Pain in the lower abdomen in women is an unpleasant sensation that often signals a harmful effect on the genital organs, their damage, or the occurrence of a condition dangerous to health. They can occur even in the absence of traumatic factors. However, discomfort affects the psycho-emotional sphere of a person’s life and limits his mobility.
According to the World Health Organization, many diseases are accompanied by this symptom. Therefore, if women experience pain in the lower abdomen, they should make an appointment with a doctor. He will correctly determine the reason for their appearance. To do this, you will undergo an examination and a comprehensive examination, which may include laboratory, visual, endoscopic and other diagnostic methods. Based on the results obtained and medical history, the doctor decides on treatment tactics - conservative and/or surgical.
The nature of pain in the lower abdomen in women
When visiting a doctor, it is important to provide comprehensive information about your health condition. You need to pay attention to the circumstances under which you experienced discomfort, as well as the nature of the manifestations. So, for example, you may experience:
- acute pain in the lower abdomen in women. Sometimes it is called piercing;
- nagging discomfort;
- cutting pain;
- cramping pain. They are accompanied by spasms.
It is also important to consider when exactly you felt discomfort. According to the time of occurrence, there are:
- sharp pain in the lower abdomen in women. They appear suddenly and are characterized by high intensity;
- chronic pain. They may be felt for some time, and then subside and reappear after a certain period.
M-anticholinergics
M-anticholinergics are one of the oldest groups of drugs.
Atropine has been used in medicinal herbs since the 4th century BC. e. Thus, the ancient Greek naturalist Theophrastus described mandrake as a remedy for treating wounds, gout and insomnia, and also as a “love potion.” The ancient Greek military physician Dioscorides (1st century AD) described mandrake wine as an anesthetic to treat pain or insomnia, to be given before surgery or cauterization. M-anticholinergics most effectively affect the upper gastrointestinal tract. The use of non-selective M-anticholinergics (atropine, platyphylline, metacin) is limited by their prescription, as well as by the fact that they have a systemic effect and have a number of side effects, such as intestinal atony and obstruction.
One of the relatively oldest selective M-anticholinergics is hyoscine butyl bromide (first registered in Germany in 1951). It acts on the M1 and M3 subtypes of receptors, localized mainly in the walls of the upper gastrointestinal tract, gallbladder and biliary ducts. Hyoscine butyl bromide does not penetrate the blood-brain barrier and has a weak systemic effect, unlike atropine. However, it is contraindicated in people with glaucoma, benign prostatic hyperplasia, as well as organic stenosis of the gastrointestinal tract and tachyarrhythmias. Hyoscine butyl bromide accumulates in the smooth muscles of the gastrointestinal tract and is excreted unchanged by the kidneys. The drug is successfully used for sphincter of Oddi dysfunction, biliary dyskinesia and pyloric spasm.
The severity of the effect of hyoscine butylbromide also depends on the patient’s individual sensitivity to this drug. Unfortunately, the antispasmodic effect of hyoscine butyl bromide on the small intestine (except the duodenum) and large intestine can be realized when taking a dose 2–10 times higher than the therapeutic dose, so its use is useless for spasms in the lower abdomen. A large number of restrictions and risks when taking this drug require medical supervision, which is why the M-anticholinergics known to us are currently used less and less abroad. However, hyoscine butyl bromide is still available without a prescription.
Causes of lower abdominal pain in women
Discomfort can be caused by physiological conditions, as well as pathologies:
- reproductive organs. In this case, discomfort signals inflammation, neoplasms, etc. Typically, pain in the lower abdomen is not the only symptom in women. It can occur along with increased body temperature, irritation in the genital area and other manifestations;
- urinary system. Pain is caused by infections and viruses that provoke the occurrence of an inflammatory process;
- digestive organs. In this case, neoplasms and inflammation of unknown etiology occur. Gas may occur in the small and large intestines.
Let's take a closer look at the common causes of lower abdominal pain in women.
