How to recognize the flu
As a rule, influenza is characterized by sudden development and the absence of prodromal symptoms. In the first days after infection, there is no runny nose or nasal congestion.
The development of the pathogen occurs rapidly, so the incubation period is short, often not exceeding 2 days.
Obvious symptoms of pathology are:
- Severe fever, temperature reaches 38 C or more.
- Alternating fever with chills.
- Headache.
- Pain in the eyes, fear of bright light.
- Aches in joints and muscles.
In addition to signs of intoxication, influenza is accompanied by an intense dry cough innervating the chest area.
Influenza is more dangerous when complications develop on the respiratory system. This manifests itself in increased coughing and shortness of breath. In severe cases, the respiratory rate increases to 30 or more, respiratory failure and acrocyanosis occur. In this case, you must urgently call a doctor. It is acute pneumonia and respiratory dysfunction that are the main causes of death with influenza.
Antibiotics for influenza
Antibacterial agents do not have a therapeutic effect against influenza. Their pharmacological action is determined by their effect on pathogenic bacteria. In this case, they may cause more harm than good. By destroying the microflora in the intestines, medications reduce the body's protective functions, making it more vulnerable to viruses.
Antiviral drugs are used to combat the influenza pathogen. They have a wide range of effects, suppressing the development of various viral infections. Their use is indicated not only for treatment, but also for the prevention of influenza. However, their use without the prescription of a specialist is contraindicated in order to eliminate negative consequences.
Is it possible to overcome resistance?
Over time, the bacteria adapt by producing genes that protect against the effects of antibiotics. If a person becomes infected with such bacteria, it is much more difficult to treat. This process is on a planetary scale, and doctors themselves are largely to blame for the problem. They often thoughtlessly use broad-spectrum antibiotics, which, like carpet bombing, destroy the microflora of the mucous membranes.
“It’s easier to prescribe an antibiotic to a child with a high fever or an unconscious intensive care patient and not worry about further treatment,” complains therapist and medical blogger Philip Kuzmenko. “The doctor simplifies his work by shooting sparrows out of a cannon and achieves the patient’s recovery, but at too high a cost.”
The next time the same disease overtakes a recovered person, the previous medicine may not work, since the bacteria have learned to resist it. In this arms race, microbes have a clear advantage. There will always be bacteria against which even the latest generation of drugs will be powerless.
“Self-medication with antibiotics is the murder of our grandchildren and great-grandchildren,” Dr. Kuzmenko is convinced. — Every day I receive letters that inexperienced or incompetent doctors prescribe antibiotics for ARVI. The mortality rate from influenza does not exceed 2−3%, and from a bacterial infection, for which there is no cure, it reaches 50%. Personally, in the first year of practice I prescribed antibiotics often, then less often, and in the 4th-5th year - almost never. There are 3 groups of so-called antibiotics of choice or first line: penicillins, macrolides and cephalosporins. These drugs are prescribed in case of a threatening situation even before confirmation of an accurate diagnosis. It is a myth that pneumonia can be “heard out” at an early stage, but in some cases the patient may not even make it to the pharmacy. Therefore, empirically, from a variety of antibiotics, “broad-spectrum” drugs were selected that act on 20–25 species of bacteria.”
When to take antibiotics
It is advisable to start taking antibiotics for mixed infections, when other pathogens are added to the flu. This occurs with complications such as bronchitis, pneumonia, laryngitis.
Then the patient is prescribed additional medical examinations to determine the sensitivity of the pathogen to the antibiotic. In this case, Amoxicillin, Augmentin, Ceftriaxone, Amoxiclav may be prescribed.
Prolonged high temperature is also a clear sign of a complicated course of influenza and requires the use of antibacterial agents.
To treat a viral infection, depending on the severity of the disease, drugs are prescribed both orally and by injection.
Modern drugs for the treatment of ARVI and influenza
Acute respiratory infections (ARVI) are the most common among all infectious diseases. ARVI and influenza account for at least 70% of infectious diseases. In Russia, about 50 million infectious diseases are registered annually, of which up to 90% of cases are ARVI and influenza.
Almost 90% of the population experience one of the respiratory infections of viral etiology at least once a year, which generally determines high morbidity and even affects the mortality rate [2].
