Connective tissue dysplasia (CTD) is a disorder of the formation of connective tissue at the moment of conception, when the genetic material of the future fetus is formed. This is a different type of combination of amino acids that affects the connective tissue of the body. Connective tissue in the body is present in all systems: cardiovascular, musculoskeletal, respiratory, urinary, visual and auditory analyzer systems, nervous system, etc. DST occurs due to a genetic disorder in which mutations occur during the formation of collagen, a building protein body. If it mutates significantly, it leads to severe organ damage and problems in their functioning.
Connective tissue dysplasia can be differentiated or undifferentiated.
The first includes:
- Ehlers-Danlos syndrome - very mobile joints, thin skin prone to damage, scar formation instead of proper wound healing, thin and fragile blood vessels;
- Marfan syndrome - occurs in patients with tall stature, long limbs and fingers, and is characterized by insufficient formation of fatty tissue, vision problems and cardiovascular disorders, as well as joint hypermobility;
- Stickler syndrome: facial asymmetry, vision and eye problems, decreased hearing and joint pathology;
- osteogenesis imperfecta syndrome: brittle, curved bones, ligament weakness, muscle atrophy and other manifestations.
Undifferentiated CTD (UCTD) is a combination of various clinical manifestations of abnormalities that go beyond the above genetically determined syndromes, which we will consider below.
How are dysplastics different?
Increased elasticity of fabrics. Everyone. Because connective tissue is everywhere. She is omnipresent! Such patients are predisposed to early postural disorders, chest deformities, and flat feet. They have hyperextension of the joints to varying degrees (hypermobility, which leads to dislocations). Their vascular walls also have increased, that is, excessive elasticity, and therefore there is a tendency to develop a disease such as varicose veins. There are also more serious complications - aneurysms, that is, thinning and bulging of the vascular walls. As a last resort, tear them apart! In my heart, when I start listening to dysplastic patients, I already know exactly what I will hear - mitral valve prolapse at a minimum and, perhaps, some other interesting findings. All this is then confirmed using ECHO-cardiography.
You can tell a lot about such patients and even without examination you can find a lot of things in them. Because the very presence of DST traits allows you to do this. Many diagnoses and features of internal organs seem to be predetermined by dysplasticity itself. We can also talk about vision. Predisposition to myopia, strabismus, astigmatism...
And of course, I would like to say a little about the characteristics of the nervous system and the psyche of dysplastic patients. As was said, these patients have a pronounced asthenic constitution: tall, thin or thin, with delicate facial features, so graceful, as we say. That is, graceful, gentle. So, what’s interesting is that most often the structure of their nervous system and psyche is also distinguished by excessive subtlety, or something.
These are rather vulnerable individuals, often emotionally labile, vulnerable, and easily exhausted. That is, we can say that among dysplastic people there are many neurasthenics, psychasthenics, and simply neurotics
And I also noticed an interesting feature in my patients: they, as a rule, have very good - even, I would say, high - cognitive abilities. These are such special and such beautiful dysplastics.
Connective tissue dysplasia in the practice of a pediatrician
Translated from Greek as “deviation in formation”
“Medical Bulletin” has touched upon the topic of DST more than once.
But so far only isolated manifestations of this congenital pathology have been described. Thus, in “MV” No. 21 for 2010, Professor L.M. Makarov spoke about primary channelopathies, often leading to sudden cardiac death in children and caused by mutations of genes expressed in the myocardium. In “MV” No. 4 for 2011, Professor I.V. Viktorova described joint hypermobility syndrome, and in No. 17-18 for 2011, Professor E.A. Gallyamov spoke about the most important pathogenetic factor of gastroesophageal reflux disease - congenital hiatal hernias, formed due to the increased elasticity of the tissues limiting this hole.
These publications already show how widespread and significant diseases caused by CTD are. However, many years of research by Z.V. Nesterenko and the world science data that she analyzes indicate that DST affects not three, but much more body systems, and this problem is incomparably wider and more acute than it was thought about in 1989, when the Scottish doctor R. Beighton first proposed to designate the congenital pathology of TS, manifested by a decrease in its strength, by the term dysplasia, which translated from Greek means “deviation in formation.”
If proline changes to arginine
The frequency of detection of CTD (according to various authors) is quite high - from 26 to 80% for all ages and from 74 to 85% among children.
In the development of such dysplasias, mutations of genes encoding the synthesis and spatial structure of collagen and responsible for the formation of matrix components are of key importance. Accordingly, according to one of the first classifications of DST, they were divided into diseases caused by impaired synthesis or catabolism of the fibrous components of DST or its main substance.
