Joints are parts of the body that undergo an incalculable number of movements every day. In this regard, they are susceptible to numerous destructions and various types of inflammatory processes, which have a common name - arthritis.
Arthritis is a generalized, collective name for various types of inflammation localized in the joints. The current clinical picture suggests that arthritis can be either a separate disease or act as a complication.
Types of Arthritis
Arthritis is a disease that is characteristic of people predominantly of old age, however, the clinical picture also occurs in a category of people at an earlier age, in particular, in children and adolescents.
The varying incidence statistics at different ages are explained by the probable causes of the development of joint arthritis, according to which it is customary to distinguish several types of arthritis:
Rheumatoid
It occurs in conditions of frequent failure of the immune system, and therefore belongs to the category of autoimmune diseases. It manifests itself as chronic inflammation of the connective tissues of the body.
Symptoms include:
- symmetrical joint damage;
- the appearance of “nodules” at the folds.
Among the main factors contributing to the occurrence of the disease are:
- heredity;
- past viral diseases;
- allergic reactions;
- other types of arthritis;
- being under constant stress;
- hormonal imbalances.
Reactive arthritis
One of the heaviest varieties. During the development of regenerative processes, inflammation occurs not only inside the joint, but also in the tissues of the digestive system. In addition, it is worth noting that pelvic inflammation can also occur in reactive arthritis.
There are two subtypes of reactive arthritis:
- postenterocolitic (develops as a complication of intestinal infections caused by pathogens of various kinds, in particular Salmonella, Yersinia, Campylobacter, etc.);
- urogenital (develops after suffering infections such as chlamydia, ureplasmosis, etc.).
The main symptoms may be accompanied by additional:
- inflammation of the urinary tract;
- the appearance of cystitis, urethritis;
- tearfulness;
- conjunctivitis.
Infectious arthritis
Inflammation has a bacterial, viral or fungal etiology. It is diagnosed in patients of all ages: from newborns to the elderly.
Infectious arthritis can be:
- bacterial;
- viral;
- fungal-viral;
- parasitic-viral.
In addition to the classic symptoms, you may experience:
- intoxication;
- chills;
- fever;
- elevated body temperature.
The risk group includes people with rheumatoid arthritis, osteoarthritis, as well as those with addictions, diabetes, obesity, etc.
Gouty arthritis
An inflammatory process that occurs due to the accumulation of uric acid in tissues, which destroys the structure of cartilaginous and periarticular tissues.
There are two types:
- primary – is hereditary in nature and makes itself felt in the presence of unfavorable factors;
- secondary – hyperuricemia (increased levels of uric acid in the blood), resulting from a number of diseases or the use of medications.
Symptoms include:
- swelling and swelling of the joints of the limbs;
- redness of areas of inflammation;
- cramping pain syndrome.
Psoriatic arthritis
Inflammatory processes occurring inside the joint provoke a skin disease such as psoriasis.
The etiology of the disease is unclear. The treatment process is one of the most difficult.
Typical symptoms include:
- asymmetrical increase in the size of small joints of the limbs;
- change in skin color;
- lack of mobility of varying degrees;
- the need to take anesthetics.
Factors that increase the risk of developing the disease:
- frequent occurrence of stressful situations;
- abuse of bad habits;
- infectious diseases.
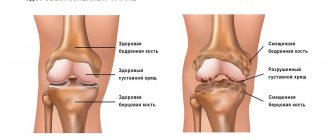
Osteoarthritis
An inflammatory process that affects the cartilage tissue and bones that form the joint. In the process of destruction of cartilage tissue and the body's attempts to restore it, excessive growth of bone tissue occurs, which often leads to direct destruction of the joint.
Symptoms appear slowly, gradually, as the disease develops.
This type of disease often occurs in older people (over 60 years old). Among the factors that increase the risk of disease, it is customary to highlight:
- natural aging of the body;
- excess body weight;
- musculoskeletal injuries;
- hereditary predisposition.
Traumatic (Post-traumatic)
It occurs as a result of previous injuries, not only to the joint itself, but also to injuries/bruises of the periarticular tissues.
The risk group includes people associated with traumatic, physically demanding professional activities, in particular athletes.
Often the disease affects mainly large joints: shoulder, elbow, knee, ankle.
The main symptom is the appearance of crunching in the joints.
The main causes of traumatic arthritis are single and repeated injuries.
