Gynecologist, physiotherapist-resortologist E.K. Ermolaeva
Sign up for treatment of kraurosis
We are not treated anywhere: we are given a diagnosis and offered to try various ointments one after another!.. But here we receive intensive treatment for this particular area and feel a clear improvement!
From reviews of patients about the treatment of kraurosis
KRAUROSIS is a gross keratinization and atrophy of the skin and mucous membrane of the vulva (external genitalia in women).
Kraurosis is manifested by atrophy (thinning) and sclerotic changes (wrinkling) of the labia majora and minora, and the clitoris.
With kraurosis of the vulva, sexual intercourse, urination, and defecation are DIFFICULT, which makes the treatment of kraurosis of the vulva socially significant.
- STAGE 1 - itching, swelling, hyperemia (redness) of the external genitalia, dry skin and the appearance of microcracks in the skin, decreased sensitivity of the external genitalia (clitoris, labia majora) and the entrance to the vagina.
- STAGE 2 - atrophy (flattening) and thickening (decreased elasticity) of the labia majora and minora, atrophy of the clitoris, narrowing of the vaginal opening, whitish (pale) color of the skin and mucous membrane of the vulva, coarsening of the skin and mucous membrane of the external genitalia, appearance on the skin depigmented areas of the vulva (areas with a lack of pigmentation) and/or pigment spots of various sizes and shapes, a significant decrease in the sensitivity of the vulva (clitoris, labia majora and minora), the entrance to the vagina, a decrease in the hair of the external genitalia. Sexual intercourse becomes painful and requires volitional efforts.
- STAGE 3 (sclerotic) - complete atrophy and sclerosis (wrinkling, “drying”) of the external genitalia: pubic hair is scanty or absent; the skin and mucous membrane of the vulva looks like a crumpled parchment sheet. Against the background of thinning and loss of elasticity of the skin, deep, poorly epithelized (“healing”) cracks and erosions (ulcers), almost complete loss of sensitivity of the vulva, narrowing and sclerosis (roughening) of the vaginal opening often occur. In some cases, complete closure of the vaginal opening is possible. Every sexual intercourse becomes a “test of feelings”, when “it is impossible to refuse, and it is impossible to agree.” After sexual intercourse, desquamation of the vulva and perineum (focal and/or generalized exfoliation of the skin of the external genitalia and perineum), the appearance of single or multiple microcracks, bleeding wounds and erosions (ulcers) are often observed. Desquamated areas (areas with no skin) are very painful, poorly epithelialized (impossible to heal) against the background of antibiotic therapy and traditional conservative treatment. Maintaining the strength of “family ties” requires incredible, sometimes heroic efforts from a woman, bordering on self-denial.
| Photo of kraurosis of the vulva, stage 1. The mucous membrane of the labia minora is thinned, dry, with microcracks |
| Photo of kraurosis of the vulva, stage 2. Atrophy (flattening) of the labia majora and minora, pale color of the skin and mucous membrane of the vulva, narrowing of the vaginal opening, reduction of hair |
| Photo of kraurosis of the vulva, stage 3. Thinning and loss of elasticity of the skin, wrinkling of the external genitalia, clitoral atrophy, narrowing and sclerosis of the vaginal opening, multiple microcracks in the skin |
See all photos of krauroz
Pay ATTENTION to the excellent quality of the photographs, testifying to the expert class of colposcopes of the Women's Health Resort Clinic.
You can find photos of vulvar kraurosis taken by our EXPERIENCED specialists in the treatment of kraurosis on many Russian and foreign websites and in textbooks.
KRAUROSIZATION OF THE VULVA, kraurosis of the perineum DOES NOT HINDER the onset and gestation of PREGNANCY.
The condition of the VULVA and perineum EVEN SOMETHING IMPROVES during pregnancy. However, the high RISK OF MATERNAL INJURY in the form of deep cracks and ruptures of the vagina, vulva and perineum inclines towards delivery by Caesarean Section.
KRAUROSIS OF THE VULVA occurs more often in menopause and very rarely in young women, usually after extirpation (removal) of the ovaries.
Kraurosis of the vulva is NOT SEXUALLY TRANSMITTED, that is, it is not contagious.
| As you age, you stop enjoying many things: clothes, travel, restaurants, cosmetics, cars. Only HEALTH and vigor are always in demand. Vulvar kraurosis only gets worse if treatment is not effective. It is IMPORTANT to start moving in the RIGHT direction now! EVERYTHING you need to know about the right direction in the treatment of kraurosis, see HERE: |
- Causes of kraurosis of the vulva
- Prognosis for kraurosis of the vulva
- Diagnosis of kraurosis of the vulva
- Treatment of kraurosis of the vulva
- Reasonable restrictions for kraurosis
- Questions and answers about kraurosis
- Photos of kraurosis symptoms
Treatment of kraurosis by appointment by multi-channel telephone 8 (800) 500-52-74 (calls within Russia are free), or +7 (for foreign calls).
| ONLINE to an experienced gynecologist about the treatment of kraurosis in Pyatigorsk at BOOK ONLINE for kraurosis treatment here. SIGN UP online for kraurosis treatment here. Buy coursework for treatment by phone or here. |
Booking a course
Kraurosis of the vulva
Kraurosis of the vulva is a chronic, difficult-to-treat pathology in women, characterized by slowly progressive atrophy of the skin and mucous membranes of the external genitalia.