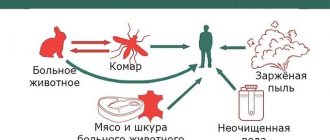
Such a high incidence of respiratory tract diseases is explained by a variety of etiological factors (influenza viruses, parainfluenza, adenoviruses, rhinoviruses, reoviruses, respiratory syncytial (RS) viruses, mycoplasmas, chlamydia, bacterial agents), as well as the ease of transmission of the pathogen and the high variability of viruses.
Differential diagnosis of influenza and ARVI is difficult due to the similarity of the clinical picture of these diseases, but it is quite possible. The main differences can be considered the initial signs of the disease, symptoms of intoxication, the nature of catarrhal symptoms and fever, the type of complications that develop, etc. The clinical diagnosis, confirmed by laboratory tests, determines the choice of therapy.
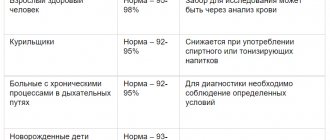
The clinical picture of ARVI and influenza depends on the causative virus (see table).
It should be noted that complications from ARVI, especially during an epidemic, are recorded in 20–30% of cases. The main causes of complications are disorders of the immune defense, leading to long-term insufficiency in the functioning of the immune system. A decrease in the body's antibacterial resistance leads to protracted periods of convalescence and creates the possibility of complications over a long period of time. A special place among complications is occupied by the so-called post-viral asthenia syndrome (PAS), which can develop in 65% of patients within 1 month from the onset of the disease. The leading symptoms of SPA are fatigue, emotional disturbances and various mental disorders.
The range of drugs used in the treatment of ARVI and influenza is wide and varied. It includes live and inactivated vaccines, chemotherapy drugs with etiotropic action, as well as drugs used for immunocorrective and pathogenetic therapy.
However, the course of influenza and other acute respiratory viral infections remains difficult to control. This is due not only to the polyetiology of these diseases, but also to the unique variability of viruses and the global nature of epidemics. The spread of ARVI largely depends on the environmental, socio-economic situation, the presence of allergic diseases in patients and a number of other factors.
Antiviral drugs
Chemotherapy
The mechanism of action of this group of drugs is based on the selective suppression of individual stages of viral reproduction, without interfering with the vital activity of the cell of the macroorganism. For respiratory infections, two groups of drugs are used - M2 channel blockers and neuroaminidase inhibitors, as well as ribavirin, which is active against the RS virus.
M2 channel blockers
In 1961, a symmetrical amine, amantadine, was synthesized, and then a number of its derivatives (rimantadine, midantan, deutiforin). In our country, rimantadine is widely used, which is used for the treatment and prevention of influenza caused by the type A virus. The effectiveness of this drug is 70–90%.
The antiviral effect is realized by blocking special ion channels (M2) of the virus, which is accompanied by a violation of its ability to penetrate cells and release ribonucleoprotein. This inhibits the most important stage of viral replication. In approximately 30% of cases, resistance to rimantadine may develop [6].
Rimantadine is available in the form of rimantadine in tablets of 50 mg and syrup for children from 1 to 7 years of age - algirem - 2 mg/ml. For therapeutic purposes, the drug is prescribed from the moment the first symptoms are registered. The duration of therapy should not exceed 5 days to avoid the emergence of resistant forms of the virus. As a preventative measure, rimantadine should be taken for at least 2 weeks.
Neuroamindase inhibitors
Drugs in this group are effective not only against type A influenza viruses, but also against type B viruses.
Neuroamindase (sialidase) is one of the key enzymes involved in the replication of influenza viruses. When neuroamindase is inhibited, the ability of viruses to penetrate healthy cells is impaired, their resistance to the protective effect of respiratory tract secretions is reduced, and thus the further spread of the virus in the body is inhibited. Neuroamindase inhibitors are able to reduce the production of cytokines (IL-1 and tumor necrosis factor), preventing the development of a local inflammatory reaction and weakening systemic manifestations of a viral infection such as fever, pain in muscles and joints, and loss of appetite [7].
Preliminary studies have shown that the effectiveness of such an inhibitor as a prophylactic agent is 70–80%. Taking these drugs can reduce the duration of the disease by 1–1.5 days (if you start taking the drug no later than 36–48 hours from the moment the first symptoms appear). At the onset of the disease and in its early stages, the average duration of viral replication is reduced by an average of 3 days, and the number of severe forms of ARVI and influenza, characterized by elevated temperature, by 85%. The drugs do not have a harmful effect on the central nervous system. However, it should be noted that it is not always possible to use them in the first 48 hours: due to the difficulties associated with the differential diagnosis of influenza and other acute respiratory viral infections.
