An important role of therapeutic nutrition in the complex therapy of kidney diseases is played by pronounced metabolic disorders and possible disturbances in the functioning of the digestive organs. Nutritional therapy is prescribed simultaneously with drug therapy. Diet therapy is based on the main pathogenetic mechanisms of the disease and provides for the need to spare the kidneys, level out metabolic disorders, and potentiate the effect of diuretics and other medications. The possibility of concomitant circulatory failure determines the need to spare the cardiovascular system.
The main differences in diet therapy relate to the amount of protein, salt and water, which is determined by the clinical form, period of the disease and the functional characteristics of the kidneys. What matters is the presence or absence of edema, high blood pressure, azotemia, albuminuria, hypoproteinemia and the degree of their severity.
So, with azotemia, it is necessary to limit protein, with edema and high blood pressure - salt. Noteworthy is the fact that there is no fluid retention in the body on a salt-free diet, and therefore the permissible volume of fluid consumed is determined by diuresis plus 500 ml (extrarenal losses).
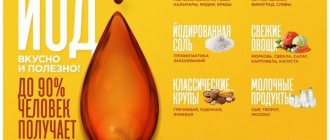
Since edema can be associated with proteinuria, hypoproteinemia in the absence of azotemia dictates the need to enrich the diet with protein. It is necessary to enrich the diet with potassium when prescribing a number of diuretics that promote its excretion in the urine and can lead to hypokalemia (dichlorothiazide, furosemide, etc.).
Therapeutic nutrition for kidney diseases involves the use of renal diets No. 7a, 76, 7b, 7 and special fasting diets (sugar, apple, potato, rice compote, watermelon, pumpkin), which help remove fluid and under-oxidized metabolic products from the body, reduce blood pressure and reduction of azotemia.
General rules
Glomerulonephritis is a bilateral diffuse inflammation of the kidneys with damage to the glomerular apparatus. The most common (70–80% of the total) mechanism of disease development is immune complex. There is no direct damage to the kidneys by the pathogen, and the disease is caused by an immunological reaction to various infectious agents and their antigens . Therefore, in the “classical” course of, for example, acute post-streptococcal glomerulonephritis, signs of the disease are observed 2 weeks after suffering from a sore throat - during this time, sensitization to streptococcal antigens occurs.
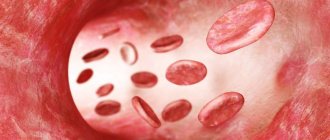
Nephritogenic strains of the pathogen produce proteins that have an affinity for the kidney glomeruli. These proteins are carried by the bloodstream to the kidneys and bind to areas of the glomeruli, forming immune complexes. This, in turn, leads to damage to the glomerular capillaries; exudative and proliferative processes develop in them with the development of local intravascular coagulation (microthrombosis of the glomerular capillaries is formed). Damage to the capillaries leads to an increase in their permeability, as a result of which red blood cells penetrate into the cavity of the glomerulus and kidney tubules - the patient develops red blood cells in the urine ( hematuria of varying degrees). With significant damage, the glomerular filtration rate decreases, which is manifested by oliguria (decreased amount of urine excreted).
edema occurs in 80-90% of patients and its primary location is the face. They are most pronounced in the morning and may subside during the day. Some patients develop a characteristic appearance: pale skin, facial swelling and swollen neck veins.
80% of patients experience increased blood pressure . This is due to an increase in circulating blood, an increase in cardiac output and peripheral resistance. A persistent increase in blood pressure is considered an unfavorable sign and may indicate congestive heart failure . Quite often the disease is asymptomatic, and the diagnosis is established already at the stage of chronic disease and chronic renal failure.
Patients are treated in a hospital. In the acute period, it is necessary to adhere to bed rest, create rest, which helps improve blood circulation in the kidneys. As the swelling disappears and the pressure normalizes, the regimen is expanded.
In addition to treatment, a special diet can affect all these changes. Nutrition for this disease is organized within the framework of treatment Table No. 7 (or its varieties) with carbohydrate fasting days during the acute stage. The diet protects the kidneys and is aimed at reducing swelling and pressure (food is prepared without salt), and helps improve the elimination of nitrogenous waste by limiting protein in the diet.