Changes in the epidermis with kraurosis of the vulva resemble the histological picture of lichen sclerosis, so experts often combine these concepts. The term also has other synonyms: lichen sclerosis, lichen sclerosis, white lichen of Tsumbusha. According to ICD 10, kraurosis of the vulva in gynecology has code L90.4.
The disease mainly affects women of pre- and postmenopausal age.
Possible complications
For any type of pathology and treatment outcome, a woman needs long-term observation by a doctor. The main complications of vulvar kraurosis can be the following types of diseases:
- relapse of the disease;
- healing of leukoplakia;
- transition of the main process to neoplasm of the vulva;
- vulvar cancer.
With kraurosis of the vulva, the prognosis for health and life is quite favorable, but only subject to regular visits to the doctor and a mandatory annual preventive examination in a specialized Center. The worst treatment option is a delayed visit to the doctor and late diagnosis of the disease, so any woman with vulvar itching should consult a specialist promptly.
Causes of kraurosis of the vulva
The exact etiology of lichen sclerosis has not yet been established. Since the pathology most often occurs in women 45–55 years old, its onset is associated with a decrease in estrogenic activity. However, this does not explain the reason for the development of the disease in young girls. In addition, there are isolated cases of lichen sclerosis in teenage girls.
In this regard, it is generally accepted that the disease kraurosis of the vulva in women is a reaction to negative factors, which are divided into several groups:
- Viral-infectious - the disease occurs against the background of the human papillomavirus or herpes virus.
- Hormonal – kraurosis develops due to a decrease in estrogen production due to hormonal disorders or natural aging of the body.
- Neuroendocrine – the causes are due to diseases of the endocrine system or an imbalance in the functioning of the hypothalamic-pituitary system.
- Genetic – hereditary predisposition to the disease.
- Autoimmune – the etiology of the disease is associated with autoimmune processes in the body.
- Mechanical - the cause of lichen lies in frequent injuries and chemical burns of the external genitalia, surgical interventions on the genitals, constant violation of hygiene rules (insufficient or excessive care).
Psychological help
Lichen sclerosus (kraurosis) of the vulva can become a factor in emotional and psychological distress. Representatives of the fair sex, and especially young girls, do not want to go to the reception for various reasons. The itching begins and the women don’t know what to think—either her husband brought it, or she picked it up herself.
Meanwhile, the symptoms intensify, unpleasant ulcers form, and it becomes impossible to have sex. Problems begin in the family and personal life. The constant itching and burning is simply driving me crazy. Women's health problems develop into nervous and mental ones.
To avoid bringing yourself to this state, contact the Kuntsevo Medical Center for help. Friendly service staff and the absence of queues will not leave you indifferent.
The doctor will listen to you carefully and help solve your problem. The specialist will work with you on the troubles that have accumulated during this time. You will start a new life! Kraurosis is a curable disease. The sooner you start getting healthier, the better.
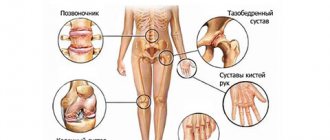
Symptoms of vulvar kraurosis
The clinical manifestations of the disease directly depend on its degree.
There are three stages of vulvar kraurosis: initial, atrophic (thinning stage) and sclerotic (wrinkling stage).
In the initial phase of the disease, symptoms of vulvodynia appear - pain in the vestibule of the vagina, dryness and tightening of the skin of the perineum. The most striking sign of kraurosis is itching. It is usually minor or moderate in nature. But sometimes it causes serious inconvenience, worsening after drinking coffee and spicy foods, contact with water, physical activity, overheating, and also at night. Some women notice slight swelling and hyperemia of the labia. Symptoms characteristic of kraurosis are usually absent; sometimes small isolated whitish spots appear on the tissues.
At the atrophic stage, a characteristic triangle becomes visible with the base in the upper part of the labia minora and the apex in the projection of the pubis. There is a reduction in the clitoris, thinning and flattening of the labia minora. A whitish tint appears on soft tissues.
