The following types of amenorrhea are distinguished:
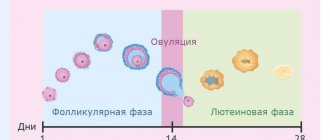
- true amenorrhea - no menstruation due to the absence of changes in the uterus and ovaries characteristic of a normal menstrual cycle. All this happens against the background of hormonal imbalance;
- false - cyclical changes in the uterus and ovaries occur, but due to abnormalities in the development of the genital organs (for example, vaginal occlusion), no bleeding is observed;
- physiological amenorrhea is a normal state of the body that is observed in teenage girls in the first two years of menstruation, as well as in women during pregnancy, lactation and menopause;
- pathological amenorrhea - can be primary (you have never had a period in your life) or secondary (you used to have periods, but for some reason they disappeared).
In addition, depending on the mechanism of development, amenorrhea can be:
- Lactational amenorrhea is one example of the physiological cessation of menstruation. Occurs with exclusive breastfeeding. The mechanism of development is similar to that of hyperprolactinemia.
- Uterine amenorrhea occurs as a complication of gynecological manipulations - curettage, cauterization, or as a consequence of childbirth. The absence of menstruation in such cases is due to the intensive growth of adhesions in the uterine cavity.
- The diagnosis of “primary amenorrhea” is given to girls who have not had a single menstruation before the age of 16, provided that the patient has secondary sexual characteristics. If a girl’s breasts do not grow, there is no pubic or armpit hair, and there has been no characteristic weight gain, a gynecologist should be consulted no later than 14 years of age.
- Secondary amenorrhea is the absence of menstruation in previously menstruating women for six months or longer. According to statistics, it accounts for up to 80% of all types of amenorrhea.
In clinical practice, secondary true amenorrhea is most common. It can occur for various reasons (for example, deficiency or excess weight, constant stress). The absence of menstruation can be a consequence of diseases of the endocrine organs, complicated abortions, tumors and the use of a number of psychotropic drugs.
Types of amenorrhea: norm and pathology
- Physiological
. Typical for women during pregnancy and breastfeeding, it is not a pathology. After cessation of lactation, the menstrual cycle returns to normal. - False
. A form of amenorrhea in which no endocrine, hormonal or gynecological disorders are observed, but menstruation is absent for 3 months or more. - Primary
. This diagnosis is given to girls if they have not started menstruating before the age of 16. - Secondary
. A pathological form of amenorrhea, which occurs due to exposure to stress, the development of endocrine and gynecological diseases. - Uterine
. A pathological form of amenorrhea resulting from destruction of the endometrium.
What is amenorrhea
Amenorrhea is a disorder of the menstrual cycle, manifested by the complete absence of menstruation in women of childbearing age for six months or more.
The absence of menstruation, not associated with pregnancy or breastfeeding, is a symptom indicating the presence of a serious gynecological pathology.
Amenorrhea is diagnosed when the patient has not had menstruation for 6 months. There are a number of physiological conditions in which amenorrhea is considered normal. These include:
- Gestation period
- Feeding time
- Time from birth to puberty of a girl (0-15 years)
- Menopause (age 45-50)
- Women of reproductive age (16-45 years) who are not pregnant or breastfeeding should have regular menstrual periods.
Amenorrhea may occur after taking low doses of oral contraceptives. In such cases, bleeding becomes scanty and sometimes disappears completely. This is due to the gradual thinning and atrophy of the endometrium under the influence of hormonal drugs. The condition is considered a normal variant.
Symptoms
Depending on the type of amenorrhea, it may be accompanied by different symptoms, but the most important and obvious one is, of course, the absence of menstruation for more than 3 cycles in a row without pregnancy.
False amenorrhea is accompanied by pain in the lower abdomen and breast swelling.
Secondary amenorrhea also manifests itself as endocrine and mental disorders - excessive growth of body hair, sudden changes in body weight, malfunction of the thyroid gland, disturbances in the functioning of the ovaries, irritability and anxiety.
Treatment
Treatment of amenorrhea comes down to correctly identifying and eliminating the cause that led to a long absence of menstruation.
Tactics depend on the patient’s age, form of amenorrhea, and the presence or absence of other diseases. General recommendations for amenorrhea:
- Eliminate psycho-emotional overload. It is necessary to avoid stressful situations or use psychological auto-training, yoga and taking sedatives to minimize their impact.
- Adjust your diet. If amenorrhea is caused by a strict diet or anorexia, it is necessary to balance the diet to quickly normalize weight. With some hormonal disorders, obesity is present, which also requires a revision of the menu.