During the acute period of the disease, the consumption of salt and water is sharply limited. For oliguria , the daily amount of fluid is calculated using the formula: the amount of urine excreted over the previous day + 400 ml. Subsequently, the amount of fluid increases in accordance with the increase in diuresis.
In the first week of the disease, a salt-free diet is recommended. In most patients, even in the absence of treatment, this leads to the rapid disappearance of edema syndrome and normalization of pressure. If they are preserved, the salt-free diet is extended for a longer period.
After stable normalization of blood pressure, the addition of salt in the amount of 0.5-1.0 g/day is allowed. If the course is favorable, salt consumption is restored from 4-5 weeks - 50 mg per kg (for example, with a weight of 70 kg - 3.5 g of salt per day).
In acute glomerulonephritis, it is necessary to reduce the energy value of the diet. In case of mild to moderate severity, from the 1st day of illness, carbohydrate fasting days are prescribed for 1-2 days (watermelon, compote, grape, rice, vegetable, apple, potato) with a transition to Diet No. 7 with the exception of salt. The food is enriched with vitamins.
In severe cases and impaired excretory function of the kidneys (accumulation of nitrogenous waste), the patient is transferred to Table No. 7A or No. 7B . An increase in potassium in the diet (with the permission of a doctor, after determining the level of potassium in the blood) is achieved through the consumption of vegetables, fruits, cereals, and potatoes in their skins. To improve the taste, use tomato and lemon juice, weak apple cider vinegar, spicy vegetables and boiled onions. Vegetables can be consumed stewed, raw, boiled and lightly fried.
Thus, the diet for renal glomerulonephritis has the following basic principles:
- Limiting salt - food is not salted, and depending on the patient’s condition, a certain amount is added to prepared dishes. The approximate amount is given above, but for each patient it is calculated individually according to the doctor’s recommendations.
- Reducing the amount of protein by 0.9 g per kg of weight (or less in case of renal failure). Milk and egg whites, as well as vegetable proteins, are recommended as more easily digestible, although they have less nutritional value.
- Lean meat and fish. They are not allowed to be consumed without prior boiling. Prepared in this way, they can be baked, stewed or lightly fried. This intake reduces the protein load on the kidneys.
- Exclusion of products with essential oils: celery, fresh dill, radishes, radishes, basil, parsley, fresh garlic and onions.
- Limiting the amount of fluid.
- Five meals a day.
- Exclusion of spicy and salty snacks, strong broths and sauces, alcoholic beverages, pickled vegetables, strong tea and coffee, herbs and spices, cocoa and chocolate.
For chronic glomerulonephritis in remission and without impaired nitrogen excretion function, Diet No. 7 with a limit of salt to 8 g and protein to 60-65 g (half of which should be animal proteins). Protein restriction prevents the onset of kidney failure . Animal fats and sources of simple carbohydrates are limited, replacing them with vegetable oils and vegetables. This is due to disorders of fat and carbohydrate metabolism that are observed in chronic glomerulonephritis. With arterial hypertension, the amount of foods containing potassium increases (apricots, dried apricots, raisins, potatoes in their skins, bananas, grapes).
The amount of protein in the diet varies and depends on the severity of renal failure, so the diet has several varieties. Table No. 7A provides for the complete exclusion of salt and a significant restriction of protein - up to 20 g. This is a predominantly plant-based diet, which is prescribed for acute or chronic nephritis with severe renal failure.
When azotemia decreases, patients are prescribed Diet 7B , in which the amount of protein is increased to 40 g. In nephrotic syndrome (there is loss of protein in the urine), Table 7B with an increased protein content of up to 125 g, which replenishes its losses. As with previous varieties, the amount of liquid and salt is limited. For hemodialysis patients, Table No. 7G (contains 60 g of protein, 0.7 l of liquid and 2-3 g of salt).
In case of exacerbation of chronic glomerulonephritis, a carbohydrate fasting diet is prescribed for several days, followed by a transition to Table No. 7 . Thus, an individual diet for glomerulonephritis should be carried out by nutritionists or the attending physician.