At the last stage, atrophy progresses and leads to the development of sclerotic changes. What does kraurosis of the vulva look like? The labia minora and clitoris practically “disappear” due to severe atrophy, the labia majora become flattened, hair disappears, the skin and mucous membranes become pearlescent in color. The tissues of the vulva are covered with multiple folds. Minor hemorrhages and cracks appear. The entrance to the vagina sharply narrows, which is why sexual intercourse first becomes painful and later completely impossible. Gradually, the pathological process covers the inguinal folds and the perianal area. There is a narrowing of the urethral opening, which causes pain when urinating. The itching becomes so pronounced that women intensively scratch the affected areas, which is why new microtraumas are constantly formed.
Against the background of pronounced local lesions, patients experience neurological symptoms: emotional stress, depressive, anxious and neurotic states, sleep disturbances.
Itching in the perineum
Symptom of a progressive disease: damage to the anal area.
A complaint of itching in the perineum is the most striking symptom of vulvar kraurosis; it is usually what forces you to seek help from a gynecologist. It is characterized by some features in the form of amplification:
- at night, in the evening;
- overheat;
- after taking hot baths or just contact with water;
- after physical activity;
- eat spicy food, coffee.
If at the initial stage the symptoms are not very pronounced and manifest themselves in the form of tingling in the perineum, then over time they quickly intensify. Patients begin to experience debilitating, persistent and painful itching in the perineal area.
Women came to our emergency department for the treatment of vulvar kraurosis, so exhausted by their condition that they honestly admitted to suicidal thoughts in this context.
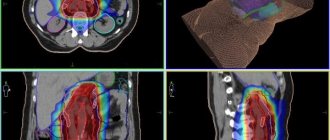
Diagnosis of kraurosis of the vulva
At the initial stage of the disease, due to the lack of specific symptoms, differential diagnosis of kraurosis with vulvovaginitis, neurodermatitis, vitiligo, leukoplakia, lichen planus and diabetes mellitus is important.
As the disease progresses, the clinical picture of vulvar kraurosis is so pronounced that the doctor makes the diagnosis during a routine gynecological examination.
To assess the degree of changes in the skin and mucous membranes, vulvoscopy is performed, and, if necessary, a microscopic examination of a smear from the cervix for flora, a cytological examination of a smear for atypical cells, an immunogram, and a clinical blood test. If malignancy of the process is suspected, a biopsy of vulvar tissue is prescribed with further histological analysis of the biopsy sample.
Differential diagnosis
Differential diagnosis in the early stages should be carried out with the following diseases [1, 2, 13-15]:
- with neurodermatitis - the epithelium is thickened, compacted, dry, the skin pattern is enhanced with inflammatory papules of a brownish-pink color, the skin is hyperemic, shagreen-like, itching appears and on other parts of the body;
— vitiligo is characterized by a lack of pigmentation, sometimes mild itching, and no atrophic changes;
- for lichen planus - multiple grouped papular rashes with atrophic changes or sclerosis with the formation of keloid-like scars;
- with diabetes mellitus - severe itching of the vulva, the tissues of the external genital organs are swollen, have a “doughy” consistency, and are sharply hyperemic.
As a chronic inflammatory dermatosis with a long course of cycles of “itching-scratching-itching” and the formation of scars, SALV is a triggering factor for carcinogenesis or contributes to it. Apparently, dysregulation of immune processes also predisposes to the development of vulvar malignancy.
Treatment
One of the initial measures is the elimination of irritating factors, careful care of the vulva, treatment of secondary infections, local use of estrogens, which prevents atrophy of the vulva and vagina. This consists of following a diet (excluding spicy, salty, sweet foods, caffeine-containing products, alcohol) and intimate hygiene rules (limiting/excluding soap-containing products, deodorants, synthetic underwear, pads, tampons). For severe manifestations of itching, desensitizing therapy and sedatives are recommended [2].
The most widely accepted and recommended gold standard treatment for PALS is topical application of ultrapotent corticosteroid ointments [16], especially clobetasol propionate 0.05% ointment. The anti-inflammatory properties of clobetasol are most effective in the treatment of SALV, which is reflected in the reduction of inflammation and the prevention of progression of the condition and subsequent scarring. Topical ultrapotent corticosteroids are first-line therapy in the treatment of SALV (mometasone furoate, clobetasol proprionate (Ib, A). Clinical guidelines published in 2014 by the American Association of Child and Adolescent Gynecologists suggest the use of highly active glucocorticoid drugs in the long term as first-line drugs mode.They have the following effects:
- anti-inflammatory effect;
- antihyperplastic effect on the proliferating superficial layers of the skin;
- antiallergic, local analgesic and antipruritic properties;
- inhibitory effect on the functions of cellular and humoral immunity.