- To refuse from bad habits.
- Avoid high physical activity. If you have menstrual irregularities, it is not recommended to engage in strenuous sports.
With secondary amenorrhea, the first step is to normalize body weight and metabolism. According to indications, such patients are prescribed hormonal correction and symptomatic therapy. Depending on the nature of the disorders, the following drugs are used:
- natural estrogens;
- progestogens;
- dopamine receptor agonists;
- analogues of gonadoliberin or gonadotropic hormones;
- sedatives and painkillers.
For anatomical disorders, surgical treatment is possible - removal of tumors or organs with a high risk of malignant degeneration, plastic reconstructive surgery.
If the cause of reproductive dysfunction is diseases of the endocrine glands, then the patient is managed together with an endocrinologist.
Author:
Baktyshev Alexey Ilyich, General Practitioner (family doctor), Ultrasound Doctor, Chief Physician
Possible causes of amenorrhea
Each type of amenorrhea has its own causes of development
:
- In the case of false amenorrhea, it is most often atresia (lack of a natural canal) of the vagina, cervix or hymen. In second place are inflammatory processes in the uterus and the consequences of medical abortions.
- Primary amenorrhea is most often caused by hereditary, psychological and anatomical reasons - underdevelopment of the gonads, occlusion of the vaginal canal and hymen, severe stress and shock.
- Secondary amenorrhea occurs in approximately 8–10% of women aged 16 to 45 years due to the development of anorexia or obesity, early menopause, increased levels of the hormone prolactin in the blood, and polycystic ovaries.
- The main reasons for the development of uterine amenorrhea are gonorrheal and tuberculous endometritis, difficult childbirth, abortion and other surgical interventions.
Diagnosis of amenorrhea
Diagnosis of amenorrhea
is carried out in several stages. First of all, the doctor interviews and examines the woman to determine the type of amenorrhea. After this, it is necessary to find out the reasons for the development of this condition. For this purpose, the doctor asks the patient in detail about the present complaints, the time of their appearance, and possible provoking factors. If a woman has previously taken treatment, she should inform the doctor about this. It is also necessary to evaluate the treatment provided - whether it was effective, how long the effect lasted, whether there were side effects, and, if so, what they were. Family history is collected separately - it is important for the gynecologist to know whether the patient’s immediate relatives had similar abnormalities.
The main laboratory tests for diagnosing amenorrhea are:
- pregnancy test - allows you to exclude physiological amenorrhea;
- karyotype study - carried out if the patient is suspected of having a genetic abnormality;
- progesterone test - used to determine the condition of the endometrium;
- blood test for hormones (LH, FSH, androgens, estradiol and prolactin) - to exclude PCOS and identify the type of amenorrhea;
- blood test for diabetes and thyroid hormones.
If there are indications, instrumental diagnostics of amenorrhea may be prescribed:
- MRI, CT – if the patient is suspected of having developmental anomalies;
- Ultrasound – to determine the condition of the endometrium and ovaries;
- hysteroscopy – to exclude intrauterine adhesions;
- X-ray of the skull (in the area of the sella turcica) – if there is a suspicion of pathologies of the pituitary gland.
Before making a diagnosis of amenorrhea, the doctor must make sure his suspicions are correct.
Diagnostics
The diagnosis is made by
a gynecologist after an examination, which includes
:
- Gynecological and vaginal examination
- Ultrasound of the pelvic organs
- MRI
- Hematological studies (clinical, biochemical blood tests, analysis for tumor markers)
- Hormonal research
- Radiography
- Treatment
In the case of amenorrhea, self-medication is completely excluded, since pathological forms of this disorder are treated with a complex of physiotherapeutic procedures and medications prescribed by a doctor.
Treatment methods used in gynecology
:
- Hormonal therapy (including the use of COCs and steroid hormones)
- Stimulation of ovulation (medical and surgical)
- Infusion therapy
- Surgical removal of adhesions and neoplasms
- Anti-adhesive drug therapy
- Antibacterial therapy in the postoperative period
- Correction of mental health in case of development of anxiety, panic and other disorders
Amenorrhea in young girls
Amenorrhea is the absence of menstruation. If you have never had menstruation in your life, this is primary amenorrhea. If you had menstruation and then disappeared (for 90 days or more), this is secondary amenorrhea; rare irregular menstruation (6-8 times a year) can be safely classified in the same category.
This problem (primary and secondary amenorrhea) is dealt with by pediatric gynecologists and gynecologist-endocrinologists.
Why did menstruation disappear?
