Ascites - what is it?
Ascites is a variety of complications caused by a number of diseases.
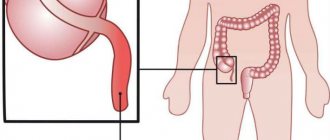
This pathology reveals itself as the accumulation of a large amount of liquid mass inside the peritoneal cavity. Hence the second name “edema of the abdomen”. The accumulated liquid mass increases the volume of the abdomen, causing unpleasant symptoms and secondary dysfunctions of the organs of the peritoneal cavity.
In such a condition, medical intervention is simply necessary, especially if the liquid mass accumulates rapidly.
Manifestations
A small amount of liquid mass accumulated in the abdominal cavity does not reveal itself in any way. How to determine the onset of the disease, since there are no symptoms? Ultrasound comes to the rescue here.
As the disease progresses, a feeling of heaviness appears in the abdomen, and the lower part is subject to dull aching pain. Next comes difficulty breathing, after which there is indigestion in its various varieties, and urination is impaired.
A severe form of pathology can dramatically worsen your health. The state of health leaves much to be desired:
- Unpleasant sensations in the stomach become the norm;
- Shortness of breath appears;
- An umbilical hernia develops;
- Legs swell;
- Internal organs are compressed.
Medical practice is faced with the fact that some patients accumulate up to twenty liters of fluid. As a result, they have:
- Increased pressure inside the peritoneum;
- The diaphragm becomes pressed into the chest cavity;
- Significant difficulty breathing;
- Heart failure develops.
If the order of things is not restored, the following are possible:
- Impaired drainage of the lymphatic system;
- The occurrence of impaired lymphatic drainage in the legs;
- Swelling of the extremities;
- Outflow of lymph to internal organs.
The result of such changes can be disastrous. Atypical cells penetrate from the affected lymph nodes to other organs.
Pathology in a small form can be determined during a medical examination: the abdomen is enlarged, it is saggy when a person is standing, or flattened when a person is lying down. In thin patients, the navel often protrudes.
Determining the pathology at the very beginning of its development is important, since its moderate form is diagnosed in almost half of patients in the early stages of oncology.
Bloating: can the problem be solved?
Bloating is one of the most common problems of the digestive system, with which patients around the world regularly consult general practitioners, internists and gastroenterologists. Up to 30% of adults experience some degree of bloating during their lifetime. In some diseases (for example, irritable bowel syndrome), the prevalence of bloating reaches 85-90%.
What is bloating? Despite the apparent simplicity of the question, it must be asked. The fact is that often the doctor and the patient, when talking about bloating, mean different symptoms by this term. According to modern concepts, bloating is a feeling of fullness (fullness) and bloating of the abdomen, excessive gas formation and discharge of gases. But a common increase in abdominal circumference, visible even from the outside, is identified as a separate symptom - abdominal distension. Often both of these symptoms are observed in one person, and quite reasonably they are combined into the common complaint “bloating.”
Where do gases come from in the gastrointestinal tract?
Gas formation is a normal process that occurs daily in the body of even a healthy person.
Some gases (according to some sources, up to 60%!) enter the gastrointestinal tract by swallowing air. This occurs when eating and drinking (especially when eating in a hurry), talking while eating, using chewing gum, lozenges, etc. The swallowing of air increases in some diseases, when the swallowing process is impaired, in pathology of the nasopharynx, etc.
Gas is also formed in the intestines during chemical reactions: for example, hydrochloric acid of the stomach, interacting with the alkaline contents of the duodenum, causes the formation of carbon dioxide. In addition, intestinal bacteria can break down carbohydrates that are not absorbed in the small intestine to form various gases, primarily hydrogen, methane, ammonia, hydrogen sulfide and carbon dioxide.
Finally, a small amount of gases enters the intestinal lumen through the walls of blood vessels.
Normally, the body always maintains a balance of gases - the resulting gas is either absorbed by the intestinal wall or excreted through the rectum in free form or with feces. As a result, the average healthy person's intestines contain 200 ml of remaining gas.
If there are disturbances in any of the links in the chain, the formation of gases -> absorption of gases -> excretion of gases results in excessive accumulation of gases in the intestinal tube, which leads to unpleasant symptoms.