Representatives of neuroamindase inhibitors are oseltamivir and zanamivir.
Oseltamivir (Tamiflu) is prescribed 75–150 mg 2 times a day for 5 days. For prevention - 75 mg 1 or 2 times a day for 4–6 weeks. In patients with creatinine clearance less than 30 ml/min, the dose is reduced by 2 times.
Zanamivir (Relenza) is a structural analogue of sialic acid, a natural substrate of influenza virus neuroamidase, and therefore has the ability to compete with it for binding to the active site. It is inhaled using a special device - a diskhaler. For therapeutic purposes, 10 mg is prescribed 2 times a day (with an interval of 12 hours) for 5 days, for prevention - 10 mg 1 time a day for 4-6 weeks. The inhalation route of administration has the advantage of providing a fairly rapid antiviral effect in the area of the primary source of infection.
Adverse reactions of this group of drugs account for no more than 1.5% of cases. Most often these are headache, dizziness, nausea, diarrhea, and sinusitis. Patients with obstructive bronchopulmonary diseases may develop bronchospasm.
Drugs active against other viruses
Ribavirin (virazol, rebetol), which acts on many RNA and DNA viruses, is used in aerosol dosage form to treat infections caused by the RS virus. It is assumed that the drug inhibits the early stages of viral transcription, disrupting the synthesis of ribonucleoproteins, messenger RNA, and blocking RNA polymerase. It is used inhalation using a nebulizer only in a hospital setting.
When taking ribavirin, bronchospasm, rash, and eye irritation may occur, not only in patients, but also in medical staff. In rare cases, leukopenia, insomnia, and irritability are observed. There is a risk of drug crystallization in the respiratory tract and endotracheal tubes. Has a teratogenic effect.
A promising antiviral drug is plenoconaril, recently developed in the USA. In vitro studies and animal experiments have revealed its activity against enteroviruses and rhinoviruses. Data from the first placebo-controlled studies indicate the effectiveness of the drug against respiratory infections and enteroviral meningitis [8].
In Russia, original antiviral drugs are used, created on the basis of domestic developments. The most widely known of them is arbidol. It has an inhibitory effect on influenza viruses type A and B and other respiratory viruses, the mechanism of which is not fully understood. It is believed that such an effect is associated with both the interferon-inducing and immunomodulatory properties of the drug. In particular, arbidol stimulates the activity of phagocytic cells. Available in tablets of 0.1 g. For medicinal purposes, 0.2 g is prescribed 3-4 times a day for 3-5 days. For prophylactic purposes, 0.2 g/day is used for 10–14 days.
Interferons
Interferons (IFNs) are among the regulators of immunogenesis. They are produced by various cells and not only implement the antiviral response, but also regulate immunological reactions. The main effects of interferons can be divided into antiviral, antimicrobial, antiproliferative, immunomodulatory and radioprotective.
Despite the diversity of the genetic material of viruses, IFNs suppress their reproduction at a stage required for all viruses: they block the onset of translation, i.e., the synthesis of virus-specific proteins. This may explain the universality of the antiviral action of interferon. Under the influence of interferon in the body, the activity of natural killer cells, T-helper cells, cytotoxic T-lymphocytes, phagocytic activity, the intensity of B-lymphocyte differentiation, and the expression of MHC type I and II antigens increases [1].
α- and β-interferons are used to treat viral infections. A good effect in treatment is achieved by the combined use of chemotherapy and IFN drugs.
β-interferon (betaferon) is available in powder form, in bottles containing 9.5 million units of IFN. For influenza, it is instilled or sprayed into the nasal passages at least 4–5 times a day [2].
Human leukocyte interferon is a mixture of interferons synthesized by leukocytes of donor blood in response to exposure to a viral inducer. The drug is administered by inhalation or an aqueous solution prepared from a dry substance in an ampoule or bottle is instilled into the nasal passages.
Viferon - recombinant interferon-α 2b - is available in the form of rectal suppositories and is used in the treatment of acute respiratory viral infections and influenza. Damage to cell membranes observed during the development of the infectious process is the reason for the decrease in the antiviral activity of interferon. Tocopherol acetate and ascorbic acid, which are part of Viferon, are membrane-stabilizing components, antioxidants, in combination with which the antiviral activity of recombinant interferon-α 2b increases 10–14 times [1].
The peculiarities of the administration of the dosage form ensure long-term circulation of interferon-α 2b in the blood.