During the period of reverse development of acute nephritis, urine output is restored, swelling disappears and blood pressure normalizes, and only after 2 months urine values return to normal. However, complete recovery (reversal of morphological changes in the kidneys) is observed after 1-2 years. Such a long recovery period dictates long periods of adherence to the diet. If individual symptoms persist for more than six months, this indicates a protracted course of the acute disease, and the duration of symptoms for more than 1 year indicates a transition to a chronic form.
Children of any age are at risk of kidney damage if they are exposed to one type or another. In children, there is a clear connection between infection and the occurrence of glomerulonephritis. An infectious factor is a trigger that triggers the development of immune complex or autoimmune diseases. The leading role in its development belongs to streptococcus , and acute post-streptococcal glomerulonephritis is the most studied and widespread form. Viral infection is also important. In the overwhelming majority, associations of glomerulonephritis are found, especially in its acute course, with the hepatitis B and herpes simplex virus type I , which is isolated from the blood, urine and saliva.
In children, isolated microhematuria sometimes persists for more than 1 year after acute glomerulonephritis, but without chronicity of the process.
The general principles of child nutrition are no different from those of adults. In severe forms, a salt-free fruit and sugar diet is prescribed in the first days. A child should eat 300-800 g of fruit and sugar at the rate of 8-10 g per 1 kg of weight. In the future, a dairy-vegetable diet is recommended. Since no convincing evidence of the effect of a low-protein diet on the course of the acute form of the disease has been obtained, it is customary to limit protein only at the rate of 1.0 g per kg of weight. Consumption of animal proteins is limited during the first 2-3 weeks.
The diet is replenished mainly from vegetable protein. The energy value must correspond to the needs of the sick child. In non-severe forms, a dairy-vegetable diet is immediately prescribed without prior fasting nutrition. Food is given in boiled or stewed form - baked potatoes, mashed potatoes, milk porridge, fresh fruits, fresh fruit purees, fresh vegetables in the form of salads, salt-free bread, milk, kefir, juices, savory cookies, cheesecakes, pancakes, tea with sugar , tea with milk, baked apples, juices, cereals, pasta, vegetable potato soups, milk soups, vegetable casseroles, cabbage rolls, compotes, mousses, jelly, rosehip infusion. If a child is taking diuretics, the diet must be enriched with foods rich in potassium (dried apricots, baked potatoes in their skins, prunes, raisins).
For children aged 7-13 years, the daily food set consists of one egg, 400 ml of milk, 20 g of sour cream, 300 g of salt-free bread, 300-500 g of potatoes, 60-90 g of cereal, 80 g of sugar, 60 g of butter, 10 g of vegetable oil, 250 g of vegetables and fresh fruits, 200 ml of juice, 10 g of dried fruits.
Spicy foods, smoked foods, extractive substances (broths, stews and fish), allergens (strawberries, citrus fruits, chocolate, coffee, cocoa chocolates), salted and pickled foods are contraindicated.
The prognosis for acute glomerulonephritis in children is favorable and 90% recover. In adults, the risk of chronicity of an acute disease with an outcome in chronic renal failure is 10 times more likely than in children.
Diagnosis of the disease
The most difficult thing to diagnose is an infant. During diagnosis, only an acute process can be identified, which in the vast majority of cases subsequently becomes chronic. In addition, the manifestations of the disease are similar to pyelonephritis. Source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305788/ Mamiko Hosoya, Yukihiko Kawasaki, Ryo Maeda, Masatoki Sato, Kazuhide Suyama, Koichi Hashimoto, and Mitsuaki Hosoya Predictive factors for poor outcome in pediatric C3 glomerulonephritis // Fukushima J Med Sci. 2018; 64(3): 142–150
Laboratory research:
- Analysis of urine;
- general blood analysis.
A number of examinations are also carried out:
- ECG;
- Ultrasound;
- Doppler ultrasound of renal vessels;
- fundus examination;
- if a chronic form is suspected, a kidney biopsy is performed.
Authorized Products
Nutrition for chronic glomerulonephritis includes:
- Bakery products and sweet pastries without salt.