Types of arthritic inflammation
This inflammatory disease has two degrees of involvement, according to which it can be systematized: monoarthritis (develops in one joint) and polyarthritis (affects several joints at the same time). According to the rheumatological classification, arthritis is divided into types, some of which can only be determined through tests. Therefore, if you have regular joint pain, do not self-medicate. We recommend contacting the Innovative Medical Center, where experienced specialists, after examination, will give you an accurate diagnosis and prescribe the necessary treatment.
There are these types of arthritis:
- reactive;
- rheumatoid;
- infectious;
- gouty;
- psoriatic;
- osteoarthritis;
- traumatic.
- Knee-joint
- Elbow joint
- Shoulder joint
- Finger joints
- Joints of the hands
Arthritis stages
The dynamics of the pathological process suggests the identification of four stages of arthritis:
Stage 1 – the disease practically does not manifest itself, but x-rays of the joints show primary signs of arthritis.
It is characterized by slight stiffness of movement and a feeling of pain when performing various types of loads.
Stage 2 – the progress of inflammation causes the destruction of articular tissues and the formation of erosions on the heads of bones.
The inflamed joint experiences swelling and increased temperature.
Stage 3 – the structure of the joint tissue continues to deteriorate, a visually noticeable deformation of the joints appears, which causes limited mobility and the appearance of pain that accompanies every movement.
There is a partial loss of the functionality of the joint, which is often compensated by tension in the muscle frame.
Stage 4 – the changes that have occurred are irreversible, the inflamed joint loses its ability to move.
If the disease is localized in the knee joints, contractures (tightening, narrowing) are formed at the final stage, and in the hip joints, ankylosis (fusion of the bones of the joint) is formed.
Diagnostics
Have you noticed the presence of several symptoms, but don’t know which doctor treats arthritis? Feel free to seek help from specialists such as a rheumatologist, traumatologist, or therapist (including a chiropractor).
In order to diagnose arthritis of various types, an integrated approach is used, which involves primary and secondary examination of the patient. Modern medicine distinguishes two main methods:
- laboratory (blood and/or immune system testing);
- instrumental (x-ray/ultrasound examination, computed tomography/magnetic resonance imaging, arthroscopy, myelography).
Treatment of joint arthritis
Only a specialist can determine how to treat arthritis.
The key condition for competent treatment of arthritis of any type is complexity and optimal duration.
Treatment of joint arthritis is prescribed taking into account the diagnostic results, in accordance with current medical standards, in accordance with the scheme developed by a specialist. A number of therapeutic measures are determined by the causes of the disease, its type and characteristics of its course. At the same time, the doctor also takes into account the likelihood of various complications and existing contraindications.
The entire treatment process consists of two stages:
- eliminating the causes of the disease;
- impact on the mechanisms of disease development.
Traditional complex treatment of arthritis involves:
- use of medications of various effects;
- prescription of vitamins;
- use of ointments/gels;
- carrying out physiotherapeutic treatment;
- possibility of surgical intervention;
- organization of therapeutic exercises;
- dieting.
The use of a set of measures ensures effective work aimed at achieving a single goal - curing the patient.
Let's look at the types of treatment in more detail.
Medication
Treatment of joint arthritis with medications is aimed at relieving pain and restoring a normal lifestyle, which includes proper rest, quality work and daily activities without outside help.
To treat arthritis, anti-inflammatory and painkillers are used, as well as chondroprotectors, the key task of which is to restore cartilage tissue.
To eliminate severe inflammation and abscess (formation of a purulent cavity), antibiotics of various spectrums of action can be used.
Physiotherapeutic
Accompanies the phase of reduction of acute inflammatory processes. Using the influence of physical factors makes it possible to significantly accelerate the healing process and achieve stable remission of the disease.
Physiotherapeutic treatment includes:
- laser therapy – promotes activation of local microcirculation and increases local immunity;
- ultra-high frequency therapy (UHF) – promotes the dilation of blood vessels and increases the flow of immune cells to the site of inflammation;
- ultraviolet irradiation – has a bactericidal effect, which increases resistance to viruses and bacteria;
- phonophoresis - involves rubbing hydrocortisone ointment and subsequent exposure to a radiator, which enhances its anti-inflammatory effect and activates blood flow, thereby improving metabolic processes inside the joint;
- Magnetic therapy – normalizes blood circulation and metabolic processes, improving the absorption of medications for arthritis and eliminating inflammation, swelling and pain syndromes, which promotes active recovery.