But in the 1990s, a classification that is more common today was adopted. The first group of dysplasias includes fairly rare differentiated dysplasias (DDSDs), which have a monogenic and specific type of inheritance, more often autosomal dominant, and clearly defined clinical symptoms. These are Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta and several others.
To get acquainted with DDST, let's turn to the most common (frequency of occurrence among newborns is 5:100,000) of their representative - Marfan syndrome (MS). All proven cases of this syndrome are a consequence of a mutation in the fibrillin gene. It is localized in the long arm of chromosome 15, field 21 (15ql5-q21.3). The essence of the mutation is the replacement of the amino acid proline with arginine in the fibrillin protein. As a result, the synthesis of collagen type 3 increases and the content of collagen type 1 decreases. If normally the ratio of collagen-1:collagen-3 is 6:4, then with SMA it drops to 3:7.
The clinical picture in a typical case of SMA is manifested by a characteristic triad of signs related to the musculoskeletal and cardiovascular systems, as well as the visual organs.
Changes in the musculoskeletal system include: tall stature, asthenic physique (the length of the limbs is disproportionate to the length of the body), arachnodactyly (long thin fingers), chest deformity, high arched palate, kyphoscoliosis, ligamentous weakness. Lesions of the cardiovascular system include: dilatation of the aortic root, aortic regurgitation, dissecting aortic aneurysm, mitral valve prolapse, blood regurgitation due to insufficiency of this valve. A characteristic pathology of the visual organs is iridodenesis (tremor of the lens due to weakness of the ligament of Zinn), subluxation of the lens, a high risk of retinal detachment and high myopia.
Before the widespread use of surgical correction of cardiovascular pathology, almost all patients with SMA died before the age of 30-35 years. Moreover, the main group is still in childhood. However, in the 21st century, with adequate therapy, the life expectancy of most patients with SMA is only slightly inferior to this indicator in the general population.
Tall, freckled, stooped
The second group of DST, which makes up the disorders most often encountered by practical pediatricians, includes disorders united by the term undifferentiated dysplasia (UDTD). Unlike differentiated dysplasias, UCTD are genetically heterogeneous pathologies. The main characteristic of such dysplasias is a wide range of clinical manifestations without clear symptoms. That is, UCTD is not a nosological entity, and there is no place for it in ICD-10 yet. In turn, UCTDs are divided into 2 groups: diseases with an established and unidentified (and this is the vast majority of UCTDs) gene defect.
UCTD in a child can be diagnosed already at the stage of physical examination with a comprehensive assessment of the so-called phenotypic markers. External and visceral markers are distinguished, the predominance of which depends on what type of TS lesion occurs - dense or loose. The critical number of external markers that allows one to make a conclusion about the presence of UCTD is now considered to be 3-6. Based on the diagnostic significance of individual signs of UCTD, diagnostic tables are proposed with a score of external and visceral markers, as well as biochemical parameters.
For example, external changes in the skin in children with UCTD usually indicate damage to loose connective tissue and are characterized by the presence of hyperelasticity, increased extensibility, stretch marks, keloid scars, a pronounced subcutaneous venous network, characteristic pigment spots of the “café au lait” color, or depigmentation, a large number nevi.
But lesions of dense TS are manifested by changes in the skeleton: poor posture in the form of kyphosis and scoliosis, stooping, chest deformities, and flat feet. Such children, as a rule, are tall and asthenic in build.
All children with UCTD exhibit so-called minor developmental anomalies, or dysmorphia. The most common dysmorphias include: fair skin, fused eyebrows, wide bridge of the nose, hyper- and hypotelorism, blue sclera, epicanthus, abnormal tooth growth, deformed auricle, fused lobe, curved little fingers, incomplete syndactyly of the fingers, light or red hair color. Diagnostically significant for identifying UCTD is the presence of 6 or more dysmorphias in a child.
Markers external and internal
Let us now turn to the internal markers of UCTD, and we emphasize that there is a direct correlation between the number of external and internal markers.
If we talk about the integral indicators of internal UCTD markers detected by biochemical methods, then the most informative is determining the level of molecules formed during the breakdown of collagen. These are hydroxyproline and glycosaminoglycans in daily urine, and in blood serum - lysine and proline. A change in the ratio of collagens of different types in UCTD allows the use of the indirect immunofluorescence method according to Sternberg LA (1982) in diagnosis.
On the membranes of leukocytes, an increased representation of HLA histocompatibility antigens is usually detected - A28, B35, Cw5, Cw52, and on the other hand, a reduced number of antigens such as A2, B12, Cw3. The most promising, of course, are molecular genetic diagnostic methods that identify specific gene mutations. However, in cases of UCTD, these assays are still at an early stage of development.