- Lean meat (chicken, beef, lamb, turkey). It is necessary to pre-boil the meat before final cooking. Boiled minced meat is used for stuffing vegetables, preparing cabbage rolls, pancakes and casseroles.
- Low-fat fish, which is also boiled and then baked or stewed with vegetables.
- Sauces (any vegetable, sour cream, tomato, milk or onion) as an addition to meat, cereal and fish dishes. Dried dill, cumin or parsley are added to sauces.
- Soups made with water or vegetable broth. You can prepare soups with vegetables, pasta, cereals, borscht, cabbage soup and beetroot soup. First courses should not be very sour and spicy. Season the soups with sour cream or butter, add dried dill and parsley. Onions are introduced and used only after preliminary boiling.
- Cereals and pasta. You can diversify your dishes from them by making puddings, casseroles, cutlets, pilaf with vegetables or fruits. Dried apricots, raisins, and prunes are added to sweet cereal casseroles.
- Milk, curdled milk, yogurt - up to 400 ml per day. Cream and sour cream are added only to dishes. Cottage cheese and dishes made from it with the addition of carrots, pumpkin and various fruits.
- Up to 2 eggs per day (if the amount of proteins is reduced due to other products). They are consumed in the form of an omelet or soft-boiled.
- Vegetables (with the exception of prohibited and pickled ones) are boiled, stewed, baked. They are used to make cutlets and casseroles, adding permitted dried herbs (cumin, parsley and dill).
- Ripe fruits and berries: fresh, baked, jam, jelly, compotes, purees, jelly.
- Juices, rosehip infusion, weak coffee, tea with lemon and sugar. As desserts you can eat caramel, marshmallows, fruit ice cream, honey, marshmallows.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| apricots | 0,9 | 0,1 | 10,8 | 41 |
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
| figs | 0,7 | 0,2 | 13,7 | 49 |
| nectarine | 0,9 | 0,2 | 11,8 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| strawberry | 0,8 | 0,4 | 7,5 | 41 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| dates | 2,5 | 0,5 | 69,2 | 274 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| milk candies | 2,7 | 4,3 | 82,3 | 364 |
| fondant candies | 2,2 | 4,6 | 83,6 | 369 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
Raw materials and seasonings | ||||
| cinnamon | 3,9 | 3,2 | 79,8 | 261 |
| honey | 0,8 | 0,0 | 81,5 | 329 |
| dried parsley | 22,4 | 4,4 | 21,2 | 276 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
| sour cream sauce | 1,9 | 5,7 | 5,2 | 78 |
| tomato sauce | 1,7 | 7,8 | 4,5 | 80 |
| caraway | 19,8 | 14,6 | 11,9 | 333 |
| dried dill | 2,5 | 0,5 | 6,3 | 40 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
| acidophilus | 2,8 | 3,2 | 3,8 | 57 |
| yogurt | 4,3 | 2,0 | 6,2 | 60 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| boiled beef tongue | 23,9 | 15,0 | 0,0 | 231 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Oils and fats | ||||
| corn oil | 0,0 | 99,9 | 0,0 | 899 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
| ghee | 0,2 | 99,0 | 0,0 | 892 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| coffee with milk and sugar | 0,7 | 1,0 | 11,2 | 58 |
| black tea | 20,0 | 5,1 | 6,9 | 152 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| * data is per 100 g of product | ||||
Necessity of diet
With the development of glomerulonephritis, the excretory capacity of the kidneys decreases, which inevitably leads to the accumulation of harmful substances and the development of many chronic pathologies. Prescribing a special treatment table helps to avoid this, which helps restore metabolic processes in the body and speeds up recovery.
Dietary nutrition is prescribed for the following purposes:
- reducing the load on the kidneys;
- correction of urinary retention;
- acceleration of clearance (purification) of blood plasma from toxic substances;
- decreased blood pressure;
- elimination of edema.
The therapeutic diet for glomerulonephritis should provide the patient with all the necessary vitamins and minerals without overloading the body, as well as combat excess weight and accelerate the regeneration of kidney tissue.
Fully or partially limited products
- Salt, salty food. You cannot eat regular bread, all flour and confectionery products with salt, and any cheese.
- Products containing artificial ingredients.