The first thing a doctor thinks about when faced with amenorrhea is pregnancy. Even for those who categorically deny its possibility. Unfortunately, this is the same situation about which the notorious Dr. House said: “Even babies lie.” History knows a large number of home-grown “Virgin Marys” with insufficiently immaculate conception. That is why the diagnostic search starts only after pregnancy has been reliably excluded.
However, the most common cause of “lost” periods is PCOS (polycystic ovary syndrome). I detail
talked
about this disease.
Most often, constant delays in menstruation are accompanied by acne, hair growth in “male” areas and problems with excess weight. Too skinny
girls with a BMI less than 17 (weight, kg/height, m2) may also have reasonable problems with the menstrual cycle. In order for the body to begin childbearing, it needs to accumulate a certain amount of adipose tissue. If there is critically little fat, the body is able to “turn off” menstruation so as not to take risks. This is especially typical for anorexia nervosa, an eating disorder in which very thin girls consider themselves very fat and continue to lose weight.
Too much load.
Menstruation may “not turn on” or “turn off” in female athletes and ballerinas. Extremely high loads and complete mobilization of the body’s physical and mental strength can give such an effect.
Too much prolactin.
Prolactin is a hormone produced by the pituitary gland. This small gland is located almost in the center of the head, in the sella turcica, and produces many interesting and important hormones. It seems surprising now, but not long ago we were not able to determine the levels of hormones in the blood as easily as we do now. Therefore, the diagnosis of “hyperprolactinemia” was given to patients with “amenorrhea-galactorrhea”: there is no menstruation, but milk flows from the mammary glands. Nowadays there are almost no such “classic” patients, because we make the diagnosis much earlier. Hyperprolactinemia is a “good” cause of amenorrhea; this disease is successfully treated in most cases.
Too early menopause
- unfortunately, this happens. Sometimes the ovaries fail too early, plunging a woman into premature menopause. Since I wrote about this problem, little has changed. We still cannot cure these women, but we can help significantly.
Contraception is too reliable.
For some types of contraception, the absence of menstrual-like reactions is quite typical. Firstly, this applies to purely progestin contraceptives (implants, hormone-releasing IUDs or mini-pills). Combined contraceptives used in long-term regimens or with a shortened hormone-free interval may also not cause withdrawal bleeding. This is not a disease at all and not a cause for concern; menstruation is restored after stopping the drug. Most likely, the doctor was talking about how this could happen, but someone just didn’t listen well. In most cases, the absence of menstrual-like reactions is not a reason to cancel the method.
When exactly should you go to the doctor?
The problem should be taken care of if:
- The girl was 15 years old and had not yet started menstruating.
- At the age of 13, the girl has absolutely no secondary sexual characteristics (complete absence of mammary gland growth and sexual hair growth).
- Menstruation occurred regularly, and then disappeared for 90 days or more (pregnancy is reliably excluded).
- Menstruation appears rarely, with an interval of 45 days or more.
What should you pay attention to?
It is worth drawing the doctor’s attention to some circumstances that may be important when making a diagnosis:
- pregnancy is possible and cannot be reliably excluded;
- your mother or sister also had/has problems with menstruation;
- acne appears and/or hair grows on the face or chest;
- weight gain and serious problems with weight loss;
- recent weight loss;
- a feeling of “hot flashes”, like a hot wave going from the chest to the face and through the whole body;
- sweating or hot flashes at night, sleep disturbances;
- headaches or visual disturbances appeared;
- mammary glands produce “milk”;
- intense physical or emotional stress;
- change in diet (quantity and composition of products);
- taking medications, vitamins, dietary supplements or herbal infusions. For example, some antidepressants (clomipramine, amitriptyline), antipsychotics (haloperidol, thioridazine, risperidone, sulpiride, promazine, etc.), antihypertensives (reserpine, verapamil, alpha-methyldopa) or anticholinergics (physostigmine, phenytoin).
Tests and treatment
The only test you should do yourself is a pregnancy test. There is absolutely no point in donating blood for hormones on your own - most of these results will be thrown into the trash.
The doctor will build the logic of the diagnostic search in such a way as to, moving from simple to complex, establish the correct diagnosis and cut off associated causes. An ultrasound of the pelvic organs will most likely be added to the mandatory examination; an MRI of the brain may be required.
Those whose cycle disorders are associated with weight loss or, conversely, excess weight, need to enter target limits (lose weight or gain weight). Hormonal therapy without weight normalization has extremely low effectiveness.
In general, treatment of the disease will depend on the specific diagnosis and reproductive plans of the woman. If you need pregnancy, that’s one story; if you need it, but not now, it’s a completely different story.
