Paget's cancer, or Paget's disease, is a rare type of malignant breast tumor that affects the nipple and areola. The disease is named after the English physician James Paget, who lived and worked in the 19th century. In 1874, he was the first to note the connection between changes in the nipple and malignant tumors of the mammary gland. At the moment, Paget's disease is quite well studied, and there are effective methods for its treatment.
- Causes of Paget's cancer
- Paget's classification of cancer
- Stages of the disease
- Symptoms
- Diagnostic methods
- Modern methods and principles of treating Paget's cancer
- Forecast
- Are there effective methods of prevention?
Some numbers and facts:
- According to American experts, Paget's cancer accounts for about 1–5% of all types of breast cancer.
- Like all other types of malignant breast tumors, Paget's cancer in most cases occurs in women. The disease is rarely diagnosed in men.
- Most often, the disease is found in people over 50 years of age. There are cases where the pathology was diagnosed in adolescents and people over 80 years of age.
- The average age of female patients is 62 years, male patients - 69 years.
- 97% of patients with Paget's cancer also have "carcinoma in situ" or an invasive malignancy in the breast.
Causes of Paget's cancer
The causes of the disease are currently not fully known. There are two theories:
- Most experts are inclined to believe that Paget's cancer initially occurs inside the breast, and from there the cancer cells penetrate into the nipple and areola. This explains why 97% of patients have another tumor.
- According to the second theory, Paget's cancer develops independently as a result of malignancy of cells located in the nipple or areola. This is confirmed by the 3% of patients who do not have a second tumor in the chest.
The above-described changes in cells occur due to certain mutations. Each cancer cell carries a set of mutations that help it multiply and survive uncontrollably. Why such “cancerous” genetic changes occur in each specific case is impossible to say for sure. Doctors and scientists know some risk factors that increase the likelihood of developing Paget's cancer:
- Age. Over the years, mutations accumulate in the human body, and one day they can lead to the emergence of a malignant neoplasm in the mammary gland or other organ.
- Family history. If you have close family members who have been diagnosed with breast cancer, your risk is also increased.
- Hereditary mutations. For example, it is known that the likelihood of developing malignant breast tumors increases with mutations in the BRCA1 and BRCA2 genes. If parents have these genetic defects, they can pass them on to their children.
- Increased density of breast tissue. This can be detected during a mammogram, an x-ray examination.
- Burdened personal history. If a woman has previously been diagnosed with breast cancer, she has an increased risk of it recurring.
- Excess weight. This factor is especially dangerous if a woman begins to gain extra pounds after menopause.
- Alcohol. Excessive and frequent consumption of alcohol increases the likelihood of developing cancer.
- Hormone replacement therapy. Women who take estrogen medications are more likely to develop Paget's cancer.
If you find factors from the list, this does not mean anything. None of them are guaranteed to lead to cancer. Each only increases the probability to some extent. At the same time, the absence of all these factors does not guarantee protection against cancer.
Book a consultation 24 hours a day
+7+7+78
Pathophysiology.
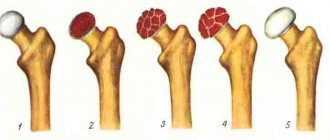
A characteristic feature of the disease is increased bone resorption, accompanied by acceleration of bone formation, which is usually sufficient to compensate for resorption. In the early stages, resorption processes predominate (for example, in a variant of the disease called limited osteoporosis), and the bone becomes excessively vascularized. This is called the osteoporotic, osteolytic or destructive phase of the disease, in which the calcium balance may be negative. As a rule, excessive resorption is immediately followed by the formation of new, but pathological bone tissue. In the so-called mixed phase of the disease, the rate of bone formation is so consistent with the rate of resorption that the increase in bone turnover does not affect the overall calcium balance.