One of the most often involved in the pathological process in UCTD in children is the cardiorespiratory system.
This leads to serious pediatric errors
With UCTD in children, the formation of the elastic framework of the lungs is disrupted at the beginning of life, which causes the valve mechanism of bronchial obstruction and the formation of emphysematous bullae due to rupture of morphologically incompetent interalveolar septa. The consequence of subpleurally located bullae can be spontaneous pneumothorax. A congenital defect in the cartilaginous and connective tissue framework of the trachea and bronchi leads to their increased mobility, the occurrence of bronchiectasis, and pneumosclerosis. Dyskinesia of the trachea and bronchi leads to the development of broncho-obstructive syndrome (BOS).
There is a high correlation between the severity of bronchial asthma in children and the manifestations of dysplasia. And the more common and severe the latter are, the earlier the child develops pulmonary hypertension and pulmonary fibrosis in addition to bronchial asthma.
Anomalies in the structure of the bronchopulmonary system in UCTD lead to a deterioration in the elimination of pathogenic agents in conditions of altered immune reactivity and contribute to the long-term persistence of bacteria and the formation of a recurrent course of pneumonia. It is also noteworthy that the level of atypical childhood pneumonia is growing, caused by intracellular pathogens - chlamydia and mycoplasma, with a predominant lesion of the interstitium of the lungs, with a recurrent course of which progresses, as in cases of asthma, pneumofibrosis, pulmonary hypertension.
With UCTD, congenital defects are often diagnosed: tracheobronchomegaly, tracheobronchomalacia, cystic hypoplasia of the lungs. Against the background of dysplasia, the listed diseases are especially often accompanied by the development of severe complications in the form of pneumofibrosis, pulmonary hypertension, bronchiectasis, and spontaneous pneumothorax.
Unfortunately, in contrast to the above-mentioned pronounced manifestations of UCTD in children, subclinical variants are usually not diagnosed. This often leads to incorrect interpretation of the pathological process and serious pediatric errors.
Truly small heart
Since 1987, the classification of diseases of the cardiovascular system of the New York Heart Association has identified the syndrome of connective tissue dysplasia of the heart (CDS), which accompanies both differentiated and undifferentiated dysplasia. In turn, cardiac dysplasia includes several syndromes.
Valvular syndrome combines isolated and combined heart valve prolapses and myxomatous valve degeneration. In approximately 70% of cases, the syndrome is represented by prolapse of the mitral valve, less often - tricuspid or aortic, enlargement of the aortic root and pulmonary trunk; ectopically located chordae, aneurysms of the sinuses of Valsalva. In some cases, such changes are accompanied by regurgitation phenomena, which is reflected in the indicators of myocardial contractility and volumetric parameters of the heart.
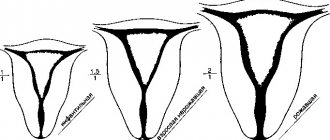
With thoradiaphragmatic syndrome, we are talking about the asthenic shape of the chest or its deformation, spinal deformities (scoliosis, kyphoscoliosis, hyperkyphosis, hyperlordosis), changes in standing and excursion of the diaphragm. Among children with CTD, the most common deformity of the chest is pectus excavatum, and the second most common is keeled. Deformations of the sternum, ribs, spine and the associated high position of the diaphragm reduce the chest cavity, increase intrathoracic pressure, disrupt the inflow and outflow of blood, and contribute to the occurrence of arrhythmias.
Vascular syndrome involves damage to elastic arteries, in which their walls expand and saccular aneurysms appear. Arteries of both muscular and mixed types are affected. As a result, bifurcation-hemodynamic aneurysms appear, as well as pathological tortuosity of vessels up to looping.
Thoradiaphragmatic heart syndrome (THDS) is formed in parallel with the progression of deformation of the chest and spine, against the background of valvular and vascular syndromes. In children with a typical asthenic constitution, the asthenic variant of STDS is more often manifested. In this case, the size of the heart chambers decreases, but while maintaining their normal thickness. In a word, a “true small heart” is being formed, functioning without serious deviations.
Unfortunately, in some children with chest deformation due to displacement of the heart, when it “moves away” from the mechanical influences of the chest bone, rotating and accompanied by “torsion” of the main vascular trunks, the so-called false stenotic variant of TDS is formed, which is especially severe.
Metabolic cardiomyopathy syndrome combines cardialgia, arrhythmias, and disorders of repolarization processes. The development of metabolic cardiomyopathy is determined by the influence of cardiac factors (valvular syndrome, variants of CVD) and extracardiac conditions (autonomic dysfunction, deficiency of micro- and macroelements, etc.). Cardiomyopathies with DST usually do not have specific symptoms.
