Bone pain in cancer patients is usually caused by tumor cells that have invaded the bone, in other words, metastases. Bone pain is often the first sign of bone metastases, which is why it is necessary to verify or reject this assumption.
The treatment of such bone injuries itself is aimed at reducing pain, reducing the risk of fractures, and preventing or slowing down the development of other complications.
Cause
So, a very common cause of bone pain is metastatic cancer. That is, the doctor and the patient are no longer faced with primary, but with secondary oncology. Atypical cells of a primary disease of any organ can damage bone and cause pain.
Moreover, it is the bones that are most susceptible to metastasis of atypical cells into them, which often penetrate there with the bloodstream, attaching to the vascular wall of the network of capillaries located in the bone tissue.
Another way (this happens much less frequently) of penetration of atypical cells into the bone is ingrowth from a tumor localized in the immediate vicinity.
The cause of pain is the disruption of the normal functioning of bone cells by cancer cells. This changes the structure of bone tissue.
When a bone is healthy, it constantly undergoes the process of destruction of old tissue and the formation of new one. Once in the bone, atypical cells disrupt this balance. The attacked periosteum (bone membrane) and nerves react to the invasion, causing pain.
Anatomy of the lower leg
The leg and ankle are a complex mechanical structure, the correct operation of which ensures full motor activity of the whole organism. There are three bones in the ankle joint. Their interaction must be correct, in combination with the functions of connective tissue elements, ligaments, muscles and tendons.
The foot has 20 bones, 30 joints, 100 muscles, ligaments and tendons. Their work must happen correctly and harmoniously. When at least one function of the general mechanism is disrupted, certain pathological processes begin to develop. They are accompanied by pain in the lower legs.
The shin is the part of the lower limb that connects the knee to the heel. The tibia contains the tibia and fibula, to which the kneecap is attached. Near the heel, these two bones merge into the anterior and posterior malleolus. There are muscles throughout all parts of the lower leg. With their help, the foot bends, extends and rotates. In most cases, the appearance of pain in the lower leg is not associated with serious pathologies. However, the help of a doctor is mandatory.
Diagnosis of metastases
As a rule, bone metastases are found in the central region of the skeleton, but, of course, they can damage absolutely any bone.
To detect bone metastases, fluoroscopy or a bone scan is performed. This helps to understand what caused the pain syndrome.
During the scan, the patient is injected intravenously with a special radioactive substance that circulates throughout the body and enters the bones. If the substance is too concentrated in a certain location, this indicates the presence of atypical cells.
Of course, pain can be caused by other pathologies, for example, arthritis. The thing is that if the pain is caused by an oncological process, it has one quality - permanence. Bone pain that lasts a week or two is a good reason to visit a doctor.
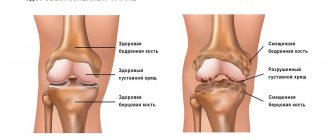
Arthrosis and arthritis: what is the difference
Both diseases affect human joints. The quality of life of people who suffer from one of these illnesses is significantly reduced. Although the names of the diseases are similar, their symptoms and manifestations are very different.
Osteoarthritis affects the cartilage of the joint and nearby bones. It is more common in older people. It can be caused not only by age, but also by heavy physical labor or sports activities.
It is difficult to call arthrosis inflammation. But some doctors believe that it is precisely because of the inflammatory process that this disease begins to progress. The cartilage and bone tissues that are located near the joint undergo changes over time. This happens due to the stress that they experience every day. The disease develops slowly.
Arthritis is inflammation that occurs in a joint. It can almost completely destroy cartilage. Unlike arthrosis, this disease is more common among the young population.
The development of the disease and inflammatory process occurs due to autoimmune factors. That is, immunity independently affects the human body. This process can start due to genetic disorders or infectious diseases.
Inflammation is the culprit behind the onset of arthritis. Bacteria that infect the body's cells have antigens similar to its protein. Therefore, he begins to attack his own tissues. Most often, not only joints are affected, but also internal organs. It could be the heart or kidneys. Few people know that in this case, doctors recommend removing tonsils if a person often suffers from sore throats. Otherwise, there is a high risk of complications in the cardiovascular system and other organs.
If we compare arthritis with arthrosis of the foot, the second disease is more acute. Its symptoms are pronounced, so they are difficult to confuse with something else. Arthritis manifests itself in the form of swelling, severe pain, as well as other, not the most pleasant symptoms.
How the disease will develop in the future depends on the type of arthritis. Almost always, after an acute form, the disease “slows down” and then becomes chronic. Some changes in the joints remain forever, so new outbreaks of osteoarthritis are possible. Sometimes relapses occur and the disease again enters an acute form, joint pain and swelling appear, and the temperature rises.
Osteoarthritis, an inflammatory condition, can be controlled with anti-inflammatory medications. But osteoarthritis is much more difficult to treat, since it mostly remains in a chronic form, changing and destroying joints over a long period of time.