As disease activity decreases, the rate of resorption progressively decreases and eventually strong, dense, less vascularized bone appears (the so-called osteoplastic or sclerotic phase) and a positive calcium balance is established. With active Paget's disease, the rate of bone turnover increases sharply and sometimes exceeds the norm by 20 times. Quantitative histomorphometry of biopsies of the affected bone confirms the high rate of its reconstruction, revealing a marked increase in resorption surfaces with deep serrated lacunae containing giant osteoclasts with many nuclei. The bone formation surfaces are also enlarged, and the edges of the lesion are lined with a large number of osteoblasts. The rate of calcification is also increased. Normal hematopoietic bone marrow is replaced by loose stroma, which may contain many vessels. The degree of increase in bone turnover depends on the volume of the lesion and the activity of the process and correlates with an increase in the plasma level of bone alkaline phosphatase, which is higher in Paget's disease than in any other disease except congenital hyperphosphatasia. Although the acceleration of bone resorption causes an increased release of calcium and phosphate ions from it, their use in new bone formation and, probably, feedback regulation of parathyroid hormone secretion usually keeps the concentration of calcium ions in the plasma at a normal level. Plasma phosphate concentrations are normal or slightly elevated. When the balance between bone formation and resorption shifts sharply in favor of the latter, as occurs with prolonged immobilization or fractures, urinary calcium excretion may increase and hypercalcemia rarely occurs. On the other hand, if bone formation exceeds resorption (which is relatively rare), the level of parathyroid hormone in the blood may increase. Resorption involves both the organic and mineral phases of bone. If the inorganic ions of the mineral phase are reutilized during the process of bone formation, then amino acids such as hydroxyproline and hydroxylysine, released during resorption of the collagen matrix of the bone, are utilized during the process of collagen synthesis. Urinary excretion of small hydroxyproline-containing peptides increases, reflecting increased bone resorption. Urinary excretion of peptides with a molecular weight of 1500-2000, containing hydroxyproline and other amino acids in a ratio characteristic of collagen, also increases and correlates with the acceleration of bone formation. Other markers of increased matrix synthesis include increases in osteocalcin (bone GLA protein) and long procollagen fragments in plasma.
Stages of the disease
Paget's cancer, in which there are additional tumor nodes in the breast, is classified into stages according to the generally accepted TNM system. Depending on the indicators T (size and spread of the primary tumor), N (spread to regional lymph nodes) and M (presence of separated metastases), 5 stages are distinguished:
- Stage 0 - the tumor is contained within the tissue from which it developed and has not spread to adjacent tissue.
- Stage I - tumor no more than 2 cm in greatest dimension. Cancer cells do not spread to the lymph nodes, there are no distant metastases.
- Stage II - tumor is 2 to 5 cm, which can spread to the lymph nodes. In this case, mobile lymph nodes are palpated on the affected side.
- Stage III . At stage IIIA, the size of the tumor can exceed 5 cm. It spreads to the lymph nodes, which become fused with each other and surrounding tissues. At stage IIIB, the primary tumor grows into adjacent tissues: skin, chest wall.
- Stage IV - there are distant metastases. It does not matter what size the primary tumor is.
Complications
Neuritis of the trigeminal nerve (see), facial nerve (see), deafness (see), optic nerve atrophy (see), hypertensive syndrome (see), CSF disorders are caused by thickening of the bones of the base and vault of the skull, flattening of the cranial fossae and narrowing of the openings of the skull. If the spine is damaged, spinal compression syndrome may develop.
Involvement of the hip joints in the process leads to severe coxarthrosis (see Arthrosis) and sometimes to protrusion of the head into the pelvis. Patol, fractures are not uncommon (see). Against the background of P. b. Both benign tumors can develop - osteoblastoclastoma (see), and malignant ones - osteogenic sarcoma (see) and other types of sarcomas (see), multiple myeloma (see). Malignization is the most dangerous complication of P. b. Sarcomas occur in 3-15% of observations of P. b. By structure, these are osteogenic, spindle cell, polymorphic cell sarcomas, chondrosarcoma, fibrosarcomas, reticular sarcomas. The course of sarcomas complicating P. b. is particularly malignant.
Symptoms
In 40–50% of patients with Paget's cancer, a lump in the breast can be felt. In 60–90% of cases, such a symptom indicates invasive cancer, that is, growing into surrounding tissues.
Usually the first symptoms of the disease are associated with changes in the nipple and areola. They can easily be mistaken for manifestations of another pathology - eczema or psoriasis:
- redness;
- itching, tingling, burning, soreness;
- deformation, flattening of the nipple;
- discharge - yellow or bloody;
- ulcerations, weeping, crusts;
- the nipple is easily injured, begins to bleed, and then crusts form.
It is worth remembering about other manifestations of malignant breast tumors: induration, asymmetry, “lemon peel”-type skin changes, enlarged axillary lymph nodes.
These signs do not always indicate cancer. But, if they appear, it is important to immediately visit a doctor and get checked.
A very rare type of disease is Paget's pigmented cancer. In this case, it is necessary to carry out a differential diagnosis with melanoma.
X-ray changes.