The drug is used both in newborns and in adult patients with ARVI and influenza in age-specific dosages. Children under 7 years of age are prescribed Viferon-1, children over 7 years of age and adults - Viferon-2.
Interferon inducers
Exogenous interferon preparations are logically combined with the use of its inducers in clinical practice. They represent a very heterogeneous family of high- and low-molecular natural and synthetic compounds, united by the ability to induce in the body the formation of its own (endogenous) interferon α- and β-interferons in different proportions by leukocytes, macrophages, epithelial cells, as well as tissues of the spleen and liver , lungs, brain. The drugs penetrate the cytoplasm and nuclear structures and activate the synthesis of “early” interferons. Helps correct the immune status of the body [3].
Amiksin is a low molecular weight synthetic inducer of endogenous aromatic interferon, belonging to the class of fluorenones. The main structures that produce interferon in response to the administration of amixin are intestinal epithelial cells, hepatocytes, T-lymphocytes, and granulocytes. In human leukocytes, amixin induces the formation of interferon, the level of which in the blood is 250 U/ml. After taking amixin orally, the maximum interferon in humans is determined sequentially in the intestines, liver, and blood after 4–24 hours [2].
When treating influenza and acute respiratory viral infections, amixin is prescribed in the first hours of the disease; 5–6 tablets are enough per course. For the purpose of prevention, it is prescribed once a week for 4–6 weeks.
Cycloferon is a low-molecular-weight inducer of IFN-α, which determines a wide range of its biological activity. It quickly penetrates cells, accumulating in the nucleus and cytoplasm. Cycloferon intercalates cell DNA, which is responsible for the mechanism of its interferon-inducing activity [3].
Cycloferon quickly penetrates the blood. There is low binding to blood proteins and at the same time widespread distribution in various organs, tissues, and biological fluids of the body.
Due to the fact that cycloferon is a low-molecular drug, it easily crosses the blood-brain barrier, causing the formation of IFN in the brain. Cycloferon is quickly eliminated from the body: 99% of the administered drug is eliminated unchanged by the kidneys within 24 hours.
Cycloferon is well tolerated by patients and is prescribed from the first day from the onset of the disease in tablet form or parenterally [4].
Ridostin is a high molecular weight IFN inducer of natural origin. Ridostin is a double-stranded RNA obtained from the lysate of the killer yeast Saccharamyces cervisiae.
Systemic administration of ridostin stimulates the production of early IFN. The maximum accumulation of IFN in serum is observed 6–8 hours after injection; after 24 hours it is not detected in the bloodstream [1].
The drug exhibits a pronounced immunomodulatory effect. It stimulates T-cell and humoral immunity, proliferation of bone marrow stem cells and phagocytic activity of macrophages and neutrophils in peripheral blood. Ridostin increases the level of corticosteroid hormones; used for the treatment and prevention of influenza and other acute respiratory viral infections.
Currently, the drug dibazol, used for the treatment and prevention of influenza and ARVI, is undeservedly forgotten. Dibazol has immunomodulatory activity and induces the production of endogenous interferon. For prevention, 1 tablet (0.02–0.05 g) is prescribed once a day for 3–4 weeks; for treatment, 1 tablet 3 times a day for 5 days.
Indispensable in the treatment of influenza and ARVI are complex drugs such as Grippostad, Rinza, Theraflu, Fervex, as well as drugs for external and local use - Doctor Mom cold ointment, Tussamag cold balm.
Despite the variety of drugs presented for the treatment of acute respiratory viral infections and influenza at the present stage, the choice of a drug remains an urgent task for the practicing physician. The choice of tactics for prescribing and managing a patient with ARVI or influenza is directly related to the severity of the infectious process, the form of the disease and the presence of complications. The success of treatment depends on the correct assessment of the patient’s condition and early initiation of treatment.
O. A. Melnikov , Candidate of Medical Sciences L. V. Averkieva “GUTA-Clinic”, Moscow
Antibiotics for complications of influenza
Depending on the severity and type of complications, the use of the following antibacterial groups of drugs is recommended for influenza:
- Penicillins are used to treat consequences in the form of otorhinolaryngological diseases, damage to the lower and upper respiratory tract.
- Fluoroquinolones are effective in the development of symptoms of pharyngitis, sinusitis, otitis, and sinusitis. Representatives of Oflosaccin, Ciprofloxacin and others.
- Cephalosporins are prescribed for prolonged and acute flu, when the risk of complications is high.
