease is most common in men under the age of 50; women and older people get sick much less often.
Treatment methods for glomerulonephritis
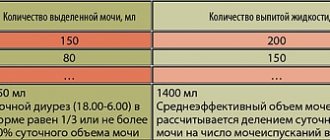
If the process is active, treatment is carried out in a specialized hospital. Bed rest and a special diet are prescribed. Determining the daily volume of fluid that a child should consume is carried out individually for each patient, taking into account many parameters.
Drug treatment is complex and includes glucocorticoids, and it is also possible to prescribe cytostatics. In addition, the treatment uses drugs that lower blood pressure, antibacterial, antihistamines, and, if indicated, diuretics, vitamin therapy, and cardiometabolites. If renal failure develops, hemodialysis is necessary.
Self-medication of glomerulonephritis at home is unacceptable and extremely dangerous for the health and life of the child.
In what cases does the disease develop?
Most often, streptococci or staphylococci become the impetus for the development of the inflammatory process in the renal glomeruli. Doctors consider the main causes of glomerulonephritis to be:
- acute viral infections - influenza, pneumonia, sore throat, scarlet fever;
- vaccination with “live” vaccines”;
- allergic reactions of the body;
- systemic diseases - lupus erythematosus, vasculitis.
You should not discount the accompanying unfavorable factors, first of all:
- chronic infections - caries, sinusitis, tonsillitis, viral hepatitis, etc.;
- uncontrolled use of medications;
- prolonged exposure to the sun;
- frequent consumption of salty foods;
- Presence of unhealthy habits – consumption of alcohol, drugs.
The inflammatory process occurs due to damage to the immune mechanism: antibodies form protein complexes with antigens left in the blood by the infection, and these proteins settle on the walls of the capillaries in the glomeruli. Blood circulation in the kidneys worsens, tissue cells begin to die, which is why the filtering function of the glomeruli deteriorates and the general intoxication of the body increases, which is expressed in a certain set of manifestations.
Acute glomerulonephritis in children
Glomerulonephritis is a heterogeneous group of immunoinflammatory kidney diseases, characterized by predominant damage to the glomeruli, to a lesser extent, tubules and interstitial tissue, different clinical and morphological picture, different course and prognosis.
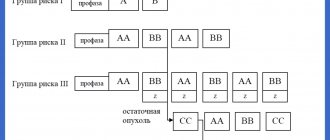
There are primary and secondary, occurring in a number of pathological processes (including systemic vasculitis, diffuse connective tissue diseases, etc.), glomerulonephritis. Primary glomerulonephritis usually occurs in children, and according to their course they are classified into rapid, chronic and rapidly progressive.
Acute glomerulonephritis is understood as an immune complex lesion of the glomeruli, which usually occurs in children 5–12 years old 2–6 weeks after an infection. In the clinic, nephritic syndrome manifests itself, and the morphological substrate of the disease is represented by mesangioproliferative changes. The disease has a cyclical course, and in 80–85% of cases it ends in complete recovery.
Due to the association of the disease with previous infection, it is often called acute postinfectious glomerulonephritis (APIGN).
Most often, acute glomerulonephritis is preceded by pharyngitis, acute tonsillitis, exacerbation of chronic tonsillitis, streptoderma, scarlet fever, erysipelas, and less often - acute respiratory infection. Due to the predominance of diseases of streptococcal etiology, acute glomerulonephritis is also often called acute post-streptococcal glomerulonephritis. Most often, the disease is associated with specific nephritogenic strains of group A B-hemolytic streptococcus. These strains differ in a number of parameters from the streptococci that cause acute rheumatic fever.
The connection between acute glomerulonephritis and streptococcal infection is confirmed by an increase in the level of antistreptococcal antibodies starting from 2–3 weeks of illness, a decrease in the content of individual complement fractions (C3–5), and an increase in the concentration of IgG A (less often M) in the blood serum. Neutrophilic leukocytosis, accelerated ESR, and increased levels of globulins and acute-phase proteins are also noted.