X-ray data reflect the nature of the main pathological process and the phase of the disease prevailing at the time of the study. The most commonly affected bones are the pelvis, followed by the femurs, skull, tibia, lumbosacral and thoracic spine, collarbones and ribs (in that order). Small bones are affected less frequently. The lytic phase of the disease is not always detected unless the skull bones are affected, as in limited osteoporosis, with the appearance of sharply defined radiolucent areas in the frontal, parietal and occipital bones. In long bones, areas of lysis are usually detected first at one end, from where they spread to the other in the form of a growing V-shaped edge. Damage may be accompanied by cortical proliferation and other signs of malignant growth. Typically, the area of lysis is followed by a zone of increased density, reflecting the process of new bone formation in the mixed phase of the disease. In general, the bone appears enlarged and denser with an unevenly expanded, rough and striated cortex; sometimes these changes are focal. Transverse radiolucent lines (cortical fractures) are often observed on the convex side of curved long bones, especially the femur and tibia. Complete fractures may also occur, some of which begin in areas of cortical fractures. Reconstruction of the affected bone is usually carried out in the direction of pulling muscle force or gravity, which determines the characteristic lateral bends of the femurs or the anterior bend of the tibia, as well as the deposition of the bulk of dense bone on the convex side of the bends. At the mixed stage of skull damage, there is an increase and thickening of the outer bone plates with uneven areas of increased density, often in the form of spots. Basilar invagination involving the base of the skull is common. Changes in the pelvic bones also reflect a combination of processes of bone resorption and new formation; the latter is often accompanied by a characteristic thickening of the pelvic arch. In the sclerotic phase of the disease, bone density may be uniformly increased; delineation is often absent. It is usually observed in the facial bones, but sometimes in the vertebrae, to which the homogeneity and density give an "ivory" appearance similar to that of typical Hodgkin's disease, although in the latter case the affected vertebrae are not enlarged.
Diagnostic methods
Diagnosis of the disease is carried out by an oncomammologist. During the initial appointment, he examines the mammary glands, nipple, areola, and palpates (feeling) to detect lumps.
Depending on the clinical manifestations, three forms of the disease are distinguished:
- There is damage to the nipple and areola, but there are no tumor nodes in the mammary gland.
- Nodal form.
- There is a tumor node, but there is no damage to the nipple and areola.
The main method for diagnosing Paget's cancer is biopsy. The essence of the study is that a sample of pathologically altered tissue is obtained and sent to the laboratory for examination under a microscope. This helps to reliably detect tumor cells and establish an accurate diagnosis.
Biopsy material can be obtained in different ways:
- Using scraping.
- Removing a thin layer of skin using a blade is a shave biopsy.
- Needle biopsy - using a special instrument in the form of a tube with sharp edges, it allows you to obtain a column of tissue.
- During a wedge biopsy, a wedge-shaped piece of tissue is removed.
- In some cases, the entire nipple is removed.
If the results of the biopsy reveal Paget's disease, the doctor prescribes additional tests: mammography, MRI, ultrasound. They help identify additional nodes in the chest.
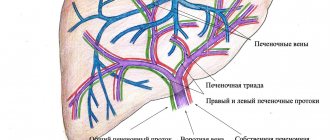
Epidemiology
The disease is most common in Western Europe, Australia and the USA, where it affects 1% to 4% of older people. Less common in Scandinavia, extremely rare in Asia and Africa. Epidemiology in our country has been poorly studied, but at least in its European part, Paget's disease is not uncommon. The disease affects not only mature and elderly people, but also young people (under 40 years old in approximately 10% of cases). Men get sick somewhat more often. Dominant, recessive types of inheritance and familial forms are detected with a frequency of 1.1% to 30% and are characterized by a more severe clinical course.
Modern methods and principles of treating Paget's cancer
For many years, surgeons used aggressive tactics for Paget's cancer: during surgery they removed the entire mammary gland (mastectomy) and axillary lymph nodes on the side of the tumor. This approach was argued by the fact that patients often have additional tumor nodes in the breast, and even if there is only one tumor, then after removal of the nipple and areola, part of it may still remain in the depths, which is fraught with relapse. Lymph nodes were removed just in case, since they may also contain cancer cells.
Currently, approaches have changed. Studies have shown that if there is only one tumor in the breast in the nipple area, and there are no other nodes according to mammography, only the nipple with the areola can be removed, subsequently prescribing a course of radiation therapy. After such organ-conserving surgery, there is no increased risk of relapse.