The main mechanisms of development of bloating
Bloating is a difficult symptom . Not easy for the patient as it can be a problem for many months and years. Difficult for a doctor, since there is a whole group of causes and mechanisms of its development, which a medical specialist must clarify before prescribing the correct treatment.
The first reason is an increase in the amount of gas in the intestines. This may happen due to:
- excessive swallowing of air (see above);
- consumption of foods rich in gases (carbonated drinks, kvass, beer, mineral waters);
- increased formation of gases by bacteria of the small and large intestines.
Let's pay a little attention to the last point. Normally, there are few bacteria in the small intestine, but in the large intestine their number is greatest in the entire gastrointestinal tract. Increased gas formation by small intestinal bacteria occurs if the patient has the so-called bacterial overgrowth syndrome - a common condition after treatment with antibiotics, against the background of chronic diseases or as a consequence of operations. In this case, carbohydrates that enter the small intestine with food are partially broken down by excessively multiplied bacteria. As a result, an increased amount of gas is formed, unabsorbed split carbohydrates “attract” liquid into the intestinal lumen - patients experience bloating, often in combination with loose stools.
In the colon, a large number of bacteria is the norm, and increased production of gases by them is observed in the case of excess intake of carbohydrates from food.
The second cause of bloating is a violation of the removal of gases from the intestines.
This can occur with constipation of any origin, or with dysfunction of the rectal muscles.
The third mechanism is the increased sensitivity of intestinal receptors to stretch, the so-called viceral hypersensitivity. This mechanism has been described in patients with irritable bowel syndrome. Its essence lies in the fact that even a slight increase in the amount of gases or their normal amount is perceived by the sensitive nerve endings in the intestines as excessive, which leads to the appearance of unpleasant symptoms.
The fourth mechanism is described to a greater extent for abdominal stretching, i.e. visible increase in abdominal circumference after eating . The intake of food always requires additional volume in the abdominal cavity. Normally, the body “provides” this volume by raising the diaphragm. With abdominal distension, the volume of the abdominal cavity increases due to the relaxation of the muscles of the anterior abdominal wall, it protrudes, creating a feeling of a bloated abdomen.
Conditions and diseases that cause bloating
A significant proportion of cases of bloating have a nutritional cause, i.e. associated with the nature of nutrition. The fact is that when certain carbohydrates predominate in the diet, they become a source of nutrition for colon bacteria. We are talking about non-absorbable carbohydrates, such as fructans and galactans, found in various vegetables, fruits, legumes, nuts, and grains. Excess fructans and galactans in the diet leads to increased formation of gases, most often a few hours after eating, in the evening.
Bloating can be one of the early signs of pregnancy.
Finally, some illnesses may present as an unpleasant feeling of bloating. Among the most common reasons are:
- irritable bowel syndrome;
- functional or secondary constipation;
- lactase deficiency and fructose intolerance;
- celiac disease;
- functional dyspepsia;
- any diseases and conditions accompanied by the development of bacterial overgrowth syndrome;
- parasitic diseases and helminthiasis.
More rare causes include inflammatory bowel diseases (Crohn's disease, ulcerative colitis), intestinal tumors, chronic pancreatitis with exocrine pancreatic insufficiency, diabetes mellitus, systemic scleroderma, ascites, etc.
Diagnostic search for bloating
Collecting complaints, a detailed description of the time, conditions and possible causes of bloating is an important step towards finding the correct diagnosis. So, the patient may say that bloating occurs only after eating certain foods, or this symptom is observed only when stool is retained (constipation).
Laboratory diagnostics is aimed at excluding an inflammatory process (stool analysis for fecal calprotectin), polypoid and tumor formations (stool occult blood analysis) in the intestine, parasitic invasion (stool analysis for protozoan cysts and helminth eggs, determination of Giardia antigen in stool, etc. .). In young people with suspected celiac disease, antibodies specific to this disease are determined in the blood.
Patients with suspected lactase deficiency and fructose intolerance undergo a hydrogen breath test with lactose and fructose, respectively.
If there are indirect signs of bacterial overgrowth syndrome, it is possible to perform a hydrogen breath test with lactulose.
