A woman's uterus consists of two layers: the inner basal layer and the outer functional layer. It is the outer layer that reacts to hormonal changes in the cycle and is shed monthly with menstruation. In the case of hormonal disorders, the functional endometrium grows, which is a pathology, and if left untreated, there is a risk of the appearance of atypical cells, which is a precancerous disease.
The main reason for excessive growth of the endometrium is the increased production of estrogen and lack of progesterone. Most often, this pathology is diagnosed in premenopausal women and teenage girls. Both conditions are associated with hormonal changes in the body. Endometrial hyperplasia is characterized by an anovulatory cycle—the absence of ovulation.
Danger of HGE
Treatment of endometrial hyperplasia should not be delayed. The fact is that, under certain conditions, GPE can become a catalyst for the development of oncological processes.
Another dangerous consequence of the disease is infertility, since pathological changes occurring in the endometrium prevent the embryo from attaching to the wall of the uterus. As HPE progresses, the chances of pregnancy decrease further. In addition, the risk of miscarriage and premature birth increases.
Endometrial hyperplasia is characterized by prolonged menstruation, a significant amount of menstrual flow and intermenstrual bleeding. As a result, patients with HPE are more likely to develop anemia due to constant blood loss.
Sometimes, after treatment, the disease may return. According to statistics, relapses occur on average in 32% of cases after conservative therapy and in 12% of cases after surgery. This is due to repeated hormonal imbalances.
Intrauterine synechiae
Intrauterine synechiae are adhesions in the uterine cavity, which very often interfere with the implantation of a fertilized egg, which leads to infertility. The causes of intrauterine synechiae can be inflammatory diseases of the pelvic organs, as well as intrauterine interventions (abortion, curettage for a missed pregnancy, surgical interventions on the uterus).
The presence of intrauterine synechiae is safe for life, and can manifest itself as scanty menstruation or its absence. However, if pregnancy issues arise, intrauterine adhesions can be a serious problem, especially with common forms and severe damage to the uterus./p>
Forms of the disease
Based on the cellular composition (histologically), glandular and glandular-cystic GPE are distinguished.
Atypical endometrial hyperplasia and hyperplasia in polypous form are also distinguished.
According to the WHO classification, hyperplasia occurs:
- simple without atypia;
- simple with atypia;
- complex.
Glandular hyperplasia
Glandular hyperplasia of the endometrium is characterized by the proliferation of tissue mainly due to glands that change shape (become tortuous, form loops) and increase in volume. As a result, the thickness of the functional layer of the endometrium increases, and there is no characteristic distinction between the basal and functional layers. The location of the glands changes: if normally they are located singly and relatively evenly, then with glandular hyperplasia they can be in close contact, forming groups.
Let us recall that the basal layer is a layer of cells directly adjacent to the myometrium and having a high ability to regenerate, due to which active proliferation becomes possible. The functional layer lining the uterine cavity under the influence of hormones grows during the first and second phases of the menstrual cycle, after which, if pregnancy does not occur, it is rejected during menstruation. During one cycle, its thickness increases by an average of 6-7 mm.
Patients with glandular endometrial hyperplasia complain of menstrual irregularities such as hypermenorrhea and menorrhagia. As a result of prolonged blood loss, anemia may develop. It is also possible to develop infertility.
Within this type of hyperplasia there are:
- The active form, when active cell division occurs at high levels of estrogen.
- The chronic form, when estrogen levels are not high, and under the influence of hormones, mitoses occur quite rarely.
Glandular cystic hyperplasia
Glandular-cystic hyperplasia of the endometrium is not always isolated separately, however, unlike the previous type, cysts are present in the endometrium. The reason for their formation is that with the active division of cells localized in the area of the mouth, a blockage of the gland occurs, from which mucus can no longer be freely released. At this site, a cavity filled with fluid is formed - a cyst.