Inflammatory diseases of the reproductive system
This symptom may indicate the following pathologies:
- adnexitis. There is a feeling of heaviness in the lower abdomen;
- endometritis.
With these diseases, intense paroxysmal or constant pain occurs over the pubic bone, as well as discomfort in the lateral abdomen. Their exact localization is a signal of inflammation. However, with acute endometritis, you will not be able to determine exactly where it hurts. You may experience weakness, unusual discharge, and an increase in body temperature.
Chronic adnexitis is accompanied by nagging pain with short-term spasms. Its intensity increases after stress, during hypothermia. It is important to pay attention to the intensity of pain in a woman’s lower abdomen during sexual intercourse. Its rapid intensification is a defining (pathognomonic) sign.
Endometriosis
With this pathology, patients report nagging or aching pain in the pelvic organs. Their intensity increases before the start of the menstrual cycle. Discomfort reaches its peak in its first 2-3 days. You may also notice increased pain during sexual intercourse.
Neoplasms
Depending on the etiology, the following pathologies are distinguished, in which pain in the lower abdomen occurs in women:
- myoma. This disease is accompanied by the formation of a benign tumor. It grows from the muscle and connective tissue of the uterus. With subserous and interstitial forms of pathology, the patient feels dull pain. Submucosal fibroids are accompanied by severe spasms. The nature of the sensations changes on different days of the menstrual cycle;
- oncology. With malignant tumors there is constant discomfort. In this case, the pain “radiates” to the rectum, to the sacrum, to the lower back. With oncology of the uterine body, cramping sensations occur. They appear suddenly. After the attack of pain ends, you can replace the bloody or bloody discharge from the vagina.
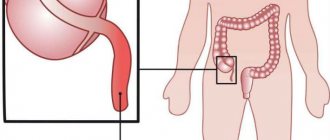
Appendicitis
When the appendage of the cecum becomes inflamed, discomfort occurs in the iliac region, as well as above the pubis. The exact location of pain in the lower abdomen in women depends on the location of the appendix in a particular patient.
You will feel intense discomfort with increasing tension in the right iliac fossa. In some cases, problems with bowel movements and vomiting may occur. Do not delay seeking emergency medical help: as acute appendicitis progresses, it can cause peritonitis.
Algomenorrhea
According to WHO data, up to 70% of women aged 15-45 years experience this condition. It is characterized by the onset of pain 12-24 hours before the start of the menstrual cycle. As a rule, women of reproductive age note aching or nagging discomfort. In most clinical cases it is characterized by moderate intensity.
The severity of algomenorrhea (dysmenorrhea) may vary. However, in 15% of cases, women present with severe pain, which leads to disability. They may also be accompanied by dizziness, weakness, and nausea. Spasms intensify with defecation, turning the body, coughing, sneezing. This condition also negatively affects the psycho-emotional background of a woman.
Conditions during pregnancy
Carrying a child is one of the natural states of women. During a normal pregnancy, she may experience discomfort in the lower abdomen for a short time. This is due to the growth of the uterus, the load on the ligaments that support it.
As the fetus gets larger, the uterus begins to put pressure on some other organs. Because of this, pregnant women may experience pain in the lower abdomen in the second or third trimester. This is also when Braxton Hicks contractions begin. They are false, but they cause contractions of the uterus, which can cause discomfort.
However, intense pain in the lower abdomen in women carrying a fetus is often a signal of the development of complications. For example, a sign of an ectopic pregnancy is considered to be aching discomfort on the left side of the groin area or on the right side. In this case, the patient notes a delay in menstruation, swelling of the mammary glands, and a change in appetite.
During a miscarriage, acute pain occurs in the sacrum and above the pubis, as well as bleeding. This can be triggered by stress, heavy lifting, or a blow to the stomach.
