Gonarthrosis is arthrosis of the knee joint, a chronic non-inflammatory disease manifested by the progressive destruction of intra-articular cartilage, which is accompanied by abnormal formation of the bones that form the joint, changes in the synovial membrane and synovial fluid.
Gonarthrosis is the most common type of arthrosis. Many people experience knee pain, especially after sitting for a long time without moving, such as after a day of work in the office. It is very likely that gonarthrosis is the cause of such discomfort.
This degenerative disease often develops with age, as stress in the knee, which cannot be avoided in various life situations, inevitably leads to wear and tear of the cartilage over the years. At first, a person feels pain when starting to move after long periods of lying or sitting, but this quickly passes. However, as the disease progresses, knee pain increases and begins to significantly limit a person's ability to move normally in daily activities.
In more than half of the cases where arthrosis affects the knee, both knees are affected at once. In the category of patients from 65 to 75 years old, gonarthrosis is detected in 35% of women and 21% of men.
Features of the development of osteoarthritis of the knee joint
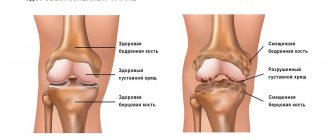
Osteoarthritis of the knee joint
is a common pathology that belongs to the category of the most common diseases that have an extremely negative impact on a person’s quality of life.
Degenerative-dystrophic processes most clearly manifest themselves in the form of physical dysfunction of the legs, accompanied by severe pain. Depending on how much the pathological process progresses, further forecasts for the course of the disease are made.
One of the disappointing forecasts is paralysis of the lower limbs. The seriousness of the consequences of pathological processes necessitates seeking qualified medical help.
Classification of changes
In the taxonomy of arthrosis, several defining criteria are used: causes and etiology, localization, area of coverage.
By etiology:
- primary arthrosis - develops independently, affecting completely healthy joints, without the participation of previous pathologies;
- secondary – formed against the background of a disease (gout, psoriasis, rheumatism), as well as in the presence of existing joint deformities or injuries.
By coverage:
- local forms - affecting a limited number of joints: monoarthrosis - 1 joint, oligoarthrosis - 2-3;
- generalized forms - various types of polyarthrosis, when 3 or more large structures are involved in the pathological process.
Based on the localization of the process, arthrosis of each joint is named separately:
- coxarthrosis – disables the hip joint;
- spondyloarthrosis – affects the intervertebral discs, mainly of the cervical, thoracic and lumbar regions;
- gonarthrosis – with disruption of the knee joint; one of the most common types;
- crusarthrosis – involving the ankle in the pathological process.
Arthrosis can be rapidly or slowly progressive, compensated or decompensated.
What causes lead to knee arthrosis?
To identify the causes of arthrosis of the knee joint, it was necessary to conduct a large number of studies. Many years of examinations of patients and a thorough study of the clinical picture of the pathology allowed specialists to come to the conclusion that the influence of a number of negative factors is the root cause of the destruction of joint tissue, causing severe pain and inflammation.
Among the main reasons leading to degenerative-dystrophic processes, it is worth highlighting:
- previous injuries - a bruise, dislocation or fracture of the knee automatically classifies a person as a risk group and can cause the development of the disease. Damage to the joint presupposes its fixation, and long-term immobility is a direct path to the formation of arthrosis;
- strong physical activity - intense stress on the knees (especially in older people) leads to microtraumas, which also leads to the development of negative pathological processes;
- insufficiently strong ligamentous apparatus - abnormal joint mobility also negatively affects their condition, which manifests itself mainly in old age;
- excess body weight - extra pounds can cause irreparable damage to the knee joints, because the likelihood of meniscus injuries in this case is incredibly high. If a lot of weight is accompanied by varicose veins, then there is a high probability of developing severe forms of arthrosis of the joints of the lower extremities;
- metabolic disorders - a failure in the exchange of nutrients and elements in the body provokes the development of various kinds of diseases, which is caused by insufficient supply of various tissues, in particular bone and cartilage;
- increased levels of stress - worries and worries negatively affect not only people’s mood, but also the level of physical well-being.
General information
Arthrosis is diagnosed in approximately 1/5 of the world's population, but the disease is more common among older people. This is proven by the statistics of its distribution among different ages:
- youth under 40 years old – no more than 6-7%;
- persons of mature age after 45 years – up to 20-25%;
- after 70 years – up to 80%.
The disease affects tissues that are under constant stress: small joints of the hands and metatarsals of the feet, hip and knee joints, areas in the cervical and thoracic spine, and, a little less often, the ankle and shoulder joint.
On a note! Damage to the interphalangeal joints of the hands occurs 10 times more often in women than in men.