Basal hyperplasia
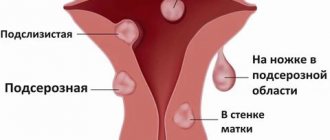
A form of hyperplasia characterized by the growth of the basal layer, which can be focal or diffuse. In the first case, local tissue proliferation causes the formation of an endometrial polyp in the uterus.
Against the background of the growth of the basal layer of the uterine mucosa, the functional layer gradually becomes thinner, and the characteristic cyclic changes in it do not occur so noticeably.
Adenomatous hyperplasia
With adenomatosis, not only the growth of the endometrial glands occurs, but also a change in their structure. Normally, in the tissue, the glands are separated from each other by the epithelium, but with atypical hyperplasia they are grouped, forming different structures. There may be epithelial cells inside the gland or the appearance of one gland inside another.
Pathological changes can occur in each of the layers of the mucous membrane separately, or in both simultaneously. In the latter case, the risk of malignancy increases markedly.
Why does glandular hyperplasia of the uterus occur in menopausal women?
The main cause of any type of hyperplasia is hormonal imbalance, so this disease is especially common in menopausal patients.
Normally, after ovulation, a woman produces gestagen hormones, which prevent tissue proliferation and prepare the body for the onset of menstruation. If this does not happen, the body continues to produce estrogens, which cause mucosal growth.
In the cramped uterine cavity, glandular cells have nowhere to grow, so they begin to grow “into themselves,” forming deformed convoluted glands with cystic contents (secretion). As a result, the uterine layers thicken and are rejected, the process is accompanied by bleeding. During this period, you can observe blood with clots consisting of immature cells of the inner uterine layer.
Pathology can be provoked by inflammation in the uterus, myomas and fibroids, sudden refusal of hormonal contraception, surgical abortions and curettage, late menopause.
Symptoms of endometrial hyperplasia
The main signs of endometrial hyperplasia in women of reproductive age are menstrual irregularities, which include:
- menorrhagia. The patient complains not only that menstruation has become longer, but also that the volume of bleeding has increased;
- algodismenorrhea. During menstruation, a woman experiences intense pain localized in the lower abdomen;
- metrorrhagia. In this case, intermenstrual uterine bleeding occurs;
- change in the duration of the menstrual cycle;
- infertility.
In addition, women develop anemia associated with prolonged blood loss.
The main symptom of endometrial hyperplasia during menopause is spotting from the genital tract. This is most often associated with an endometrial polyp or a malignant disease of the uterus.
During the period of hormonal changes in the body, the likelihood of developing pathologies of the reproductive system increases. Of particular danger is the risk of malignant transformation of endometrial hyperplasia.
In the absence of obvious signs of the disease, timely diagnosis of the pathology can be difficult, and therefore women are recommended to undergo an annual preventive examination by a gynecologist. In particular, regular examination is recommended for patients who:
- are in the age group over 45 years old;
- have problems with excess weight;
- suffer from arterial hypertension;
- have diabetes;
- with infertility and absence of childbirth;
- with polycystic ovary syndrome;
- have a family history of endometrial cancer.
How does healing occur?
6–7 weeks after a session of photodynamic therapy, the mucous membrane heals without scars. A healthy uterine epithelium is formed.
Within six months, all patients undergo 3-fold monitoring, which includes:
- Ultrasound with a vaginal probe,
- conducting a scarification biopsy of the endometrium of the uterus with examination using liquid cytology.
In the future, you will need to visit a gynecologist once every six months for preventive examinations.
Diagnostics
To confirm the diagnosis, the doctor uses laboratory and instrumental examination methods.
In laboratory tests, it is possible to record estradiol levels exceeding the reference interval for a given day of the cycle, and a reduced level of progesterone in the second phase of the cycle.
Instrumental examination methods play an important role in the diagnosis of endometrial hyperplasia and polyps.
Ultrasound of the pelvic organs
Reveals a discrepancy between the echographic picture of the endometrium and the expected day of the menstrual cycle. With endometrial polyps, in the projection of the median uterine echo (M-ECHO), local formations of a different acoustic density can be determined. The combination of ultrasound examination with contrasting of the uterine cavity (sonohysterography) allows for a more detailed study of intrauterine pathology.