Another complication may be placental abruption. It can be recognized by acute paroxysmal intense or aching pain in the lower abdomen in women during pregnancy. It is accompanied by bleeding. The abdomen becomes hard on palpation.
Pain in the lower abdomen after intercourse
In most cases, after sexual intercourse, women may experience discomfort in the lower abdomen due to contraction of the uterus. If its intensity is low, then do not worry.
However, systematic intense pain in the lower abdomen in women after sex can occur with the development of the following pathologies:
- endometriosis;
- fibroma;
- cystitis.
Hernias
When organs protrude in the groin area, as well as spigelian or white lines, pain in the lower abdomen is observed in women. They clearly appear when this area is compressed with a belt, straining when going to the toilet, or wearing uncomfortable clothes. With significant protrusion of the hernia, the discomfort becomes constant.
Intestinal infections
Pain in the lower abdomen occurs in women and men with the following infectious pathologies:
- yersiniosis;
- Escherichiosis;
- shigellosis;
- campylobacteriosis.
The patient experiences severe cutting discomfort. It occurs against the background of a painful urge to defecate. Diarrhea develops with urges 10 times a day.
Pathologies of the urinary system
- Bladder polyps. When they occur, dull pain appears in the pubic area. Their intensity increases at the end of urination.
- Urethritis, pyelonephritis. With these pathologies of the excretory system, pain occurs in the lower back. When urinating, a woman may feel pain in the suprapubic area.
- Cystitis. Inflammation of the bladder is characterized by severe pain. It is provoked by E. coli or staphylococcus. Women experience aching pain in the lower abdomen and a frequent urge to urinate. Going to the toilet is accompanied by cramps and pain. As cystitis progresses, the urge to urinate becomes false. In the acute form of the disease, blood may appear in the urine.
Chronic pelvic pain syndrome
These manifestations are not associated with menstruation and last for 6 months or more. The patient may notice discomfort in the pelvic organs, sacrum, perineum, and suprapubic region.
You may feel the pain “radiating” to the buttocks and joints. It intensifies with hypothermia, physical exertion, sexual contact, and gynecological examination.
Rare causes of lower abdominal pain in women
The symptom occurs most rarely with the following pathologies:
- inferior vena cava syndrome, varicose veins;
- genital prolapse. In this case, nagging pain occurs;
- Crohn's disease, ulcerative colitis.
Classification
Abdominal pain varies in location, intensity, and nature. It can be spread throughout the abdomen or localized (in the epigastrium, in the navel, lower abdomen, in the hypochondrium and iliac region on the left or right). Sometimes the pain has a girdling character, simultaneously covering the abdomen and lower back.
In terms of intensity, abdominal pain can be mild, moderate or severe. Severe pain is extremely difficult for patients to bear: they force the patient to moan, toss about in bed, and take a forced position. Of great importance for the clinician conducting the initial diagnosis is the time and conditions under which abdominal pain appears: on an empty stomach, during or after a meal, at night.
The most diverse and telling sign is the nature of the pain in the abdomen. However, this is a subjective feeling that can be interpreted differently by different people. Most often, abdominal pain is characterized by the following epithets:
- acute
- stupid
- aching
- pulling
- cramping
- cutting
- piercing (“dagger”)
- burning
- compressive
- colicky
Diagnosis of lower abdominal pain in women
Various doctors can identify the cause that accompanies such an unpleasant symptom: gastroenterologists, gynecologists and other specialists. The patient is recommended to undergo a comprehensive examination. It includes:
- gynecological examination. It is carried out in a chair. The gynecologist pays attention to the size and condition of the uterus and determines the location of pain. When examined in the mirrors, the doctor clarifies the condition of the reproductive organs, vaginal mucosa, etc.;
- Ultrasound is a visual diagnostic method that helps assess the condition of the appendages and uterus, establish pregnancy, find various neoplasms, and inflammation. It allows you to exclude diseases of the distal parts of the intestine, as well as inflammation of the appendix of the cecum;
- laboratory methods. They include blood, urine, and mucous tests. They help clarify the cause of the infection, determine the balance of hormones, and find the inflammatory process;
- X-ray. Hysterosalpingography is often used to diagnose pain. It allows you to find fibroids, endometrial polyps, determine tubal obstruction, tumors of various etiologies, and developmental abnormalities of the structure of the reproductive system. Irrigoscopy and excretory urography are also used for diagnosis;
- endoscopic methods. Characterized by high accuracy. For example, hysteroscopy helps to detect tumors and inflammation. Colonoscopy helps determine UC and Crohn's disease. If necessary, a tissue sample will be taken during a biopsy for further histological examination.