Summarizing recommendations for the treatment of SALV in children, taking into account the level of evidence, American colleagues presented them as follows:
1. Therapy in patients with SALV should begin with the use of highly active glucocorticoid drugs. Level II-2 B
.
2. There is limited data justifying the possibility of using immunomodulators both when treatment is ineffective and when patients refuse medications with glucocorticoids. Level II-3 B.
3. SALV should be suspected in children if there are complaints of various disorders of urination and defecation, including dysuria and dyschezia. Level C
.
In patients with SALV, it is necessary to exclude autoimmune diseases. It should also be noted that the diagnosis of SALV in children and adolescents does not necessarily require a vulvar biopsy. A biopsy of the skin of the vulva can be performed only if there are areas of the skin of the vulva and perianal area suspicious for atypia and/or with persistent resistance to therapy.
Patients with SALV require mandatory monitoring every 6-12 months to assess complaints, exclude changes in the architecture of the vulva and perianal area, and also to prevent the possible risk of malignancy [6].
As already noted, in the treatment of SALV, super-potent corticosteroids clobetasol or halobetasol in the form of 0.05% ointments are used. Because relapses can be frequent, prolonged, and can lead to atrophy and scarring, long-term maintenance therapy is recommended and is considered safer. Since there are no randomized controlled studies comparing the potency of steroids, the frequency of use and duration of treatment for each patient is selected on an individual basis. According to the results of a study by M. Gurumurthy et al. [17] reported that in a trial of clobetasol propionate ointment, complete remission was achieved in 66% of patients and a partial response to treatment was obtained in 30%. The scars did not progress. Conversely, there was no improvement in 75% of patients without treatment, and progression of scars was observed in 35% of women [17].
Depending on the severity of the clinical effect, modern topical corticosteroids (TCS) are divided into four groups [3, 18, 19] (Table 1):
Table 1. Current topical corticosteroids
- weakly active drugs (hydrocortisone 1%, prednisolone 0.5%, fluorocinolone acetonide 0.0025%);
- drugs of moderate action (alclomethasone dipropionate 0.05%, betamethasone valerate 0.025%, clobetasol butyrate 0.05%, deoxymethasone 0.05%, flumethasone pivalate 0.02 and 2%);
- potent drugs (betamethasone valerate 0.1%, betamethasone dipropionate 0.025 and 0.5%, butesonide 0.25%, fluorolorolone acetonide 0.025%, fluorcinoid 0.05%, fluorcinolone acetonide 0.025%, triamcinolone acetonide 0.02, 0 .1% and 2%, methylprednisolone aceponate 0.1%, hydrocortisone 17-butyrate 0.1%, mometasone fluorate 0.1%);
- drugs with very strong activity (clobetasol propionate 0.05%, difluorocortolone valerate 0.05%, galcinonide 0.1%).
Corticosteroids include halogenated (fluorinated) and non-halogenated ones [18-20]. Fluorinated corticosteroids (dexamethasone, betamethasone, flumethasone, triamcinolone, clobetasol, fluticasone, fluocinolone, flumethasone), as a rule, have greater anti-inflammatory activity, but more often lead to side effects. Non-halogenated corticosteroids include prednisolone derivatives (mometasone fuorate, methylprednisolone aceponate, hydrocortisone acetate and hydrocortisone 17-butyrate) [3, 20].
The mucous membranes of the vulva are relatively resistant to steroids, which suggests using ointments with maximum steroid potency to achieve a good effect. For 2-3 months they are applied daily, then 3 times a week in a thin layer on the vulva. In the circumference of the anus, where the skin is thinner, the ointment is applied daily for 4 weeks, followed by a transition to three times a week, and later - once or twice a week. The effectiveness of treatment is evidenced by a significant reduction in the number of cracks, erosions, hemorrhages and thickened white lesions. Even with effective treatment, they do not always disappear completely.
Various dosing regimens can be used. One of the most common is the daily use of high and maximum potency steroids: once a day for 3 months. In children, to avoid skin atrophy, TCS is used weekly for 3 months.
The use of TCS twice daily has additional benefit in the onset of lichen sclerosus. Proactive maintenance therapy with twice-daily mometasone furoate ointment 0.1% is effective and safe in maintaining remission and may help prevent the occurrence of malignant changes (Ib, A). The use of 30 g of the maximum potency steroid should continue for 3 months.
In postmenopause, long-term, for 6 months, use of corticosteroids of maximum activity is necessary. Within 12 weeks, in 77-90% of observations, it is possible to achieve significant improvement and disappearance of complaints, and in 23% of observations, complete disappearance of skin changes. Long-term treatment allows you to maintain remission of the disease for a long time. The patient should be monitored throughout her life. For thickened, hypertrophied, treatment-resistant lesions, administration of triamcinolone into them can be effective [1]. The use of TCS in combination with antibacterial and antifungal agents, such as gentamicin or fusidic acid and nystatin or azole antifungals, may be advisable when a secondary infection occurs. They can be used for a short period of time to eliminate infection (IV, C).