For individuals with chronic pancreatitis, it is important to rule out exocrine pancreatic insufficiency, which may cause bloating and associated bowel movements. In this case, the activity of chymitropsin or the content of pancreatic elastase in the feces is assessed.
In order to exclude organic pathology of the gastrointestinal tract, the doctor may recommend performing gastroscopy, colonoscopy and ultrasound examination of the abdominal organs.
Treatment for bloating
To date, there is no universal remedy for treating bloating. Many patients who have been bothered by this unpleasant symptom for a long time are usually convinced of this after several visits to specialists. This is due to the existence of different mechanisms for the occurrence of bloating and increased gas formation in different individuals. In this regard, it is very important, before starting treatment, to understand the causes of this condition and to identify the most likely mechanism (or mechanisms!) of its development in a particular patient.
What methods of correcting bloating can be effective?
1) Diet therapy.
- Persons who frequently chew chewing gum or suck on lollipops and candies are advised to limit their use to minimize air ingestion;
- Carbonated drinks should be limited or eliminated from the diet;
- Patients diagnosed with lactase deficiency should use low-lactose or lactose-free foods, which usually completely solves the problem of bloating;
- The appearance of bloating after eating certain foods is not uncommon, and in this case, a diet that limits or excludes the provoking food usually helps;
- In more complex cases, when food definitely causes bloating, but it is impossible to identify a specific provoking food, a low FODMAP diet can be useful. On the one hand, it is a diagnostic tool, since it allows you to accurately identify poorly tolerated foods, and on the other hand, it is a therapeutic method, since it reduces the severity of bloating and increased gas formation.
2) Physical activity.
Research has proven that physical activity helps reduce the severity of bloating. Even low or moderate physical activity is effective - walking, running, cycling, etc. This is due to the fact that these exercises accelerate the movement of feces through the colon and thereby contribute to faster evacuation of gases.
Strengthening the muscles of the anterior abdominal wall can help patients with abdominal distension, i.e. increase in abdominal circumference after eating.
3) Drugs - regulators of intestinal motility.
These medications accelerate the movement of feces through the colon, facilitating faster evacuation of gases. The greatest effectiveness was observed in persons with functional constipation.
4) Means for correcting stool.
Since bloating often accompanies patients with constipation, one of the ways to treat it is to normalize stool through the use of so-called “mild” laxatives: soluble dietary fiber and some osmotic laxatives. In addition, soluble dietary fiber has a positive effect on the intestinal microflora/microbiota.
5) Antispasmodics.
The use of various antispasmodics, according to clinical studies, reduces the severity of symptoms of bloating in some patients.
6) Probiotics.
The use of various drugs containing bacterial cultures, according to clinical studies, reduces the severity of symptoms of bloating in some patients (25-30%).
7) Antibiotics.
Patients whose abdominal bloating is due to small intestinal bacterial overgrowth may benefit from treatment with certain antibiotics.
 Auxiliary drugs.
Auxiliary drugs.
Antifoaming agents and sorbents can have an additional effect on bloating.
9) Antidepressants.
Since one possible mechanism for bloating is increased sensitivity of intestinal receptors to gas distension, antidepressants may have an effect. However, unlike irritable bowel syndrome, for which this is the leading mechanism, and therapy with antidepressants is highly effective, drugs in this group do not always work for bloating.
Forecast for bloating
If the patient does not have serious diseases for which bloating is only one of the symptoms (oncological pathology, cirrhosis of the liver with ascites, etc.), then the prognosis is usually favorable. Correctly selected therapy allows you to get rid of a disturbing unpleasant symptom. In some cases, for example, with a relapse of bacterial overgrowth or a change in diet, bloating may reappear.
Causes
The basis for the development of the disease is pathology: during the normal functioning of the peritoneal cavity, no significant amount of liquid mass is discharged. It is only insignificant, just to avoid adhesions from sliding intestinal loops. The liquid released for this purpose constantly flows back.
When the usual operation of this mechanism is disrupted, the function of secretion of the liquid mass is destabilized, as well as the function of its outflow. The consequence of such destabilization is the accumulation of excess liquid mass inside the abdomen.
Causes of pathology in adults
In many cases, pathology develops as a symptom of a number of diseases, including:
- Portal hypertension;
- Cirrhosis;
- Hepatitis;
- Thrombosis of the liver veins.