- Levomycetin agents have a wide spectrum of action. This group of drugs has a strong therapeutic effect, so it is used strictly for its intended purpose. Self-medication can cause negative consequences.
- Macrolides are indicated when upper respiratory tract infections are associated with influenza.
- Anti-tuberculosis antibiotics - the pharmacological activity of the group is aimed at combating the causative agent of tuberculosis and preventing complications.
- Aminoglycosides are effective for severe influenza infection. Help prevent infection of the bloodstream and peritonitis. They have pronounced toxicity and are used strictly as indicated.
- Antifungal drugs - used in case of fungal pathology.
- Actinomycetes - the main indication for use is a neoplasm in the patient.
Why are antibiotics dangerous?
Treatment with antibiotics often causes a number of adverse reactions:
- The first and most common is intestinal dysfunction. Digestive disorders are due to the fact that antibacterial drugs affect not only pathogenic bacteria, but also those that help the intestines process food. By taking antibiotics, we upset the balance of microflora, resulting in loose stools and increased gas production.
- The second most common unpleasant effect from taking drugs is nausea, which turns into vomiting. It occurs due to the fact that dead bacteria release toxins, which, when released into the blood, cause poisoning. Most often, vomiting occurs while taking bactericidal antibiotics. If the patient suffers from vomiting, he should inform the doctor about this in order to replace the type of drug with a bacteriostatic one. This will reduce the level of toxins and relieve painful nausea.
- Weakened liver function is the third side effect of taking antibiotics. The filtering organ, conducting blood flow through itself, becomes an accumulation of toxic substances. This exposes liver cells to destruction. Therefore, while taking antibiotics, it is strictly forbidden to drink alcohol - the consequences can be severe, including complete organ failure.
Features of the use of antibiotics for influenza
There are some features of taking antibacterial drugs for the flu, these are:
- The medicine must be taken strictly as prescribed, observing the permissible dosage and duration of the course.
- You cannot stop taking the drug on your own to avoid the disease becoming chronic.
- The prescription of an antibiotic for influenza pathology must be fully justified by the doctor.
- In parallel with antibiotic therapy, it is recommended to use probiotics. This is necessary to maintain normal microflora.
- During treatment, you should drink more fluids and eat dairy products.
- The patient's diet must be balanced. It is important to take additional vitamin complexes and follow preventive measures when infections develop.
Don't repeat at home
An antibiotic is a powerful medicine and should always be prescribed by a doctor. For more than two decades, many pharmacies, in an effort to increase revenue, freely sold prescription drugs, except for narcotic and psychotropic drugs. This led to the fact that many doctors forgot how to fill out prescription forms, writing prescriptions on pieces of paper without even stamping them. And patients bought antibacterial, also known as antimicrobial, drugs for self-medication. Control has only tightened in the last two years.
“Even before I started working at the Fantasy Children’s Clinic,” says pediatrician Victoria Alipova, “a child was brought to the appointment who complained of abdominal pain and bowel movements. The medical history showed that the boy had been treated with antibiotics 12 times over the past year for every cold, including ARVI, when such medications are useless. For the first time, the doctor prescribed an antibiotic, and then the child’s mother acted by analogy. It was enough to stop the drug, and the problem with the intestines would normalize. Children can take antimicrobials in the form of syrups or suspensions even from birth, but only according to indications determined by the doctor. Many doctors prescribe such medications for any reason.”
Antibiotics have many side effects. First of all, they destroy the intestinal microflora: diarrhea, vomiting, possible colitis, liver and kidney dysfunction, and allergies. In such cases, probiotics or other drugs that normalize the functions of the gastrointestinal tract are often prescribed in parallel. However, urologist Rinaz Kamaletdinov says that the clinical recommendations do not indicate that such drugs can stabilize the intestinal microflora against the background of antibacterial therapy. And in each case of illness, only a specialist can make a decision on the type of therapy:
“Treatment with antibiotics should be carried out by a doctor,” Dr. Kamaletdinov is sure. - Even if similar symptoms reappear, you should not take the pills left over from your previous illness. You can consult a doctor online or by phone. In urology, different types of antibiotics are used, most often fluoroquinolones, especially levofloxacin. It is often necessary to change the pharmacological group, dose, duration and schedule of administration. For example, a patient with bacterial prostatitis caused by Escherichia coli was given one type of antibiotic. Treatment requires 28 days, but symptoms returned in the 3rd week. It turned out that a second infection appeared in the body, and E. coli developed resistance to the drug. I had to additionally prescribe a drug of a different spectrum.”