- Out-of-season vegetables containing nitrates.
- Rich broths and decoctions of legumes.
- Fatty types of meat and poultry (pork, duck, goose, lamb), sausage, smoked meats, canned food, stewed or baked meat without prior boiling.
- Animal fats, lard, cream, sour cream.
- Smoked and salted fish, fish caviar, canned fish.
- Milk soups and porridges with milk are limited
- Legumes, fresh onions, garlic, spinach, sorrel, mushrooms, radishes and radishes.
- Any pickled, salted and pickled vegetables.
- Hot seasonings, spicy dishes, pepper, horseradish, mayonnaise, mustard.
- Strong coffee and tea, cocoa, sodium bicarbonate mineral waters.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| sauerkraut | 1,8 | 0,1 | 4,4 | 19 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| canned cucumbers | 2,8 | 0,0 | 1,3 | 16 |
| pickles | 0,8 | 0,1 | 1,7 | 11 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| celery | 0,9 | 0,1 | 2,1 | 12 |
| canned tomatoes | 1,1 | 0,1 | 3,5 | 20 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| garlic | 6,5 | 0,5 | 29,9 | 143 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| marinated mushrooms | 2,2 | 0,4 | 0,0 | 20 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ginger | 1,8 | 0,8 | 15,8 | 80 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Alcoholic drinks | ||||
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
| * data is per 100 g of product | ||||
Several dish recipes
There is no need to think that cooking for patients with glomerulonephritis is a difficult task. On the contrary, a salt-free menu allows you to show a lot of imagination.
For example, tender and delicious carrot pudding, useful for any form of glomerulonephritis, is prepared in a matter of minutes. It will require:
- carrots - 1000 g;
- cow butter - 50g;
- sugar - 30g;
- milk - 1 tbsp. l.;
- semolina - 70 g;
- egg - 2 pcs.
The carrots are grated or passed through a meat grinder, butter and milk are added, then simmered over low heat until softened. Add semolina to the slightly cooled mixture and cook for another 5 minutes. Then add eggs, add sugar and mix thoroughly.
The finished carrot mass is placed in a baking dish and placed in the oven. Served with sour cream. The calorie content of one serving (200 g) of a dietary dish is 450 kcal.
Kohlrabi stewed in sour cream is quick and easy to prepare, especially useful for acute glomerulonephritis. Cabbage contains a lot of potassium, restores the water-salt balance in the body, goes well with cereals, fish and meat, is tasty and low in calories.
Product set:
- kohlrabi - 500 g;
- sour cream 15% - 5 tbsp. l.;
- cow butter - 3 tbsp. l.;
- egg - 1 pc.
Cabbage is cut into cubes or thin slices, stewed a little in a frying pan with the addition of oil, then sour cream is added and brought to readiness. The hot dish is seasoned with egg. Served with greens. A serving (200 g) contains only 260 kcal.
Dietary nutrition for glomerulonephritis is not too strict, but requires strict adherence. Any deviations may lead to exacerbation and increase the risk of complications.
Author: Elena Medvedeva, doctor, especially for Nefrologiya.pro
Menu (Power Mode)
The food menu is almost no different from the usual, only salt, spices and spicy dishes are excluded. The diet contains various cereals, all vegetables, meat, fish and cottage cheese. Adding dried herbs, lemon juice and a little natural vinegar can enhance the flavor of unsalted foods. Home-baked and fried flour products are also prepared without salt - bread, sweet muffins, pancakes, pancakes.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a medical specialist, primary, therapeutic and diagnostic, outpatient (other specialties) | 1750 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Prescription of treatment regimen (for a period of 1 month) | 2700 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Kidney ultrasound | 1700 rub. |
| Ultrasound scanning of kidney vessels | 1800 rub. |
Reviews and results
This diet is varied, taking into account the different methods of preparing dishes from cereals, vegetables and meat. Due to the restriction of salt, dishes turn out tasteless, and some patients find it difficult to get used to this. However, these restrictions are dictated by their condition and strict adherence is simply necessary. By following all nutritional recommendations, patients note positive results - after 5-6 days, swelling decreases and blood pressure decreases.