The pathogenesis of the disease is based on damage to the glomeruli of the kidneys by circulating immune complexes, which include streptococcal antigens, immunoglobulins (usually class G) and complement. The second link in pathogenesis is the activation of the hemostasis system with the formation of platelet aggregates and fibrin threads inside the renal glomeruli. Local thrombus formation leads to disruption of microcirculation and the release of vasoactive substances (serotonin, prostaglandins, permeability factor), which subsequently leads to inflammatory proliferation of glomerular cells.
Mesangioproliferative changes in the glomerulus are often combined with disorders in the proximal tubules (dystrophy and destruction of the epithelium) and interstitium with their dysfunction, which indicates a serious prognosis of the disease.
The latent period in cases of acute glomerulonephritis that develops as a result of streptococcal infection lasts from 2 to 8 weeks. With pharyngitis and sore throat, the latent period is usually 10–14 days, with streptoderma - 21 days or more.
The most common reason to consult a doctor is sudden onset of periorbital and peripheral edema, as well as changes in the color of urine, which takes on a “meat slop” color. Patients may also complain of headache, general malaise, loss of appetite, abdominal pain, and heaviness in the lumbar region. Despite the apparent variety of symptoms, all of them, as a rule, fit into the framework of nephritic syndrome. Its main clinical manifestations are dense, symmetrical, fixed edema and arterial hypertension. In addition, there may be changes in the cardiovascular system: tachycardia, expansion of the borders of the heart to the left, intense heart sounds, as well as shortness of breath and abdominal pain.
Hypertension occurs in more than 75% of children. Approximately 5% of hospitalized patients develop severe hypertension, which can lead to the development of angiospastic encephalopathy. The main cause of hypertension is impaired glomerular filtration. Due to the retention of water by the kidneys, the extracellular volume of fluid (ECF) increases, which is accompanied by hypertension. Disruption of microcirculation in the glomeruli leads to continuous irritation of the juxtaglomerular apparatus, natural activation of the RAAS, and the release of aldosterone, which also leads to fluid retention in the bloodstream. An increase in blood volume is manifested in the laboratory as dilution anemia, which is observed with great constancy.
All of the above signs are extrarenal.
Renal manifestations include 4 main symptoms: 1. Gross hematuria with the release of brown urine with a high specific gravity; 2. Proteinuria less than 1 g/m2 per day, or less than 5 mg/kg per day, or less than 3 g/l; 3. Cylindruria; 4. Oliguria.
In some patients with oliguria, the content of urea, creatinine, and potassium in the blood may increase, and a pH shift toward acidosis may occur, which is considered as a violation of kidney function in the acute period.
Extrarenal manifestations usually disappear by the end of 2–3 weeks of illness; renal manifestations can persist for up to 1.5–3 months or more. Microhematuria can persist for a year, after which it is completely eliminated. These provisions are valid for the typical (cyclic) course of OPIGN, but currently an acyclic (atypical) course is also distinguished.
With an acyclic course, the disease manifests itself as isolated urinary syndrome (hematuria, proteinuria without edema and hypertension). Often there is an increase in ESR, sometimes anemia, leukocytosis and eosinophilia. Kidney functions are preserved or slightly impaired. Oliguria is combined with high relative density of urine. Glomerular filtration decreases slightly (up to 50–60 ml/min based on endogenous creatinine clearance). A third of children have a slight increase in serum urea, which is interpreted as hyperazotemia of the acute period, which persists for 3–5 days.
Despite the generally favorable course and prognosis of the disease, complications are not uncommon. Due to an increase in blood volume, for example, acute heart failure of the left ventricular type may develop, which is manifested by shortness of breath, expansion of the borders of the heart, wet cough, and pulmonary edema.
Angiospastic encephalopathy, another common complication of APIGN, is a spasm of cerebral vessels due to increased blood pressure. In the active stage of acute glomerulonephritis, due to damage to the glomerular barrier, decreased glomerular filtration, and impaired microcirculation in the glomerular capillaries, the volume of blood volume increases and the renin-angiotensin-aldosterone system is activated. Thus, the leading links in the pathogenesis of renal eclampsia are vasospasm, cerebrovascular accident, hypoxia up to cerebral edema. Symptoms of angiospastic encephalopathy are: arterial hypertension, bradycardia, insomnia, headache, nausea, repeated vomiting. Subsequently, hypertensive retinopathy is added - impaired visual acuity, “spots”, darkening of the eyes, changes in visual fields, loss of vision. Tonic-clonic convulsions and coma are possible.