It is possible that the cause of the pathology is blood oncology, as well as pathologies whose nature has nothing in common with the tumor.
Heart failure can also cause pathology. Problems associated with lymph circulation and the activity of organs such as the thyroid gland and kidneys can also cause pathology.
Protein deficiency
What causes fluid to accumulate?
With ascites, a pathological accumulation of fluid occurs in the abdominal cavity. The fact is that in some diseases the regulation of water-salt metabolism and normal fluid circulation in the abdominal cavity are disrupted. The reason may be:
- Oncological diseases: secondary peritoneal carcinomatosis, lymphoma and leukemia, metastases in the hepatic portal area, primary mesothelioma.
- Diseases of the liver and its vessels: liver cancer, portal hypertension, liver cirrhosis, veno-occlusive disease, Budd-Chiari disease.
- Peritonitis (inflammation of the peritoneum) of various origins: pancreatic, fungal, parasitic, tuberculous.
- Congestive heart failure, constrictive pericarditis.
- Other diseases: ovarian tumors and cysts (Meigs syndrome), pancreatic cyst, Whipple's disease, sarcoidosis, systemic lupus erythematosus, myxedema.
Euroonco treats ascites of various origins. But since our main work is related to the treatment of malignant neoplasms, a significant part of our patients are cancer patients.
Diagnostic methods
A certain amount of accumulated liquid mass (more than half a liter) can be determined during a medical examination. To confirm a preliminary diagnosis, an ultrasound is necessary.
The main problem is not to detect the liquid, but to identify the cause of its accumulation. Only then will the treatment be effective. To do this, it is necessary to conduct laboratory tests, namely:
- Blood clotting test;
- Biochemistry analysis;
- Analysis of ascitic fluid obtained during laparocentesis
Symptoms
Symptomatic manifestations of the disease depend on three main factors - the cause, the volume of accumulated liquid mass, and the rate of accumulation.
Symptoms can appear at any time: sometimes it’s weeks and months, sometimes hours.
As we have already noted, one of the visual symptoms is an enlarged abdomen. Let's add weight gain here.
The patient may develop a feeling of bursting pain, flatulence, belching, heartburn, and nausea.
An increase in the volume of the abdomen entails the appearance of severe shortness of breath, swelling of the extremities, difficulty moving and bending.
Another number of symptoms that a patient may encounter are hemorrhoids, hernias, intestinal prolapse, and the development of varicocele.
Common symptoms of the disease include:
- Feverish state;
- Toxic state;
- Losing weight and at the same time growing belly;
- The saphenous veins of the abdomen are dilated;
- Blueness on the limbs.
Types of disease
In the main classification, to differentiate pathology, the level of protein in the accumulated fluid is taken into account. According to this indicator, the disease is divided into:
- Exudative (25 g/l or more);
- Transudative (<25 g/l).
Such a division makes it possible to understand, albeit indirectly, what is the cause of the development of the disease.
Today, another indicator is used in medical practice - SAAG.
If this gradient is > 1.1, then most likely the cause of the disease is cirrhosis, heart failure, etc. All of them increase the pressure in the venous trunk.
If the gradient index is <1.1, then the cause of the disease can be considered pancreatitis or an oncological process.
Taking into account the clinical course of the disease, it is necessary to highlight the following varieties, which will be discussed below.
- Severity of the current:
- First degree. There are no symptoms, diagnosed by examination and ultrasound.
- Second degree. The abdomen is slightly enlarged.
- Third degree. The abdomen is significantly enlarged.
- An uncomplicated option. There are no signs of infection of the accumulated fluid mass and abnormalities in kidney function.
- Refractory ascites:
- Unaffected by diuretics;
- Not controlled by diuretics.
Forecast
Ascites in cancer significantly worsens the prognosis. From the moment of diagnosis, only half of the patients remain alive within 1–4 months. The average life expectancy is from 20 to 58 weeks. Timely treatment in a clinic that specializes in working with such patients helps improve survival. With ascites caused by liver cirrhosis, when there is no cancer, the prognosis is better. And a patient whose accumulation of fluid in the abdominal cavity was caused by chronic heart failure, with appropriate treatment, can live for many more years.