Arrhythmic syndrome includes ventricular and atrial extrasystoles, paroxysmal tachyarrhythmias, pacemaker migrations, atrioventricular and intraventricular blocks, anomalies of impulse conduction along additional pathways, ventricular preexcitation syndrome, and QT interval prolongation syndrome.
A practical pediatrician should remember that in children suffering from CTD, cardiomyopathies and arrhythmic syndrome are very common (in 60-64% of patients). And it is they who determine the increased risk of sudden cardiac death in such children.
A universal remedy has not yet been found
A universal remedy that restores connective tissue for all forms of dysplasia has not yet been found. An individual treatment program is selected for each child with CTD. Its three main tasks are: improving the metabolic processes of connective tissue, eliminating existing complications and preventing new ones.
In any case, we are talking about the actually coordinated work of a team of pediatricians of several specialties. And about a very complex, complex treatment that affects the entire childhood period of life (in the Russian Federation - up to 18 years). We will have time to give only one example of such therapy, related to Marfan syndrome.
Non-drug therapy includes strict adherence to the child’s diet, including nutrition, where the emphasis is on the consumption of complete proteins and foods containing polyunsaturated fatty acids; and physical activity, certain types of which are prohibited for such patients. There is a list of professions for which schoolchildren suffering from CTD cannot be trained.
Drug treatment includes symptomatic administration of b-blockers. In the case of aortic dilatation, and especially in the presence of regurgitation, they reduce the ejection into the aorta and, accordingly, the load on its walls, correcting concomitant hypertension. It is believed that these cardiotropic drugs reduce the risk of sudden death in children with cardiac damage due to SMA and any other CTD.
Since it has been proven that the progression of skeletal pathologies in Marfan syndrome slows down when the deficiency of microelements (calcium, magnesium, zinc, copper) necessary for the formation of TS is eliminated, nutritional supplements containing the above substances, as well as hyaluronic acid, synthetic analogues of vitamins K and D3. In the blood of patients with SMA, there is often an increased level of somatotropic hormone. Therefore, to reduce its secretion, high-fat Omega-3 enzymes are prescribed in the diet from early childhood.
Let us now turn to therapy affecting connective tissue. It includes ascorbic acid in the form of special children's milkshakes, as well as correctors for impaired synthesis and catabolism of glycosaminoglycans - chondroitin sulfate and succinic acid. Another drug recommended as a corrector of bioenergetic processes is carnitine chloride.
What surgeons can do
For aortic aneurysm, dissecting aneurysm, aortic valve defect with symptoms of heart failure, and children with Marfan syndrome, only surgical treatment can help. Clear indications for prosthetics have been developed. For example, an aneurysmally dilated aorta must be replaced with an endo- or exoprosthesis. In case of mitral valve prolapse accompanied by “stable” regurgitation, valve replacement is not performed. However, with the rapid progression of regurgitation, up to the addition of left ventricular failure, valve replacement becomes necessary.
Surgical treatment of deformities of the chest and spine is an extremely traumatic procedure, carried out in several stages, often complicated by pleurisy, pericarditis, and pneumonia. The question of its feasibility was discussed many times at symposiums dedicated to DST. Specialists from various countries adopted a common position denying the advisability of such operations for any DST.
How to live with dysplasia
When people ask me whether it is possible to play sports with signs of DST, I say this: if there are no serious contraindications, it is possible, but excluding high-achievement sports, that is, professional sports. It is not for dysplastic patients! Or rather, they are not for him.
And it is also necessary, if not completely eliminated, then to limit static loads, heavy lifting, frantic pumping of muscles (this type of load provokes the appearance of hernias)
Sports for dysplastic patients must be chosen for one and only purpose - health improvement! It is necessary to create a muscle corset and improve overall health.
Why is it so important to know whether there are signs of dysplasia or not and how pronounced they are (at the level of features or pathology)? But because many of the problems listed above can be avoided. For example, by creating a muscle corset through physical therapy, massage and swimming, you can avoid curvature of the spine or deformation of the chest. Or get rid of the suffering that flat feet brings (foot deformity, arthrosis-arthritis, pain, etc.) by strengthening the muscles of the arch of the foot in advance, buying custom insoles and good shoes. Knowing about your predisposition to visual impairment, follow certain rules, do the necessary eye exercises, and visit an ophthalmologist regularly.
As a rule, dysplastic patients from childhood need observation by an orthopedist, cardiologist, ophthalmologist (the list can be continued, it all depends on what is detected and requires observation). And then everything will be great for them. They will be practically healthy, well educated, successful in their careers. They just need the conditions for this.