The following basic principles are used in the treatment of APIGN: 1) Causal therapy with antibiotics and antiviral drugs; 2) Pathogenetic (anticoagulants, disaggregants, non-enzymatic activators of fibrinolysis); 3) symptomatic (diuretics, antihypertensive drugs, etc.).
In the treatment of acute post-streptococcal glomerulonephritis, preference should be given to penicillin drugs (30–50 mg/kg/day), macrolides (10 mg/kg/day once a day), 1st and 2nd generation cephalosporins are used less frequently. The course of antibiotic treatment should be continued for 10–14 days, however, in children with chronic foci of streptococcal infection, after completing the course of penicillins, it is necessary to use injections of bicillin-5 (1,500,000 units once a month for children under 7 years of age and up to 800,000 from 7 years of age), retarpen (2,400,000 units). The anti-relapse therapy regimen is 6–12–24 months. The need to continue anti-relapse therapy and/or increase/decrease the dose will be indicated by the antistreptolysin level.
When the immune phase of inflammation develops in response to the appearance of a pathogen, the use of antibiotics does not eliminate pathological damage to the kidneys. However, when they are prescribed, the possibilities for the formation of circulating immune complexes in the vascular bed are limited, which can significantly reduce the risks of complications and improve prognoses.
Pathogenetic therapy consists of prescribing disaggregants and anticoagulants. The indication for their use will be hypercoagulation. Direct anticoagulants (heparin and fraxiparin) are prescribed for 3–4 weeks and gradually withdrawn. Disaggregants can be prescribed for a longer period, since improving the rheological properties of blood contributes to a more rapid restoration of the endothelium of the glomeruli of the kidneys. They are usually used in a therapeutic dose for 4–6 weeks, and in a maintenance dose for 1.5–2 months.
If renal function is impaired in the acute period, only kaliuretic diuretics are administered. In cases of severe edema, arterial hypertension, and oliguria, preference is given to fast, strong loop diuretics, such as furosemide. In other cases, hypothiazide can be recommended. By the way, Lasix at a dose of 2 mg/kg is included in the emergency care program for eclampsia, when it is very important to reduce hypervolemia and vasoconstriction in a short time. In addition to furosemide, antihypertensive drugs such as angiotensin-converting enzyme inhibitors and calcium antagonists are used to reduce blood pressure. In severe cases, children with high blood pressure and neurological symptoms in the intensive care unit are recommended sodium nitroprusside, which is administered intravenously at a rate of 0.5–0.8 mcg/kg/min in a glucose solution. This drug should not be used in combination with other antihypertensive drugs.
For convulsions, use Seduxen 0.5% solution intravenously, GHB, because these drugs are the least likely to depress the respiratory center.
During one year of observation, a child who has suffered acute glomerulonephritis should be examined by a pediatrician twice a month for the first three months, once a month for the next nine months of medical examination. In the future, examination is carried out once every 2–3 months and against the background of intercurrent diseases.
After five years of complete remission, examination in a nephrology hospital, or a one-day hospital, or a diagnostic center, the patient can be removed from dispensary observation.
The prognosis for children is very favorable, in most cases they make a complete recovery. However, in 5–15% of children, glomerulonephritis, unfortunately, becomes chronic.
Sources
1. Acute glomerulonephritis in children, Angela Ciuntu, Departamentul Pediatrie USMF 2. Glomerulonephritis in children, Loskutkova S. A., 2015
How to recognize glomerulonephritis
Among the main symptoms of glomerulonephritis:
- the presence of red blood cells in the urine, giving it a characteristic brownish or reddish tint;
- swelling of the tissues of the face (especially noticeable on the eyelids) and legs, appearing in the morning;
- high blood pressure that does not decrease after taking medications;
- worsening urination with severe thirst;
- lack of appetite, sometimes nausea, weakness, headache;
- dyspnea;
- increase in body weight.