Pipelle endometrial biopsy
allows you to take a sample of the endometrium for histological or immunohistochemical examination. This procedure is absolutely safe, does not require anesthesia and is performed in a doctor's office.
Hysteroscopy
Hysteroscopy with histological examination of the endometrium is the gold standard for diagnosing intrauterine pathology. Many specialists have noted the positive role of hysteroscopy at the stage of preparation for ART programs. The widespread introduction of outpatient (office) hysteroscopy has expanded the diagnostic potential, eliminating the need for cervical dilatation and, as a consequence, the use of general anesthesia. However, in situations where it is necessary to remove a layer of hyperplastic endometrium or the polyp is large, standard hysteroscopy under intravenous anesthesia retains its place in the arsenal of medical care in reproductive medicine.
Histological examination of the endometrium
It is carried out by a pathologist and makes it possible to judge the nature of GPE, allowing the attending physician to select the treatment method that is most suitable for a particular patient. In the vast majority of cases, rehabilitation after intrauterine intervention is either not required at all or takes 2-3 months, after which the couple is recommended to begin an ART program. In difficult cases, when a precancerous process in the endometrium cannot be excluded, consultation with an oncologist is necessary;
Immunohistochemical study of the endometrium
In recent years, IHC has become widespread. This method makes it possible to identify a variety of biological markers in endometrial tissue, the analysis of which can help in determining the functional state of the endometrium. It has been proven that in the presence of HPE there is increased expression of estrogen receptors and decreased expression of progesterone receptors. The expression of various markers of cell proliferation increases.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Transvaginal ultrasound of the uterus and appendages | 2 800 |
| Hysteroscopy (diagnostic, therapeutic) | 47 500 |
| Endometrial ablation | 60 000 — 85 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Treatment of GPE
Treatment of GPE depends on its form, which is confirmed by pathomorphological examination of material from the uterine cavity, taken during separate diagnostic curettage or endometrial biopsy.
Treatment of simple endometrial hyperplasia
Hysteroscopy with endometrial curettage cannot be considered as a reliable treatment method, since relapses after 6 months occur in half of the patients. In addition, in 10% of cases, simple hyperplasia progresses to complex hyperplasia.
This is why anti-relapse therapy is necessary.
Treatment of HPE without atypical cells is based on hormonal therapy. For this purpose, gestagens can be prescribed, but in the future the risk of relapse cannot be excluded.
A good effect is observed when installing a levonorgestrel-releasing intrauterine system.
In some cases, combined oral contraceptives may be used.
As a rule, monophasic low-dose COCs are used, which include gestodene, levonorgestrel, dienogest or desogestrel, which can also be prescribed continuously.
Using oral contraceptives for one year reduces the risk of endometrial cancer or hyperplasia by 40-50%, and this effect lasts up to 15 years.
If conservative treatment is ineffective, ablation (removal) of the endometrium can be performed.
Treatment of complex endometrial hyperplasia
Treatment of complex GPE (adenomatosis) should be carried out under the supervision of a gynecological oncologist. Drugs are prescribed to suppress the production of natural hormones - analogues of gonadoliberin hormones. Sometimes they are used in combination with the installation of a levonorgestrel-releasing intrauterine system. To assess the results of treatment, control is carried out after 3-6 months, and therefore, 3-4 weeks after completion of the course of treatment, a separate diagnostic curettage or pipette biopsy is performed.
GnRH analogues turned out to be most effective in comparison with COCs and progestins based on the results of long-term treatment in preventing relapses of proliferative diseases of the uterus.
According to indications, patients of the reproductive period can also be prescribed norethisterone acetate, linestrenol, medroxyprogesterone acetate.
In some cases, endometrial ablation is recommended. After this procedure, women planning a pregnancy, in the absence of contraindications to ovarian stimulation, may be recommended the surrogacy procedure.