In many Western countries, the term “arthrosis” is not used, replacing it with the concept “arthritis”. Such a substitution is completely justified, since inflammatory processes in most cases precede arthrosis or accompany it. In domestic medicine, the terms “arthrosis” and “arthritis” essentially mean the same disease, but with a different etiology of the process. Additionally, the concepts osteoarthritis, osteoarthritis, and deforming osteoarthritis are used to denote pathology.
On a note! The difference between arthritis and arthrosis lies in the cause of the disease. In the first case, these are inflammatory processes (the suffix -itis means inflammation), in the second - metabolic disorders (protein, mineral).
Characteristic symptoms of arthrosis of the knee joint
The symptomatic manifestation of the disease allows timely tracking of the onset and development of pathological processes, which gives each patient the opportunity to recover.
Before determining who to turn to for help and how to treat arthrosis of the knee joint, it is important to become familiar with the symptoms of the disease.
Only a specialist competent in this matter can identify the presence and confirm the diagnosis by prescribing treatment for knee arthrosis. However, every patient should know the main symptoms of knee osteoarthritis, among which are usually identified:
- pain - discomfort that gradually develops into painful sensations does not appear immediately. Their slight manifestation in the knees can bother a person for many years, but at some point they may become stronger, and they will not stop in a calm state;
- crunch – “clicks” when flexing/extending a joint are an alarm bell, which manifests itself already in the second and third stages of the disease;
- synovitis is an inflammation of the joint membrane, in which fluid accumulates, which leads to local swelling;
- deformation is a characteristic feature that appears in the last stages of the disease, accompanied by pronounced inflammation and swelling.
Diagnosis of arthrosis of the knee joint
Diagnosis and treatment of arthrosis of the knee joint is carried out by an orthopedist or rheumatologist. If you wish to undergo a diagnostic examination, each patient can contact a therapist, who will give a referral to a specialist or independently take a voucher to one of them.
The main diagnostic tool of specialists is, of course, an X-ray machine. Thanks to the image taken, you can track not only the presence of pathology, but also the degree of its development.
It is important to note that x-rays can exclude the possibility of the presence of other diseases of the musculoskeletal system.
X-ray examination opens up the opportunity for a specialist to:
- track the narrowing of the joint space;
- detect compaction in joint tissues.
The combination of clinical symptoms and information obtained from the image provides high-quality diagnosis and diagnosis, with the determination of further treatment for osteoarthritis of the knee joint.
Endoprosthetics
Endoprosthetics
- computer navigation systems are used that perfectly calculate all angles, distances and biomechanical axes when installing an endoprosthesis;
- new, increasingly high-quality artificial joints are appearing, almost completely areactogenic (not rejected by the body), very functional (providing a high range of motion), capable of serving for decades;
- Minimally invasive techniques for installing artificial joints are used with minimal damage to soft tissue, which shortens the rehabilitation period and reduces the risk of complications.
Already on the first day after endoprosthetics, a person is recommended to put weight on the operated leg. Rehabilitation lasts several months. After six months or a little more, the person is allowed to bear full weight on the operated leg.
Degrees of osteoarthritis of the knee joint
Modern medicine divides knee arthrosis into several degrees, in accordance with the nature of the development of pathological processes.
To begin with, it is worth noting that according to observations, the disease can have a different nature:
- unilateral (right-sided/left-sided);
- bilateral.
In addition, the pathological process has three stages of development, each of which has its own clinical picture.
1st degree arthrosis of the knee joint
The initial stage of the development of pathology, the successful diagnosis of which is an incredible success not only for the patient, but also for the attending physician.
The peculiarity of the degree of development of arthrosis at this stage is the absence of clinical signs and clear symptoms. Identification of the disease can be carried out during medical examination or during the study of another disease.
Evidence of grade 1 arthrosis of the knee joint may be:
- local discomfort in the knee area during long walking;
- mild pain that disappears with rest.
It is important to note the fact that pain can be felt in one or both joints of the lower extremities.
It is interesting to note that left-sided gonarthrosis is often diagnosed in left-handed people, while right-sided gonarthrosis is typical for people involved in various sports.
2nd degree arthrosis of the knee joint
Symptoms of the second degree of development of pathology are accompanied by an expansion of signs, which are usually included:
- pronounced pain syndrome;
- stiffness and severe discomfort in the knee joint;
- atrophy of the muscles located near the knee joint, which is caused by tissue damage;
- increased pain;
- visually noticeable deformation of the joint;
- limitation of mobility.
Expanding the symptoms simplifies the diagnostic process. Changes characteristic of grade 2 arthrosis of the knee joint are easy to track during palpation. When undergoing a clinical examination, a specialist can easily detect an abnormal formation in the knee area.