If signs of glomerulonephritis appear, you should consult a doctor as soon as possible to avoid the disease becoming chronic. Statistics show that in the absence of treatment this occurs in 60% of cases.
Diagnostic tests
Currently, the diagnosis of glomerulonephritis does not cause difficulties, especially in cases where the symptoms of the disease are well expressed. But even with mild symptoms, laboratory tests and hardware tests allow the doctor to establish a complete picture of the disease, especially in the presence of a previous infection. To do this, it uses the following assignments:
- general and biochemical blood tests;
- general and biochemical urine tests;
- Ultrasound of the kidneys and ultrasound examination of the renal blood vessels;
- X-ray and CT scan of the kidneys;
- nephroscintigraphy;
- excretory urography (only for patients with acute form);
- ECG;
- fundus examination;
- kidney tissue biopsy (in some cases).
The presence of glomerulonephritis is indicated by the presence of protein in the urine, hematuria, increased levels of cholesterol and nitrogenous waste in the blood, as well as critically high values of immune complexes.
After making a diagnosis, the nephrologist prescribes appropriate therapy, taking into account the characteristics of the course of the disease and the general condition of the patient.
Recommendations for the prevention of glomerulonephritis
To prevent the development of glomerulonephritis, you must adhere to the following principles:
- avoid hypothermia;
- treat respiratory infections promptly;
- when a doctor prescribes antibiotics, drink the entire course to the end, following the doctor’s instructions;
- after suffering from a sore throat or acute respiratory viral infection, take a general urine test to exclude the asymptomatic (latent) form.
The treatment tactics for the disease and its complications are highly individual and depend on many factors that must be taken into account.
Self-medication using the Internet or on the advice of pharmacists at a pharmacy is fraught with dangerous complications.
How is glomerulonephritis treated today?
Since this is a fairly serious disease, therapy is possible only in a hospital setting, especially in the phase of pronounced symptoms or in the presence of renal failure. Modern treatment of glomerulonephritis is a complex of measures, of which the most important is given to drug therapy, which, depending on the characteristics of the course of the disease, includes:
- antibacterial drugs to fight streptococci or other infections that provoke the development of inflammation of the renal glomeruli;
- antifungal medications if the disease is caused by a fungal infection;
- anti-inflammatory drugs to reduce inflammation in the kidneys;
- symptomatic medications - antihypertensives, diuretics, immunosuppressants, anticoagulants, etc.
Severe renal failure requires hemodialysis. If the kidney is seriously damaged, a transplant may be needed.
One of the powerful therapeutic factors is a special diet for glomerulonephritis, which reduces the load on the kidneys, allowing the tissues to recover. It is based on the limitation:
- table salt – no more than 3-5 grams per day;
- proteins – no more than 80 grams per day;
- carbohydrates – no more than 350 grams per day;
- fats – no more than 90 grams per day.
The main dishes are cereal soups with potatoes, cereal porridges, pasta, herbs and vegetables, low-fat dairy products, low-fat fish, meat and poultry. Pickles and smoked foods, fried foods, sausages, chocolate, legumes, and canned food are completely excluded. In the hospital, patients receive food as part of diet No. 7, but even after discharge it is recommended to adhere to food restrictions.
Causes of glomerulonephritis
The development of this disease is based on immuno-inflammatory damage to the glomeruli, which occurs when there is an interaction between a certain provoking factor (trigger) and genetic factors. After numerous genetic studies, a hereditary predisposition to the development of this pathology was proven.
The following may act as provoking factors:
- past infectious diseases, both bacterial (especially past streptococcal infection) and viral (influenza virus, adenovirus, etc.);
- exposure to certain chemicals and medications;
- administration of serums, vaccines;
- kidney injury;
- hypothermia.
Also, one of the reasons for the development of this pathology is the presence of autoimmune diseases in the child, against the background of which secondary glomerulonephritis is formed.
At the present stage, two mechanisms for the development of glomerulonephritis are considered. The first is immunocomplex, in which, after a series of complex immune reactions, an antigen-antibody complex is formed in the body, damaging the glomeruli. This mechanism is realized in 80–90% of cases of glomerulonephritis. The second is autoimmune, in which the body produces antibodies to its own tissues, in this case to the glomerular basement membrane.