The attitude towards lymph nodes has also changed. Currently, there is a procedure that helps check whether there are any cancer cells left in them - sentinel biopsy . During the operation, the surgeon injects a special radiopharmaceutical into the tumor, which penetrates the lymphatic vessels, reaches nearby (“sentinel”) lymph nodes and causes them to “glow.” This “glow” is detected using a special apparatus - a gamma camera . This way, the doctor can find the lymph nodes that first receive lymph from the tumor, remove them and check for lesions. If the sentinel lymph nodes are “clean,” it means that the cancer cells did not have time to reach them, and there is no point in removing the remaining lymph nodes.
Sentinel biopsy helps to avoid unnecessary removal of lymph nodes and thereby prevent the development of complications associated with impaired lymph outflow - lymphedema .
After surgery, chemotherapy, hormonal, and targeted drugs may be prescribed. Typically, adjuvant chemotherapy is carried out in cases where a large tumor has been removed, foci have been found in the lymph nodes, and if the cancer cells were poorly differentiated and prone to aggressive growth. Hormonal therapy is indicated if there are hormone receptors on the surface of tumor cells.
Deep vein thrombosis
– a more severe illness, usually requiring the patient to stay in a hospital.
There are deep vein thrombosis of the leg, popliteal vein, femoral vein, iliofemoral (ileofemoral) thrombosis. Often there is damage to thrombosis of several sections (for example, the popliteal and femoral veins, deep veins of the leg and popliteal vein, etc.).
Deep vein thrombosis manifests itself primarily as swelling and moderate pain. Moreover, the higher the level of thrombosis, the more pronounced the edema. Thus, with thrombosis of the deep veins of the leg, there may be moderate swelling of the leg, sometimes the swelling is so insignificant that it is detected only when measuring the circumference of the leg (compared to the healthy leg). With thrombosis of the femoral or iliac (continuation of the femoral) veins, the entire leg, up to the groin, and in severe cases, the lower part of the abdominal wall swells.
In the photo - the left lower limb is cyanotic, thickened to the groin - deep vein thrombosis at the level of the iliofemoral segment (ileofemoral thrombosis).
Thrombosis, as a rule, is unilateral, so only one leg swells. Bilateral edema is observed with thrombosis of the inferior vena cava, deep vein thrombosis in both legs (which is quite rare).
Another symptom of thrombosis is pain. It is usually moderately expressed, pulling, sometimes bursting, is relatively constant in nature, and can intensify in a standing position. In case of deep vein thrombosis of the leg, the Homans, Lowenberg, Luvellubri, Meyer, Payra symptoms are positive.
With deep vein thrombosis, there may also be a slight increase in temperature, increased venous pattern, etc.
Forecast
The prognosis for Paget's cancer depends on a number of conditions. The presence of additional nodes in the chest and the stage of the disease are of great importance. In the United States, statistics were studied and it turned out that the 5-year survival rate (the percentage of patients surviving 5 years from the time the tumor was diagnosed) among women who received treatment for Paget's cancer from 1988 to 2001 was 82.6%. However, the average five-year survival rate for other types of breast cancer is 87.1%.
If there are additional nodes in the breast, the five-year survival rate decreases as the stage increases:
- Stage I - 95.8%;
- Stage II - 77.7%;
- Stage III - 46.3%;
- Stage IV - 14.3%.
Thus, early diagnosis helps improve the prognosis and significantly increases the chances of successful treatment. As soon as any suspicious changes in the mammary glands appear, you should immediately visit a mammologist and undergo an examination. And in order to promptly detect these changes, every woman needs to regularly conduct breast self-examination once a month. Once a year you need to be examined by a mammologist, after 40 years - a mammogram.
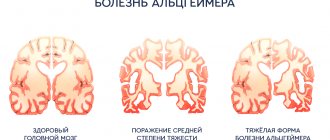
Clinical picture
Paget's disease occurs more often over the age of 40 years, but is likely to be asymptomatic for a long time before detection. Some researchers identify the so-called. juvenile form of the disease (juvenilis Paget), others designate this lesion as hyperphosphatasia.
At the beginning of the disease, pain in bones and joints appears for no apparent reason. In advanced cases, bone deformation occurs.
Skeletal involvement is often asymmetrical. The long tubular bones thicken and become arched. The skull increases in size due to thickening of the bones of the arch and base. Hyperthermia of the soft tissues over the diseased bone is characteristic, caused by its hypervascularization and dilation of the subcutaneous vessels. Restriction of mobility in the joints and lameness develop in advanced cases.
The levels of calcium and phosphorus in the blood and urine may be normal, but high levels of alkaline phosphatase and high urinary excretion of hydroxyproline are often observed.