3rd degree arthrosis of the knee joint
It is almost impossible not to notice the third degree pathology, because the patient faces constant pain. In addition, the progress of the disease reaches a critical point, which is manifested by severe deformation of the joint, in which the limb completely loses the ability to flex/extend.
The lack of proper treatment leads to complete destruction of the cartilage and, as a consequence, the development of ankylosis (fusion of articular bones).
The only solution for the final stage of development of the disease is an expensive surgical intervention, involving the removal of remnants of cartilage tissue or joint replacement.
What are chondroprotectors
Unique products in this group protect articular cartilage. Regular, course intake is a good prevention of pathology. The use of chondroprotectors can prevent cartilage damage and restore it in case of disease.
The effect of the chondroprotector group is due to glucosamine and chondroitin sulfate. Each component has properties that have a beneficial effect on the joint.
Glucosamine is a natural component of healthy cartilage, under the influence of which substances of cartilage tissue are synthesized. It will protect against peroxidation, free radicals and other destructive effects on cartilage. In case of pathology - anti-edematous effect, reduces the inflammatory process of joints.
Chondroitin sulfate is a stimulator of the formation of cartilage substances: glycosaminoglycans, proteoglycans, collagen, hylauronic acid. Protects cartilage from destruction. Under the influence of chondroitin sulfate, the production of synovial fluid inside the joints is stimulated. In case of arthritis, it reduces the inflammatory process.
A good chondroprotector protects a complex or simple joint from destruction in case of pathology, and helps the structures recover.
Chondroprotectors are different: monocomponent or combined. With simultaneous exposure to chondroitin sulfate and glycosaminoglycan, complete restoration of cartilage tissue occurs.
Receiving treatment with these drugs is often necessary.
How to treat arthrosis of the knee joint?
The level of modern medicine is at a fairly high level, which ensures successful treatment of various types of diseases. Osteoarthritis of the knees is no exception.
Today, there are a large number of methods for treating arthrosis of the knee joint.
At the initial stages of pathology development, predominantly conservative treatment methods are used. Conservative therapy includes:
- physiotherapeutic procedures;
- physical therapy (physical therapy);
- visiting various massages.
Progressive methods of treating osteoarthritis of the knee joint are also actively used. Among the modern effective ways to combat dangerous pathologies are the following:
- Ozone therapy is a local effect of ozone on the affected joint tissues. Helps reduce pain and stop inflammatory processes. Improves blood circulation in the problem area;
- kinesitherapy is a set of exercises for arthrosis of the knee joint, aimed at increasing its mobility and increasing blood flow.
Treatment of knee arthrosis with physiotherapy
Physiotherapy is one of the most popular methods of treating knee osteoarthritis.
Methods of physical influence, subject to a certain number of conditions, have the most positive effect on the area of localization of pathologies of various types.
Physiotherapy includes procedures such as:
- electrophoresis;
- ultraphonophoresis;
- irradiation with laser/infrared radiation;
- pulsed magnetic therapy.
The effectiveness of the procedures is individual and depends on the quality of the patient’s basic treatment plan.
Massage as a treatment for osteoarthritis of the knee joint
Massage is a useful addition to the treatment strategy for knee arthrosis.
Most experts around the world are of the opinion that massage is a mandatory component of the treatment of symptoms of arthrosis of the knee joint, which has a beneficial effect on metabolic processes and helps speed up recovery.
Knee massage can be performed both at home and within the walls of a hospital. The main thing during massage is preliminary high-quality warming up of the joint and compliance with the optimal duration of the process (from 10-15 minutes).
Treatment of osteoarthritis of the knee joint with massage should include techniques such as stroking, rubbing and kneading.
Gymnastics and exercise therapy for arthrosis of the knee joint
Exercises for arthrosis of the knee joint are an effective way to eliminate unpleasant symptoms and treat the disease.
The process of treating knee arthrosis is a rather complex and lengthy process, and physical therapy is an excellent assistant in achieving the desired result.
The type of exercise therapy and exercises for arthrosis of the knee joint are selected by a specialist individually, depending on the degree of development of the pathology and the general state of the patient’s physical fitness.
The main principle of gymnastics for arthrosis of the knee joint sounds like this: no increased loads on the affected joint, only rational, calm actions.
Endoprosthetics
Advanced arthrosis sooner or later requires joint replacement. This is the main treatment method for such patients. Millions of such operations are performed annually around the world. They are becoming more and more effective and safe.