An allergic reaction to any corticosteroid ointment may occur after prolonged use. It should be taken into account that TCS can change the manifestations of some skin diseases, which can complicate the diagnosis. In addition, the use of TCS may delay wound healing [21].
When carrying out long-term local corticosteroid therapy in the anogenital area, serious side effects are detected:
- skin thinning;
- “rebound” reaction, which occurs when therapy is suddenly stopped and manifests itself in the form of dermatitis with intense redness of the skin and a burning sensation;
- formation of striae;
— development of fungal infections;
- suppression of adrenal function as a result of systemic absorption.
According to research results [2], it has been proven that all side effects resolve quickly as the activity of topical corticosteroids decreases and the frequency of their use.
The selection of treatment tactics for SALV is based on theoretical assumptions. Therapy for patients suffering from SALV is associated with polypharmacy, as it should help simultaneously eliminate the phenomena of atrophy, hyperkeratosis, reduce microcirculatory disorders, inflammation, and improve the healing of erosions on the skin of the vulva and perineum. However, the inappropriate use of antiseptics, antibiotics, antiviral and other groups of drugs often increases the activity of the pathological process and the spread of SALV. In case of lichen sclerosus, long-term observation is necessary to prevent increasing scarring and early detection of malignant neoplasm, the risk of which is not great, but real. As a rule, treatment leads to long-term remission. Its absence is a reason to doubt the diagnosis. A possible complication is contact dermatitis as a reaction to local treatment or excessively careful hygiene, infection, or the development of vulvar cancer. The ineffectiveness of local corticosteroid therapy is often associated with a violation of the patient's regimen, including due to misunderstanding or the inability to fully apply the ointment due to obesity or arthritis. Scars can be painful.
According to the European guideline for the management of vulval conditions 2021, patients with SALV require treatment [21]. About 10% of patients are not pruritic but have clinical signs of lichen sclerosus and should also be treated (IV, C).
In recent years, there has been a debate among specialists about the need to continue further treatment while relieving the initial symptoms. This is due to the fact that there is no data on disease activity at that time. However, it is indicated that SALV can progress further and lead to scarring, despite the lack of symptoms after prophylactic treatment, patients are indicated for continuous therapy for many years to prevent progression (IV, C).
A 5-year follow-up period showed that continuous treatment with an individually selected corticosteroid prevented the progression of symptoms, further scarring and the development of carcinoma, respectively, in 58% of cases versus 93.3%, 40% versus 3.4%, and 0% versus 4. 7% [21].
One of the representatives of the modern generation of TCS is the domestic combination drug for external use - tetraderm (Table 2).
Table 2. Composition of tetraderma cream for external use According to its pharmacological action, it has anti-inflammatory, antibacterial, wound-healing, antifungal, and glucocorticoid effects.
Pharmacodynamics
The activity of the drug is due to the pharmacological properties of the components included in its composition.
Gentamicin is a broad-spectrum antibiotic from the aminoglycoside group. Has a bactericidal effect, active against gram-negative microorganisms: Pseudomonas aeruginosa, Aerobacter aerogenes, Escherichia coli, Proteus vulgaris, Klebsiella pneumoniae
;
gram-positive microorganisms: Staphylococcus aureus
(coagulase-positive, coagulase-negative and some strains producing penicillinase).
Dexpanthenol is a derivative of pantothenic acid. Stimulates skin regeneration, normalizes cellular metabolism, accelerates mitosis and increases the strength of collagen fibers. Penetrates into all layers of the skin. It has a weak anti-inflammatory effect.
Mometasone is a synthetic CS that has a local anti-inflammatory, antipruritic and anti-exudative effect, induces the release of proteins that inhibit phospholipase A2 and lipocortins, which control the biosynthesis of inflammatory mediators (prostaglandins and leukotrienes, cellular inflammatory mediators) by inhibiting the release of their common precursor - arachidonic acid.
Econazole is a synthetic imidazole derivative. It has an antifungal and antibacterial effect, inhibits the biosynthesis of ergosterol, which regulates the permeability of the cell wall of microorganisms. It is easily soluble in lipids and penetrates well into tissues; it is active against dermatophytes Trichophyton, Microsporum, Epidermophyton,
yeast-like fungi of the genus
Candida, Corynebacterium minutissimum,
as well as
Malassezia furfur (Pityrosporum orbiculare)
, which causes pityriasis versicolor, and some gram-positive bacteria (streptococci, staphylococci).