Clinical manifestations
Once it occurs, the pain syndrome provoked by metastases is moderate in nature. It intensifies after physical activity or at night.
As the tumor process develops, the symptoms also intensify. The pain syndrome becomes pronounced and painful.
There are other “signals” indicating the presence of bone metastases:
- Spinal cord compression. It happens quite rarely, but it makes life quite difficult. The thoracic spine or the lumbar and cervical sections are subject to compression.
- Hypercalcemia. The level of calcium in the blood increases, which ultimately leads to a malfunction of many body systems. The complication is very common.
- Pathological fractures. The femur in the area of the diaphysis or neck often suffers.
Patients with late stages of cancer also exhibit symptoms such as:
- Temperature increase;
- Exhaustion;
- Weakness, etc.
Treatment of lower leg pain due to various diseases
Depending on the established diagnosis, doctors draw up a treatment algorithm. Often, pain in the lower leg is caused by increased physical activity and prolonged walking. Therefore, in most cases, after rest, all unpleasant symptoms are eliminated.
To restore the full function of muscles, ligaments, tendons, you will need medication and physiotherapeutic treatment followed by recovery - massages, therapeutic exercises, manual therapy.
To reduce the load on the affected limb, it is necessary to wear special devices. To prevent foot pathologies, doctors prescribe orthopedic shoes or insoles. Doctors can also prescribe anti-inflammatory drugs, muscle relaxants, and chondroprotectors. In severe cases, surgical treatment may be necessary.
Primary tumors
Primary occurrence of bone cancer is rare. Among such diseases are sarcomas. The primary lesion can be caused by active growth of bone tissue, this occurs in people under the age of twenty.
Symptoms of the primary disease:
- Pain in the focal area. At first, the pain syndrome is mild or moderate. He may disappear, but then appears again. At later stages it is constant and pronounced.
- General symptoms that are characteristic of any cancer disease, for example, weight loss, weakness, etc.
- Manifestations characteristic of bone damage - lameness, pathological fractures, etc.
Primary and secondary diseases are united by a number of manifestations, which is why in making a diagnosis you should not rely only on the patient’s complaints. Diagnostics required.
MBST therapy
With the help of magnetic radiation supplied by the MBST device, the following goals can be achieved:
- improve blood circulation and vascular condition;
- get rid of pain;
- prevent further development of the pathological process.
You can sign up for ankle treatment in Moscow at ArthroMedCenter. A completed course of MBST therapy is a good prevention of arthritis, arthrosis, atherosclerosis, and osteoporosis. After the procedure, blood circulation improves and the walls of blood vessels are strengthened. When undergoing MBST therapy, tissues begin to better absorb calcium, and damage and microcracks are restored faster.
Thanks to an integrated approach to treatment and prevention, you can get rid of unpleasant symptoms and prevent further development of diseases.
Painkillers
In almost ninety percent of cases, pain can be significantly reduced with painkillers. But often this is not enough, because as the tumor develops it can become insensitive to them. The question of choosing a drug remains relevant.
There are WHO recommendations regarding the reduction of pain caused by cancer. In these recommendations, the choice of drug should be based on the intensity of the patient's pain. This intensity is graded on a special scale.
- Points 1-3 are given to pain syndrome of mild and moderate severity. Drugs – non-opioids, for example, paracetamol;
- Points 4-6 – moderate pain syndrome. Drugs – opioids (analgesic drugs containing narcotic substances);
- Points 7-10 – the pain syndrome is severe. The drugs are strong opioids. In some cases, drugs that enhance pain relief.
Speaking about painkillers, one cannot fail to note the side effects associated with them, including:
- Feeling drowsy;
- Stool imbalance;
- Dizziness, etc.
And once again about what we noted above: it is better to start using painkillers when the pain syndrome just begins to manifest itself.
How do you know if your lower leg hurts from venous thrombosis?
Vein thrombosis (or venous thrombosis) is of two types - superficial and deep.
Thrombosis of the superficial veins is manifested by inflammation along the saphenous veins in the form of redness of the skin and a painful cord in this area. In the case of deep vein thrombosis, the disease may not reveal itself externally or may only manifest itself as swelling of the limb. Both superficial and deep venous thrombosis in the legs is a dangerous situation that requires immediate attention to a vascular surgeon.
Venous thrombosis in the legs often develops in people suffering from varicose veins, who have undergone surgery, trauma, as well as in women taking hormonal contraceptives.
Diagnostics
Based on the nature of the pain and the appearance of the affected joint, even a non-specialist can make a preliminary diagnosis (arthritis or arthrosis). But hurry to your local clinic to confirm your assumptions!
A doctor examines a patient's sore knee. Photo: chayanuphol/freepik.com
Which doctor should I contact?
If you have joint pain, you should make an appointment with your local physician. He performs the functions of a medical dispatcher: he records complaints and clinical symptoms, refers the patient for examination and, based on its results, decides which doctor should be consulted for each specific patient. A variety of specialists are involved in maintaining joint health:
- arthrologist,
- traumatologist-orthopedist,
- rheumatologist,
- vertebrologist (if the spinal joints are affected),
- podiatrist (if we are talking about foot joints),
- surgeon,
- oncologist,
- neurologist (if the joint has already been treated, but the pain remains),
- nutritionist (if your joints hurt due to metabolic disorders, such as gout, or if you are overweight).