Oksana Bogdashevskaya
Photo istockphoto.com
Consequences
Amenorrhea does not threaten a woman’s life, but can cause infertility and pathological changes in the pelvic organs, such as:
- Reduction and atrophy of the uterus
- Destruction of the endometrium with the formation of adhesions
- Complete blockage of the uterus
- Osteoporosis (increased bone fragility)
Unfortunately, if a woman does not consult a gynecologist on time, the consequences of amenorrhea can be irreversible. The listed pathologies are extremely difficult to treat, and in some cases a woman is forever deprived of the opportunity to become a mother.
Don't be afraid to see a doctor. If menstruation is absent for more than 2 months in a row, you need to make an appointment with a gynecologist and find out the reasons for this phenomenon. Only a specialist can conduct a full examination and prescribe treatment.
Gynecologists from the network of Moscow MCs “Zdorovye” are always ready to help patients with any problems related to sexual and reproductive health. We guarantee complete confidentiality, professional approach and tact of the medical staff. Make an appointment with a gynecologist on the website medcentr.biz
Treatment of amenorrhea
Treatment of amenorrhea
depends on the type of pathology and can be either conservative (weight normalization, taking various medications, etc.) or surgical (destruction of adhesions in the uterus, vaginal plastic surgery). Only after a thorough examination and identification of the causes of the disease can the doctor prescribe the necessary therapy.
For congenital anomalies, surgical intervention is the most effective. In case of hormonal imbalance, every effort must be made to normalize the functioning of the endocrine glands. For this purpose, the woman is prescribed replacement therapy or drugs that block hormone synthesis. In case of excessive weight loss, it is necessary to create an individual diet that will fully satisfy the woman’s needs for nutrients, vitamins and minerals. Benign and malignant tumors, ovarian diseases, and consequences of traumatic injuries require complex combined treatment. With intense psycho-emotional stress, psychotherapy gives good results.
Treatment of amenorrhea caused by ovarian pathology consists of prescribing combined oral contraceptives. With their help, doctors are able to restore the functioning of the reproductive system and resume regular menstruation.
Central form
Damage to the hypothalamic-pituitary region of the brain is accompanied by a characteristic appearance for patients: overweight, a rounded moon-shaped face, a fat apron, purple-red stripes on the skin of the abdomen and thighs. However, excessive thinness is also possible with weakly expressed secondary sexual characteristics. Pituitary tumors may cause progressive headaches, symptoms associated with excessive secretion of tropical hormones - acromegaly (sudden growth of the feet, hands, nose in adulthood), increased irritability and swelling. Hyperprolactinemia is manifested by discharge from the mammary glands, their pain and engorgement, and decreased libido.
Forms of amenorrhea
Depending on the degree of damage, 5 main types of pathological conditions can develop:
- Central form. This occurs due to brain damage.
- Hypothalamic form. It is characterized by damage to the hypothalamus:
- against the background of sudden weight loss;
- psychogenic nature.
- Shape of the pituitary gland. Occurs due to damage to the pituitary gland:
- hyperprolactinemia;
- hypogonadotropic amenorrhea.
- Ovarian. Occurs due to ovarian pathologies:
- ovarian wasting syndrome. It is characterized by the decline of ovarian function before the age of 38 years;
- resistant ovarian syndrome is characterized by a lack of response from the ovaries to the pituitary gland;
- virilization of neoplastic ovaries.
PCOS or polycystic ovary syndrome. With this pathology, the ovaries are covered with a dense membrane that cannot rupture on its own during ovulation. The synthesis of sex hormones is disrupted: the production of estrogen decreases and the level of androgens increases.
- Uterine form. Develops due to pathology of the uterus with intrauterine synechiae or Asherman's syndrome.
Bibliography
- Vikhlyaeva E.M. Hyperprolactinemia and reproductive system disorders. Guide to Endocrine Gynecology
- Gurkin Yu.A. Adolescent gynecology / guide for doctors
- Berek J., Adasi I., Hillard P. Gynecology according to Emil Novak
- Manusharova R.A., Cherkezova E.I. Gynecological endocrinology / guide for doctors
- Bogdanova E.A. Gynecology of children and adolescents
- Smetnik V.P. Non-operative gynecology / Smetnik V.P., Tumilovich L.G. – 3rd edition. – M.: MIA, 2003.
- Heffner L. The human reproductive system in normal and pathological conditions: A visual textbook // Trans. from English – 2003. – 128 p.
- Gordner D., Shobek D. Basic and clinical endocrinology. – M.: Publishing house. "Binom", 2010.