The essence of the operation is that the person’s own joint is removed. An artificial endoprosthesis is installed in its place. It has sufficient functionality for a person to lead a physically active lifestyle. Even operations carried out over decades were mostly successful. Today their effectiveness is even higher because:
Drugs for the treatment of osteoarthritis of the knee joint
Drug treatment for arthrosis of the knee joint is used to relieve symptoms such as pain and swelling, as well as to activate regenerative processes.
Drugs for the treatment of arthrosis of the knee joint can come in different forms (ointments/gels, tablets or injections, patches).
IMPORTANT! Any medication must be prescribed by a specialist as part of an existing treatment plan developed taking into account the symptoms of knee arthrosis.
Self-medication is unacceptable and can lead to extremely negative consequences, in particular, paralysis of the lower limbs and disability.
Painkillers for arthrosis of the knee joint
Used to eliminate symptoms of arthrosis of the knee joint.
Painkillers play an important role in the treatment of arthrosis of the knee joint, because their use improves the patient’s well-being and gives him the opportunity to get a good night’s rest.
Relief of pain is achieved through the action of active substances. The most effective tablets for pain in arthrosis of the knee joint are considered to be “Ketanol” and “Nimesulide”.
Antispasmodics for osteoarthritis of the knee
Prescribed as active assistance. A key area of focus is the fight against spasms.
The active substances included in the preparations help relax the muscle frame and provide pain relief.
Among the frequently prescribed ones, it is worth highlighting Mydocalm.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Treatment of arthrosis of the knee joint with drugs of this type not only eliminates pain, but also slows down and completely eliminates the progress of pathological processes.
Regular use of medications allows you to observe a constant concentration of active components, which guarantees a positive effect.
Artradol is considered to be the most effective NSAID.
Chondroprotectors for arthrosis of the knee joint
The main assistants in the treatment of arthrosis of the knee joint are chonroprotectors.
The active effect of chondroprotectors for arthrosis of the knee joint is aimed at restoring motor ability, which is due to the microelements included in the composition, which are an integral component in the process of building cartilage tissue.
The peculiarity of the principle of action of drugs involves a rather long, but at the same time effective process of getting rid of osteoarthritis of the knee joint.
Among the most effective and affordable drugs, it is worth highlighting Artracam, Structum and Chondroxide.
Osteochondral mosaic plastic surgery
Osteochondral mosaic plastic surgery
- the presence of a limited defect of articular cartilage no more than 4 square centimeters;
- good quality of the cartilage surrounding the articular defect (pathological changes no more than grade II according to Outerbridge);
- the defect is located in the loaded area of the femoral condyle;
- There is donor material in sufficient quality and quantity.
For extensive defects of the cartilage surface, surgery is not performed. It is also not performed if it is impossible to obtain sufficient quantities of high-quality cartilage tissue from donor areas of the body.
Abrasive chondroplasty
This is a palliative operation. It reduces pain but does not prevent further wear and tear of the cartilage. During surgery, the hyaline cartilage is “polished.” Damaged fragments are removed. The thickness of the removed layer is 1-3 mm. After the procedure, a blood clot forms and cartilage-like tissue forms to cover the defect. The technique gives good early but poor delayed results. The operation does not have a drastic effect on the outcome of arthrosis.
Diet and general nutritional recommendations for arthrosis of the knee joint
A diet for arthrosis of the knee joint is necessary for patients with excess body weight. A low calorie diet and a wealth of nutrients will ensure weight loss and accelerate the recovery process of affected joints.
Nutrition for arthrosis of the knee joint should first of all be balanced. The daily diet should contain dishes enriched with beneficial vitamins and microelements necessary for the regeneration of joint tissues and maintaining the balance of the entire body.
It is recommended to give up not only bad habits (alcohol abuse and smoking), but also such dishes as:
- store-bought semi-finished products;
- fatty, spicy and overly salty foods;
- sweet carbonated drinks.
For convenience and competent planning of the diet, when treating knee arthrosis, it is recommended to keep a food diary, which disciplines and helps facilitate the process of restructuring the usual lifestyle.
Disease prevention
Complete recovery is almost impossible, so prevention should be given special attention. The main requirement is a healthy lifestyle and complete treatment of inflammatory processes:
- Avoid hypothermia and promptly treat infectious diseases;
- avoid physical overload and prolonged static loads;
- maintain normal body weight;
- adhere to a proper diet - a balanced composition of vitamins and minerals is very important for the health of the musculoskeletal system;
- fully (if possible, until complete recovery) treat any joint damage;
- practice systematic physical exercise to stimulate blood circulation (cycling, walking, light jogging, Nordic walking).
If you are at risk (old age, poor heredity, physical overload), be sure to undergo regular X-ray examinations.