What tests and research should I do?
The examination begins with the simplest - a clinical (finger) and biochemical (from a vein) blood test for signs of inflammation, as well as a general urine test. In some joint diseases, the kidneys are involved in the pathological process. Excess uric acid salts in the urine may indicate gout as a cause of joint disease.
Laboratory examination of the synovial fluid located inside the joint helps to detect the inflammatory process and clarify its nature. It is obtained by puncturing the joint capsule - puncture. If necessary, a histological examination of a fragment of the synovial membrane lining the joint cavity from the inside is performed.
A proven diagnostic method is radiography of the joint in two standard projections. It will help visualize narrowing of the joint space, bone spurs, osteoporosis and osteosclerosis (areas of low and high bone density, Fig. 3).
Figure 3. X-ray of the right wrist. Development of osteoporosis (b, c) during treatment with human monoclonal antibodies. Arrows indicate two-layer sclerotic stripes after two courses of the drug. Source: Elsevier Ltd/The Lancet
Currently, magnetic resonance imaging provides comprehensive information about the condition of the joint.
How to get rid of joint pain urgently?
Pills.
Photo: Bloack / Depositphotos Analgesics can quickly overcome pain: you should not tolerate pain under any circumstances if you do not want it to turn from acute to chronic. This metamorphosis can happen very quickly - in 3-4 weeks, so getting rid of joint pain should be an immediate priority. The joint starts to hurt as soon as you put stress on it. Therefore, in case of pain, half an hour before any physical activity, you should take a non-steroidal anti-inflammatory drug (NSAID) with a good analgesic effect.
If joint pain intensifies at night, in addition, before going to bed, the doctor will recommend taking metamizole sodium, as well as drotaverine with nicotinic acid to improve local blood circulation.
Local therapy
NSAIDs have a dangerous side effect - they can cause damage to the gastric mucosa, even leading to the formation of ulcers, so they try to use them topically, as part of various ointments and gels with anti-inflammatory and analgesic properties. They are usually rubbed into the skin over the affected joint twice a day. Special patches with magnetic powder, which are glued to a joint or area of the spine, also relieve pain.
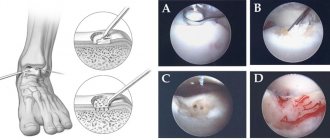
The first practices of surgical treatment of a diseased leg bone
At the beginning, the operations to treat the diseased bone were terrible. The orthopedic surgeon simply removed the protruding part of the bone. After a while, the disease appeared again, and in a more acute form, and the pain became even stronger.
The next step in treatment was the Wreden operation, which was named after the man who created it - the famous Russian surgeon R.R. Harmful. The patient experienced less pain during this operation. The method involves completely removing the inflamed metatarsal bone on the big toe. As a result, the big toe ceases to be connected to the foot and is supported only by soft tissues. Oddly enough, when everything heals, people feel relatively well, the pain goes away, and the ability to walk and lead a normal life returns. This practice still exists today. It would seem that there is no need to further develop the treatment of a diseased bone, but medicine continued to progress.
What is the treatment for a bunion? What to do if the bones on your toes hurt?
Many people have asked this question. Let's deal with him.
There are many methods to combat thumb deformation, including traditional ones:
- compresses,
- iodine nets,
- foot massage
- warm foot baths with herbal infusions and sea salt.
and others.
These remedies can help relieve pain and reduce inflammation, but they cannot cure the disease itself. The joint remains deformed, and the pain in the foot eventually returns. Only qualified orthopedic surgeons can truly cure this disease, and the radical treatment is surgery on the bone.
Preparing for bunion surgery
At the initial consultation, the doctor will explain the surgical plan to you and tell you how to prepare your leg for surgery.
If the diseased bone on the foot is not too large, and there are no changes in other toes that require intervention, the entire hospitalization will take only one day.
It is a good idea to prepare your home for the recovery period following surgery. You may want to rearrange your furniture to make it easier to walk around. It is also advisable to stock up on food so that you don’t have to go shopping, which will be uncomfortable given the pain in your finger.
Surgery to remove the bunion to relieve pain in the big toe can be performed under either local or general anesthesia. If the operation is performed under local anesthesia, after several injections at the level of the ankle joint, you will no longer feel your feet. The operation can also be performed under spinal anesthesia, in which sensitivity will be completely absent in both lower extremities, which means the patient will not feel pain.
Before any of these anesthetics, it is recommended that you do not eat for 6 hours before your planned surgery.
Your surgeon will tell you what will happen before, during, and after surgery. If there is something you don't understand, don't hesitate to ask. After you ask all the questions you are interested in and receive answers to them, you will be allowed to sign a consent to undergo surgery on your leg.