Possible complications
If we consider the absence of menstruation in general, then this pathology is not life-threatening. However, you should be aware that women with secondary amenorrhea are much more likely to be diagnosed with infertility or anovulation.
If you have not had your period for a long time, do not ignore this symptom, as over time it can lead to undesirable consequences:
- miscarriages in early pregnancy;
- the development of hyperplastic processes of the endometrium, which creates a threat of uterine cancer;
- diabetes mellitus;
- osteoporosis;
- reproductive system disorders;
- cardiovascular pathologies.
To find out the exact reason for the absence of menstruation, contact our clinic, where they will help you deal with the problem and give competent advice on this issue.
Possible complications of amenorrhea
- The most serious complication of any type of amenorrhea is infertility. Lack of menstruation prevents the maturation of the egg.
- A woman avoids intimacy, she experiences depression, a feeling of helplessness, irritability, and hormonal disorders. Due to uterine dysfunction, relationships between partners become strained.
- Another complication of amenorrhea can be extragenital diseases associated with a lack of estrogen, such as osteoporosis, diabetes, and heart disease.
- Lack of estrogen increases the risk of endometrial malignancy or the development of hyperplastic reactions in the uterus.
Output path anomalies
Imperforate maiden membrane
The maiden membrane (KUTEP) sometimes does not have an opening due to a disruption in the process of recanalization of the vaginal plate during the embryonic period and closes the entrance to the vagina, which blocks the exit of menstrual blood. Such patients complain of lack of menstruation and have primary. Over time, as a result of the accumulation of blood in the higher parts of the reproductive tract (cryptomenorrhea), stretching of the vagina (hematocolpos) and uterus (hematometra) occurs, which is accompanied by abdominal or pelvic pain.
Diagnostics. An objective examination reveals a bulging maiden membrane, often purplish-red in color due to hematocolpos. Treatment is surgical and consists of an arched opening of the imperforated maiden membrane.
Transverse membrane of the vagina
A transverse vaginal membrane may result from disruption of the embryonic fusion of the upper part of the vagina, which is of Müllerian origin, with the lower part, which originates from the urogenital sinus. The membrane is usually located in the upper half or middle of the vagina. Sometimes this membrane may be imperforate, causing primary (cryptomenorrhea), as in the case of imperforate maiden membrane.
Diagnostics. The diagnosis is based on a thorough objective examination of the reproductive tract. The transverse membrane of the vagina is often mistaken for an imperforate maiden membrane. With an imperforate maiden membrane, in contrast to the transverse vaginal membrane, a hymenal ring is found below the membrane.
Surgical correction involves resection of the vaginal membrane.
Vaginal agenesis, or Müllerian agenesis (Mayer-Rokitansky-Küster-Gauser syndrome)
Vaginal agenesis, or Müllerian agenesis, is a congenital Müllerian anomaly that can present as complete vaginal agenesis and absence of the uterus, or partial vaginal agenesis with the presence of a rudimentary uterus and distal part of the vagina. This disease should be distinguished from vaginal atresia, when the Müllerian system is developed, but the distal part of the vagina is replaced by connective tissue.
The diagnosis is determined by an objective examination and is confirmed by the following criteria:
- lack of a full vagina;
- presence of ovaries (visualization of the ovaries with ultrasonography);
- karyotype 46, XX.
With partial agenesis or atresia of the vagina, rectal examination may reveal mass formations in the pelvis that resemble the uterus. The uterus may also be visualized with ultrasonography, computed tomography, or magnetic resonance imaging.
Treatment . The creation of a neovagina can be achieved either by systematic expansion of the perineal body (the center of the perineum) over a long period, or by surgery (laparoscopic plastic surgery of the neovagina from the pelvic peritoneum, etc.). In true vaginal atresia, the neovagina created can be connected to the upper part of the genital tract.
Testicular feminization
Testicular feminization is a congenital insensitivity to the effects of androgens due to dysfunction or absence of testosterone receptors, which leads to the formation of a female phenotype in genetically male individuals (46, X ¥). The incidence of this syndrome is 1:50,000 women. Due to the presence of testicular tissue (testes), Müllerian inhibitory factor is secreted from early periods of development, therefore, such individuals do not have structures of Müllerian origin. The testicles may be undescended or migrate into the labia majora. Decreased or absent sensitivity to testosterone leads to a lack of pubic and axillary hair growth. Estrogen production usually occurs, leading to the development of mammary glands, but the absence of a uterus is accompanied by primary amenorrhea. Such patients often have a vagina in the form of a blind pocket.
Reconstructive surgical treatment involves creating a neovagina to allow sexual function. These patients have no reproductive function.