Diagnostics
Abdominal pain is never the only symptom of the disease. It is usually accompanied by other clinical manifestations. Associated symptoms play an important differential diagnostic role. Frequent companions of abdominal pain are heartburn or belching, bloating, diarrhea or constipation, and lack of appetite. Dangerous signals are increased body temperature, vomiting (especially with blood), and fainting.
However, it is not possible to determine the causes of abdominal pain solely on the basis of the clinic; in all cases, additional examination is required:
- physical: palpation of the abdomen, auscultation of noises, percussion;
- laboratory: general blood and urine tests, monitoring of biochemical parameters (liver tests, pancreatic enzymes, acute phase proteins);
- instrumental: ultrasound of the abdominal cavity and genitourinary organs, radiography of the abdominal cavity, gastroscopy, etc.
- invasive: diagnostic laparoscopy, laparocentesis.
Principles of assistance before specifying a disease accompanied by pain in the lower abdomen
If minor discomfort is observed during pregnancy, it is recommended to rest well. Do not lift heavy objects, try to avoid exercise. It is also important to follow a diet: do not eat foods that cause gas formation. They often contribute to the occurrence of abdominal pain during this period. If discomfort increases, cramping or bleeding occurs, you should immediately consult a doctor.
If you have painful periods, you can start with non-drug methods. Take care of your own psychological state, try to lie in the fetal position, applying a warm heating pad to the place where discomfort occurs. To prevent more spasms in the area, avoid coffee, tea, spicy foods, and smoked foods. Give preference to herbal teas with mint.
Pain. Warns and protects.
Who among us does not know what pain is? Everyone has experienced pain at least once in their life. Defining pain is not so difficult; it does not require sifting through a mountain of medical literature or looking too deeply into medical reference books. When a person is in pain, he suffers, and the only thought that always comes to him and in all situations when pain appears is a desperate desire for it to go away as soon as possible. And she never appeared again. But, alas, there are no miracles in the world, and no matter how much we want it, she always comes back. Sometimes more often, sometimes less often. Every minute, millions of people around the world take painkillers. Humanity consumes tons of analgesics every day. Every year, more and more advanced drugs are being developed and created around the world that “relieve this pain as if by hand.” It seems quite reasonable to us that we give pain a proper rebuff at its first appearance. Have you ever thought, even for a moment, whether the appearance of pain is so accidental? Is it as evil as we think? Remember school, a biology textbook that said that “pain is a vital function of our body that warns us of danger.” There is no pain that is safe, that can be ignored. Nature has built into us certain irritants; when the pain threshold is exceeded, they give the body a signal of danger.
Conservative treatment of pathologies that cause pain in the lower abdomen in women
The doctor chooses the treatment tactics after an examination. The medications will be prescribed to you after the clinical picture has been clarified. At the same time, it is important to adhere to the specialist’s recommendations regarding the daily routine, nutrition, and water regime. Afterwards you may be recommended to take the following medications:
- antibiotics. Required for infections. The doctor selects a group of drugs based on their underlying cause;
- hormones. Used to correct fibroids, endometriosis, severe dysmenorrhea and other pathologies. Combined oral contraceptives are often prescribed. They are selected individually for each patient;
- painkillers. Analgesics and antispasmodics can be taken for inflammation, as well as dysmenorrhea.