Indications for use of the drug Tetraderm
Treatment of dermatoses of inflammatory origin with concomitant bacterial and mycotic infection or a high probability of secondary infection (simple and allergic dermatitis, atopic dermatitis (including diffuse neurodermatitis), limited neurodermatitis, eczema, dermatomycosis (dermatophytosis, candidiasis, pityriasis versicolor), especially when localized in the groin area and large folds of skin; simple chronic lichen (limited neurodermatitis).
Directions for use and doses
Externally.
The cream is applied to the affected areas of the skin in a thin layer, gently rubbing, 2 times a day until a positive clinical result is achieved. The duration of treatment is individual, depends on the size, location of the lesion and the severity of the disease and is usually 1-2 weeks. It is not recommended to use Tetraderm for more than 4 weeks.
Second-line therapy for SALV
Topical calcineurin inhibitors (TCIs) - pimecrolimus, tacrolimus - have a dermatotropic, immunosuppressive, anti-inflammatory local effect, specifically bind to the cytosolic receptor macrophilin-12 of T-lymphocytes and inhibit calcium-dependent phosphatase - calcineurin. Currently, TICs are recommended as second-line therapy for SALV. Pimecrolimus cream 1% is an immunosuppressant that inhibits T cell activation by blocking the transcription of early cytokines, and thus significantly reduces the itching, burning and inflammation associated with SALV. In addition, it prevents the release of pro-inflammatory cytokines, mediators of inflammation from mast cells in vitro
in response to stimulation by IgE antigen, does not affect keratinocytes, fibroblasts and endothelial cells.
Although TCIs can provide effective symptomatic relief, topical clobetasol is superior to pimecrolimus in reducing inflammation and improving clinical symptoms. However, pimecrolimus cream has a more acceptable safety profile and does not cause skin atrophy, although its use is associated with an increased risk of complications due to suppression of local immunity. As a result, TCI should be administered under the supervision of a specialist who can monitor the potential risk of malignancy of SALV. Given the proven effectiveness and safety of topical corticosteroids, experts agree that TICs should be reserved for cases of SALV not responding to topical corticosteroids [2].
TIC is used externally 2 times a day, applied in a thin layer to the affected areas of the skin and gently rubbed until completely absorbed. Treatment is continued until symptoms disappear completely. At the first signs of relapse, therapy should be resumed. If symptoms persist for 6 weeks, the patient's condition should be re-evaluated.
The most famous forms of TEC:
1. Tacrolimus - Protopic ointment 0.03 and 0.1%. Undesirable effects of this drug include: burning and itching sensation, redness, pain, irritation, rash at the application site, development of folliculitis and acne. Isolated cases of malignancy (skin and other types of lymphomas, skin cancer) have been recorded.
2. Pimecrolimus - Elidel cream 1%. Side effects include a burning sensation at the site of application of the cream, the development of impetigo and skin infections, rhinitis, and urticaria.
The most relevant seems to be 0.03% tacrolimus ointment for the effective treatment of children with anogenital lichen sclerosus 2 times a week, while reducing relapses is possible (IIIA, B). A comparison of pimecrolimus (1% cream) and clobetasol propionate (0.05%) cream showed an improvement in the symptoms of itching, burning, pain 12 weeks after the onset of vulvar lichen sclerosus, while clobetasol was used to quickly relieve the inflammatory process (Ib, A) . Other studies of pimecrolimus showed that 42% of patients were in “complete remission” after 6 months of use (IIb, B). Local irritation was the most common side effect with tacrolimus and pimecrolimus. The long-term risks of TIC use still need to be studied, as there are concerns about the possibility of an increased risk of malignancy due to local immunosuppression with long-term SALV therapy [21].
Emollients
One of the important components of SALV therapy are emollients ( eng.
. emollient - emollient) softening and moisturizing agents. These products do not contain potential allergens such as propylene glycol and lanolin, can minimize local inflammation, increase the moisture content of the stratum corneum of the skin, strengthen weakened skin barrier function and reduce subclinical inflammation [2].
According to the results of a study conducted by T. Simonart et al. [22], it was found that more than 50% of women who used a daily moisturizer along with topical corticosteroids maintained remission for 58 months. And more than 2/3 of women stopped using topical corticosteroids while remaining on emollients for a long time.
Based on their source of origin, emollients are divided into plant (natural), chemical and synthetic. Plant emollients are, first of all, natural oils. They soften the skin and protect it, making it elastic. They are absolutely harmless. These include popular cosmetic oils: peach, olive, jojoba. Chemical emollients include paraffin, petroleum jelly and ointments based on it (“Propolisnaya”, “Calendula”), and mineral oils. Synthetic emollients are produced industrially by carrying out various reactions and mixing fatty acids, esters and other components. These are cyclomethicones, dimethicones and synthetic oils. The most well-known and studied are the products from the Emolium, Locobase Ripea, and Lipikar line.