Pathology and cancer
Medical statistics and practice show that the most common diseases leading to the accumulation of liquid mass in the peritoneal cavity are oncological forms:
- Ovaries;
- Mammary glands;
- Uterus;
- Stomach;
- Colon.
A liquid mass accumulates with a tumor due to damage to the peritoneal lining. Atypical cells, having settled on it, cause disruption of lymphatic drainage, which, in turn, impairs fluid absorption. This is very common, for example, in gastrointestinal oncology.
If we take an organ such as the liver, the picture will be different. A tumor or metastasis localized in an organ causes compression of the venous system of the organ and disruption of normal venous outflow from the intestine. In this case, the pathology develops rapidly and is more severe. About fifteen percent of ascites in cancer processes is diagnosed in this form.
Where does bloating occur?
Bloating occurs in different parts of the digestive tract.
In the stomach
The stomach always contains a certain amount of air that enters it during meals. The natural mechanism for getting rid of excess air is belching; the remaining volume enters the small intestine.
The stomach contains mainly nitrogen and oxygen - gases contained in the atmosphere and have no odor. An unpleasant odor occurs when gases pass through the small and large intestines.
In the small intestine
In the small intestine, gas bubbles combine with liquid digested food and are absorbed through its mucous membrane.
In the duodenum (the initial part of the small intestine), the reaction of hydrochloric acid with alkali produces carbon dioxide. Under normal conditions, most of the carbon dioxide is absorbed into the blood, and the rest passes further into the large intestine. When carbon dioxide is produced in excess, it is retained in the small intestine, causing bloating.
In the large intestine
Feces accumulate in the large intestine, and gases are not absorbed into the blood. They can only come out through the rectum. Depending on the volume of gas accumulated in the colon, it is released at different frequencies.
Gases affect the functioning of the large intestine in different ways. Thus, an excessive amount of methane in the gas composition leads to constipation, because methane impedes the movement of feces through the rectum. An increased concentration of hydrogen negatively affects motility, but activates movement in the lower parts of the colon.
When there are problems with digestion and undigested food enters the large intestine, the compounds indole and skatole are formed. When they combine with hydrogen sulfide, they acquire a sharp, unpleasant odor.
Specifics of treatment for cancer
Conservative methods are effective in treating pathologies of only minor and moderate severity. The diuretics used here allow you to remove up to a liter of liquid mass per day.
However, the surgical option is preferable. It is used when:
- The disease cannot be treated by other means;
- A significant form of the disease, in which it is necessary to evacuate up to ten liters of liquid mass at a time;
- A form of the disease that requires combined manipulation, including evacuation of a volume of liquid mass of up to seven liters on the first day and evacuation of the remaining mass at a rate of no more than one liter per day for a week.
The operation is performed on an empty stomach and with an empty bladder. The patient is positioned in a sitting position (lying down is possible).
Before the puncture, local anesthesia is performed, then the puncture is performed under ultrasound control.
As a rule, no more than five liters of liquid mass are evacuated at a time. To maintain blood pressure, it is pumped slowly.
It is important for the patient to lie on the side free from the puncture for several hours. If during this time all the planned liquid mass is not evacuated and continues to accumulate, a special reservoir is applied.
When removing large amounts of fluid, it is important that the patient does not experience protein deficiency. To do this, the patient is injected with albumin.
In modern practice, special catheters are used to evacuate accumulated fluid, and some patients undergo the procedure of omentohepatophrenopexy. This is an important part of palliative treatment.
How to treat ascites?
There are several main methods for treating ascites in patients with cancer:
- conservative therapy (aldosterone antagonists, diuretics) - aimed at normalizing water-salt metabolism and reducing the formation of fluid in the abdominal cavity;
- laparocentesis - puncture of the abdominal wall under ultrasound control; used not only for removing fluid, but also for installing drainage, which will serve for long-term removal of fluid;
- palliative surgical operations - peritoneovenous shunt, omentohepatophrenopexy, deperitonization of the abdominal walls and others.
Traditional methods of treating ascites caused by cancer do not have proven effectiveness and safety, therefore they are not used at Euroonko.
If you come to our clinic with ascites due to cancer, we recommend getting a second opinion regarding the treatment of the underlying disease from our clinical oncologists and chemotherapists.