Where to go?
The doctors of the 5th Clinical Hospital have extensive experience in performing laparoscopic operations and hernioplasty in Minsk.
In addition to accepting patients who are citizens of Belarus, the 5th City Hospital of Minsk also accepts foreign citizens (on a paid basis). Each of them can undergo comprehensive diagnostics and treatment at the surgical and therapeutic departments.
The hospital has its own clinical diagnostic laboratory, X-ray department, X-ray CT and MRI rooms. The physiotherapy department has all the conditions for conducting rehabilitation programs.
Surgical treatment of diseases that cause pain in the lower abdomen in women
Some conditions accompanied by this symptom require surgical treatment. Some of them are urgent, including ectopic pregnancy. In this case, removal of the fallopian tube or tubotomy is performed - an intervention that helps preserve reproductive health.
You can also undergo an oophorectomy, wedge resection of the ovary, or adnexectomy if indicated. Hernias and appendicitis also require surgical treatment.
Conclusion
Pain in the lower abdomen in women significantly reduces the quality of life. Don't try to endure the discomfort. Acute conditions can become chronic, which often leads to complications. Acute intense pain is a signal to immediately seek medical help. It may be a sign of a life-threatening condition.
Treatment
Help before diagnosis
For abdominal pain associated with menstruation, non-drug methods are sufficient. Herbal teas with chamomile and mint are effective. You can put a warm (not hot!) heating pad on your lower abdomen and lie with it in the “fetal position”, pulling your knees towards your body. To reduce menstrual cramps, it is advisable to give up strong tea and coffee, spicy and smoked foods. A woman’s psychological mood, the ability to calm down and relax are very important.
For minor pain that occurs in pregnant women, doctors recommend avoiding physical activity and heavy lifting and getting plenty of rest. It is necessary to exclude from the diet foods that increase gas formation, since flatulence is one of the main causes of abdominal pain during gestation. If pain intensifies, protective tension in the abdominal muscles appears, and bloody discharge from the vagina occurs, you should seek medical help as soon as possible.
Conservative therapy
Treatment of women experiencing pain in the lower abdomen should be etiopathogenetic, so drugs are prescribed only after identifying the root causes of the pain syndrome. Drug therapy is supplemented with a gentle regimen, if indicated - bed or half-bed, a fortified diet with an adequate amount of fluid. Treatment regimens may include the following groups of medications:
- Painkillers
. Taking antispasmodics and analgesics is effective for all types of inflammatory diseases of the genitourinary system and algomenorrhea, accompanied by severe pain. Non-steroidal anti-inflammatory drugs are also used for inflammation. - Antibacterial drugs
. Antibiotics are indicated for adnexitis, endometritis, cystitis, intestinal infections, etc. More often drugs from the group of cephalosporins, fluoroquinolones, and macrolides are used. For uncomplicated urinary tract infections, uroseptics are appropriate. - Hormones
. For the treatment of severe algomenorrhea, combined oral contraceptives or natural progestins are recommended. A similar treatment regimen is selected for women suffering from endometriosis. - Sedatives
. Medicines are effective for chronic pelvic pain, algomenorrhea, especially if they are combined with severe neuropsychic symptoms.
Surgery
A number of obstetric pathologies require urgent surgical intervention. In case of an ectopic pregnancy, an operation is performed to remove the fallopian tube along with the fertilized egg (tubectomy), and in case of an uncomplicated pregnancy, an organ-preserving operation - tubotomy - is possible. Complete premature placental abruption is an indication for cesarean section, regardless of gestational age.
Gynecological diseases (ovarian apoplexy and torsion of the tumor stalk) are treated surgically by oophorectomy, adnexectomy, wedge resection of the ovary. In severe forms of endometriosis, endometrioid lesions are excised. Surgical treatment is also required for abdominal pathologies: appendicitis (appendectomy), hernias (hernioplasty).