Effects of emollients:
— begin to act immediately after application to the skin, reducing moisture evaporation due to the occlusion effect;
— with further penetration into the stratum corneum, the lipids replace the missing lipids of the epidermis and maintain skin moisture for several hours (medium-term effect);
- lipids reach the deeper layers of the skin and enter the empty “storage areas” - lamellar bodies; if necessary, they are released to maintain the water-lipid balance of the skin (long-term effects).
Estrogen-containing drugs
This group of funds
has a proliferative effect without having a systemic effect on the endometrium and mammary glands [23, 24]. Orniona cream is one of the most modern domestic preparations that contains estriol, an analogue of the natural female hormone. Estriol is used to correct estrogen deficiency in pre- and postmenopausal women. Effective in the treatment of urogenital disorders. In the case of atrophy of the epithelium of the vagina and cervix, which occurs with SALV, estriol stops these disorders, helps restore normal microflora and physiological pH of the vagina, thereby increasing the resistance of the vaginal epithelium to infectious and inflammatory processes. Unlike other estrogens, estriol interacts with the nuclei of endometrial cells for a short period of time, so that with daily use of the recommended daily dose, endometrial proliferation does not occur. Thus, there is no need for cyclic additional administration of progestogens, and “withdrawal” bleeding is not observed in the postmenopausal period.
Indications for use:
- hormone replacement therapy (HRT) for the treatment of atrophy of the mucous membrane of the lower urinary and genital tract associated with estrogen deficiency in postmenopausal women;
— pre- and postoperative therapy in postmenopausal women who are about to undergo or have already undergone surgery via vaginal access;
- for diagnostic purposes in case of unclear results of cytological examination of the cervical epithelium against the background of atrophic changes (as an adjuvant).
Contraindications for use:
- established hypersensitivity to the active substance or to any of the excipients of the drug;
- untreated endometrial hyperplasia;
- established, known or suspected breast cancer;
- diagnosed or suspected estrogen-dependent tumors (for example, endometrial cancer);
- bleeding from the vagina of unknown etiology;
- thrombosis (venous and arterial) and thromboembolism currently or in history (including deep vein thrombosis, pulmonary embolism, myocardial infarction, stroke), cerebrovascular disorders;
- conditions preceding thrombosis (including transient ischemic attacks, angina) currently or in history;
- congenital or acquired predisposition to the development of arterial or venous thrombosis, for example deficiency of protein C, protein S or antithrombin III;
- liver disease in the acute stage or a history of liver disease, after which liver function tests have not returned to normal;
- porphyria;
- pregnancy and breastfeeding.
Directions for use and doses
Ornion cream should be inserted into the vagina before bed using a calibration applicator. One dose (when filling the applicator to the ring mark) contains 0.5 g of Ornion cream, which corresponds to 0.5 mg of estriol. The course of treatment consists of prescribing estriol at a dose of 500 mcg per day for 2-3 weeks daily, then switching to a maintenance dose 1-2 times a week. A small part of a single dose is applied directly to the vulva, and the rest into the vagina with a dispenser. With the detachment of hyperplastic plaques, there is increased pain that passes quickly.
Ornion cream can be used both in women with a history of hysterectomy and in women with an intact uterus. When carrying out HRT for the treatment of atrophy of the mucous membrane of the lower urinary and genital tract associated with estrogen deficiency in postmenopausal women, one intravaginal cream is administered daily for no more than two weeks until symptoms alleviate. Then the dose is gradually reduced to a maintenance dose depending on the clinical picture (for example, one injection 2 times a week).
For pre- and postoperative therapy in postmenopausal women who are about to undergo or have already undergone surgery via vaginal access,
- Magazines
- Subscription
- Books
- For advertisers
- Delivery / Payment
- About the publishing house
- Contacts
- Privacy Policy
- Publishing house "Media Sphere"
Registration
- Telephone
- +7 (495) 482-4118
- +7 (495) 482-0604
- +8 (toll-free number for subscription questions)
- Mailing address
- Publishing house "Media Sphere",
- PO Box 54, Moscow, Russia 127238
- [email protected]
- © 1998-2021
+7 (495) 482-4118, +7 (495) 482-0604
- PO Box 54, Moscow, Russia 127238 "Media Sfera Publishing House"
- [email protected]
© 1998-2021
- Publishing house "Media Sphere"
Email confirmation
An email has been sent with a link to confirm your email. Follow the link from the email to complete registration on the site.
Email confirmation
Log in to the site using your account in one of the services
Registration for legal entities
To come in
Register
Treatment of kraurosis of the vulva
How to treat kraurosis of the vulva? The etiology and pathogenesis of the disease have not been established, so therapy is a rather difficult task. The regimen is selected individually depending on the prevailing symptoms, the degree of atrophy and sclerosis. The main goal is to eliminate inflammation, reduce itching, improve tissue trophism, and normalize the patient’s psycho-emotional state.