- “... I’ve been sick for 10 years. At first it was difficult to eat unsalted food, but for the sake of health I endured it. The swelling went down on the seventh day, and I began to urinate better. The hospital said that protein should not be abused, as this would be an additional burden on them. Therefore, my diet includes 150 g of meat or fish once a day, a glass of kefir or 100 g of cottage cheese. Mainly porridge, vegetables in various forms and pasta. I make my own salt-free bread, buns with raisins and without salt, yeast pies with cabbage or pumpkin in the oven. I maintain my blood pressure with a salt-free diet and after it it’s even easier to breathe and walk”;
- “... My child has chronic glomerulonephritis, nephrotic form. She has been ill for 10 years, and during this time there have been 3 exacerbations. The last time I was treated in a hospital with prednisolone, I took it for 5 months, now I have been in remission for 7 years. All these years, a strict diet, which is quite doable, except for the restriction of salt. He eats all cereals, soups, meat and fish, but in limited quantities. I bake him unsalted pancakes with vegetable fillings, fruits and jam. The amount of salt was allowed to be increased to 3 g, and this is already normal. The whole family was forced to switch to this diet and add a little extra salt to themselves. We constantly see a doctor”;
- “... The kidneys were never disturbed, but at one point dark urine appeared. We were hospitalized, examined and diagnosed with chronic glomerulonephritis. This was 20 years ago. The hospital had a salt-free table. I did not break it and refused ready-made foods with salt. For a whole year I didn’t eat sausage, smoked meat or pickles. Then I began to increase the salt a little, but in general the food was dietary (boiled meat and fish in moderation, fermented milk products, a lot of vegetables, porridge). Over time, the disease still progresses, no matter how hard I try to limit myself. At first I only had hematuria, but now the pressure is 200 and there is protein in the urine, red blood cells all over the field of vision. All this time I’ve been seeing a nephrologist, since this disease needs to be monitored and the tests constantly monitored.”
Causes of pathology
- bacteria;
- viral diseases;
- fungal infection;
- parasites;
- allergens;
- scarlet fever, tonsillitis, pneumonia, pharyngitis and other streptococcal infections;
- connective tissue diseases;
- heredity;
- overheating or hypothermia;
- stress;
- excessive physical stress;
- cystitis and other infectious pathologies of the urinary system;
- change of living climate;
- childhood rheumatism;
- systemic lupus erythematosus;
- hemorrhagic vasculitis;
- toxins;
- poison of snakes, bees;
- and etc.
Glomerulonephritis is not a death sentence
Advanced glomerulonephritis leads to severe complications. To combat illness, proper nutrition alone is not enough. It is necessary to take medications prescribed by the nephrologist. But you shouldn’t rely solely on medications.
Only a comprehensive fight against the disease, including avoiding prohibited foods, following a daily routine, following doctor’s recommendations and taking medications in a timely manner, will help overcome the disease and give the patient the opportunity to lead a full life.
Diagnostic methods
The most informative methods for diagnosing chronic glomerulonephritis today are:
- general laboratory analysis of urine, which reveals deviations in its density, the presence of protein, casts, red blood cells and leukocytes;
- biochemical laboratory blood test, which shows the level of protein, albumin, creatinine, cholesterol, urea, as well as all fat fractions;
- a biopsy of renal tissue, revealing structural and morphological changes in the glomeruli.
In addition, in accordance with the existing symptoms, the attending physician may prescribe other types of laboratory tests and instrumental studies in order to get the most complete picture of the patient’s condition. For example, an ultrasound of the kidneys is almost always prescribed to determine deviations in their size, tissue density and determine the filtration rate.
Recommendations for the duration of compliance
Additionally, experts give the following recommendations:
- The ingredients must be cooked. You can boil or steam food.
- Include foods high in vitamin C in your diet - this will increase the body's defenses and help it fight the disease.
- Monitor the protein content in the urine, blood composition, and the amount of urine excreted.
- If a child has glomerulonephritis, he is also prescribed a special diet, which involves the exclusion of salty, smoked, canned foods, food that contains dyes, stabilizers, soda, and sweets. You can diversify your child’s menu with vegetables, fruits, berries, jelly, and fruit drinks.