Treatment of atypical endometrial hyperplasia
For patients planning IVF, atypical GPE is a contraindication to the program due to the high oncological risk.
Treatment for this form of GE is long-term. Drugs are prescribed that block the production of hormones by the pituitary gland and, accordingly, the ovaries. Sometimes they are also used in combination with the installation of a levonorgestrel-releasing intrauterine system. Careful diagnosis is necessary both during therapy and after its completion. Hysteroscopy with separate diagnostic curettage or pipel biopsy is performed.
Treatment is carried out by a gynecological oncologist.
A new method such as photodynamic therapy of the endometrium can also be used.
When choosing therapy, it is necessary to take into account the ovarian reserve. If it is reduced, the use of medroxyprogesterone acetate and levonorgestrel-releasing intrauterine system is not recommended.
It should also be taken into account that there is no data on premature depletion of ovarian function during the use of GnRH analogues.
In some cases, a hysterectomy (hysterectomy) may be performed, which is a necessary measure in case of untimely diagnosis and improper management of patients with endometrial hyperplasia, especially in combination with fibroids or adenomyosis.
According to statistics, hysterectomy is prescribed:
- in the USA in more than 30% of cases (while the age of 3 out of 4 patients is below 49 years, and half of the women are under forty);
- in the UK in 20% of cases;
- in Russia in 25-38% of cases.
How does the photodynamic therapy procedure work?
- After a thorough examination, the patient is given the photosensitizer drug “Fotoran” or “Photodinazine” and its analogues intravenously. This substance selectively accumulates in old, atypical, damaged and inflamed cells of the uterine mucosa and almost does not accumulate in healthy ones.
- After 2.5 - 3 hours according to the protocol developed jointly with the Center for Laser Medicine of the First St. Petersburg State Medical University. acad. I.P. Pavlova (scientific director of the center, doctor of medical sciences, prof. Petrishchev N.N., researcher Grishacheva T.G.), using a special method that we have developed, irradiation of the uterine cavity is carried out with an intrauterine balloon light guide.
| Disposable intrauterine light balloon for photodynamic therapy. |
- Such a light guide allows you to evenly distribute the light of the laser beam and obtain a full therapeutic effect.
- In my practice, I use only disposable intrauterine light cylinders. Using a new cylinder each time ensures that it glows properly at the specified power, which is critical for achieving the desired photodynamic effect and protects against the risk of infection.
- To achieve an adequate photodynamic effect, I develop a treatment protocol for each patient individually.
- Under the influence of laser radiation in the red spectrum, the photosensitizer enters into a photochemical reaction with oxygen to form so-called active singlet oxygen, a powerful oxidizing agent that damages the membranes of atypical cells and causes their death.
- Singlet oxygen is also an aggressive environment for bacterial and viral infections and destroys them. This allows one procedure to treat concomitant inflammatory diseases of the uterus, such as endometritis.
- Since each atypical cell accumulates a photosensitizer, PDT eliminates all areas of adenomatosis. The photosensitizer is removed from healthy cells 1-1.5 hours after administration, and they are not damaged during the treatment.
It is this selective effect that ensures complete removal of atypical cells and hyperplastic endometrium and recovery after the procedure.
- After PDT, the body launches natural mechanisms for recycling damaged atypical cells and their decay products.
- Healing after PDT occurs with the formation of a healthy and complete endometrium of the uterus.
Prevention of endometrial hyperplasia
To reduce the risk of developing endometrial hyperplasia, it is recommended to visit an obstetrician-gynecologist annually.
In addition, you should:
- normalize your diet and avoid eating foods that contain dyes and preservatives;
- reduce weight;
- normalize glucose and insulin levels;
- lead a fairly active lifestyle, without overloading yourself with exhausting workouts;
- give up bad habits (in particular, drinking alcohol and smoking);
- select effective means of protection against unwanted pregnancy to avoid abortion. Often women opt for combined oral contraceptives. However, you need to pay attention to the fact that only the attending obstetrician-gynecologist can prescribe them after conducting the necessary examination.