For external treatment, hormonal ointments are prescribed for vulvar kraurosis: for young women of childbearing age - based on progesterone (for example, Crinon or Prajisan), for older women - containing estrogen (Permarin, Estriol).
Almost all patients with vulvar kraurosis need treatment with ointments based on glucocorticosteroids (prednisolone, hydrocortisone, betamethasone). They have anti-inflammatory, antiallergic, antiexudative, immunosuppressive, epidermostatic and antipruritic effects.
Systemic therapy includes taking the following medications:
- hormonal medications (estrogens, progesterone);
- sedatives (valerian, motherwort);
- anxiolytics (fabomotizol, hydroxyzine);
- antihistamines (loratadine, clemastine);
- immunomodulators (tactivin, azoximer bromide);
- biostimulants and vitamins.
Physiotherapeutic procedures are also effective: laser and ultrasound therapy, phonophoresis (including with glucocorticoids), ozone therapy, etc.
Treatment is carried out in several stages.
The first stage is blocking inflammation in the skin
At this stage, external preparations of glucocorticosteroids in the form of creams are used. At this stage, the patient reduces itching and gets relief. It is important not to stop treatment, because after stopping the creams, the process resumes with renewed vigor. You cannot continue using glucocorticosteroids without a doctor’s prescription!
The second stage is restoration of the skin structure
PLASMOTHERAPY and hyaluronic acid preparations are used. Among the most modern drugs is REVI Reform. The drug helps stabilize cell membranes under stress, creates conditions for normal cell functioning, which fights toxins and free radicals due to such a component as Trehalose.
REVI Reform creates conditions for normal cell functioning by reactivating drainage and blocking the action of inflammatory factors such as cytokines and interleukins.
- Promotes natural renewal process
- Restores barrier, trophic, plastic function of tissues
- Adaptogenic and immunoprotective effect at the local level, protects against viral and bacterial infections
- Analgesic effect
Prognosis and prevention
How to cure kraurosis of the vulva is unknown. Usually it is not completely cured, but properly selected therapy helps reduce negative symptoms and improve a woman’s quality of life.
Basic clinical recommendations for vulvar kraurosis:
- observe the rules of personal hygiene;
- do not wear synthetic or tight-fitting underwear;
- do not use sanitary pads;
- do not use gels, sprays and deodorants in the intimate area;
- to refuse from bad habits.
The disease requires regular consultations with a gynecologist and ongoing treatment. A properly selected diet and a calm emotional state are of no small importance.
Efficiency
The effectiveness of treatment methods will depend on the patient and the duration of the disease. The sooner a woman seeks help, the faster the recovery will go. During therapy, be sure to follow the basic rules:
- tune in to constant hygiene, without soap - with a herbal solution;
- wear comfortable cotton underwear;
- give up intimacy;
- at night, use a light blanket;
- exclude spicy and fatty foods from your diet;
- do physical therapy exercises if your doctor advises;
- take walks before bed.
Gradually you will rehabilitate your intimate life, which is important. The main thing is to listen to your gynecologist. And you will get better quickly.
Frequently asked questions about vulvar kraurosis
What causes kraurosis of the vulva?
The exact causes of the disease have not yet been established. It is assumed that viruses and infections, hormonal changes, disruption of the endocrine system, and autoimmune processes can serve as trigger factors.
How can I tell if I have vulvar kraurosis?
The main symptoms of the disease are itching, dryness, pain in the vestibule of the vagina, tightening of the skin of the perineum. Over time, the clitoris becomes smaller, the labia minora becomes thinner, the entrance to the vagina narrows, and the tissues atrophy.
Is it possible to cure lichen sclerosus?
The disease cannot be completely cured, but properly selected therapy can eliminate unpleasant symptoms and improve a woman’s quality of life.
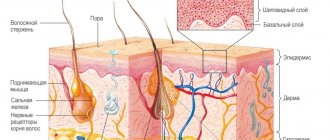
Pathogenesis of the disease
The pathology begins with atrophy of the papillary and reticular layers of the epithelium and epidermis. Then the elastic fibers die. A fibrillar protein, hyaline, appears in the connective tissue cells, the cell membranes are compressed, the cytoplasm becomes denser, and the function of the cells themselves is reduced to a minimum. Connective tissue disintegrates.
In the affected area, the epidermis first grows, new growths such as warts and foci of inflammation appear, then the volume of the skin of the labia decreases, sometimes the skin completely disappears. The mucous membrane becomes dry, brittle, and the pigment disappears. The passage into the vagina is greatly reduced due to scarring of the tissue of the genital organs.