Diet for arthritis
A balanced diet is the key to successful treatment of any disease. It is for this reason that diet for arthritis is an important condition, the observance of which significantly increases the effectiveness of drug treatment and serves as an excellent prevention of arthritis.
Today, it is customary for experts to highlight a number of general recommendations regarding nutrition for arthritis of the joints:
- Complete cessation of bad habits (smoking/alcohol).
- Balanced, varied diet.
- Reduced calorie content in the menu.
- Increasing the proportion of foods fortified with vitamins (beans, fruits/vegetables, lean meat/fish).
- Compliance with portion sizes, as well as diet (at least 5 times a day).
- Compliance with the drinking regime (1.5-2 liters of water per day).
Proper nutrition for arthritis helps to significantly reduce ongoing inflammatory processes. Following a therapeutic diet for arthritis will improve metabolism and help reduce the amount of uric acid in the body.
Exercise therapy
Therapeutic physical education (PT) is an important component of the complex treatment of arthritis. The systematic use of a set of exercises for arthritis is used to preserve the self-care function and ensure maximum efficiency in restoring joint function during the acute period of the disease.
Among the basic principles of gymnastics for joints, it is worth highlighting:
- tracking blood pressure and pulse levels, pain levels, and the degree of joint swelling;
- smoothness of movements, in conditions of small amplitude of joint movement;
- gradual increase in load;
- regularity of classes;
- MANDATORY consultation with a specialist (coordination of the exercises used).
A well-developed set of therapeutic gymnastics exercises can help achieve stable remission, significantly reduce pain and relieve pathological tension in the muscle frame.
Frequently asked questions about the disease
Arthritis and arthrosis, what is the difference?
Arthritis is inflammation of the joint, and arthrosis is the result of metabolic disorders.
Is it possible to do massage with arthritis?
As prescribed by a doctor and only at the rehabilitation stage or during remission.
Do they take into the army with arthritis?
It all depends on the condition of the joint. People with bone deformities, as well as in the presence of an acute inflammatory process, are not accepted into the army.
Is it possible to heat joints if you have arthritis?
This can only be decided by the attending physician, since it all depends on the form and type of arthritis. You definitely shouldn’t use heat during a purulent process or after an injury.
Joint inflammation is a serious disease. Without timely medical care, it can lead to disability. Therefore, at the first signs of arthritis, you should consult a doctor. The specialists of the Paramita clinic in Moscow will help you in any case, even if you have suffered from joint pain for years. Come and see for yourself!
Literature:
- Nasonov E.L. Pharmacotherapy of rheumatoid arthritis from the perspective of evidence-based medicine: new recommendations // RMJ. 2002. T. 10. No. 6. pp. 294–302.
- Korpela M., Laasonen L., Hannonen P. et al. Retardation of joint damage in patients with early rheumatoid arthritis by initial aggressive treatment with disease–modifying antirheumatic drugs: five–year experience from the FIN–RACo study // Arthritis Rheum. Vol. 50. R. 2072–2081.
- Smolen JS, Aletaha D., Machold KP Therapeutic strategies in early rheumatoid arthritis. Best Pract. Res//Clin. Rheumatol. 2005. Vol. 19. R. 163–177.
Themes
Arthritis, Joints, Pain, Treatment without surgery Date of publication: 09/30/2020 Date of update: 04/03/2021
Reader rating
Rating: 5 / 5 (1)
Medicines for arthritis
Treatment of joint arthritis with medications is carried out using drugs of various effects, among which non-steroidal anti-inflammatory drugs (NSAIDs), for example, Artradol, Ibuprofen and Diclofenac, occupy a special place.
If NSAIDs are insufficiently effective, the attending physician may prescribe treatment with hormonal steroids (Prednisolone, Hydrocortisone). It is worth noting that steroid-type drugs can be used both in the form of tablets for arthritis and used as injections and used primarily to relieve inflammation, swelling and pain.
In order to stop the process of cell division, cytostatics (Methotrexate, Immard) can be prescribed, and in parallel with them, antibiotics (Sulfasalazine, Doxycycline, etc.) can be prescribed to destroy pathogenic microorganisms and relieve inflammation.
One of the recommended treatment methods is the use of chondroprotectors, which contain chondrotin and glucosamine, which ensures high-quality restoration of hyaline cartilage (Artracam, Chondra Evalar).
Vitamin therapy involves taking vitamins of groups B (anti-inflammatory and regenerative effect), E (antioxidants) and C (immunity enhancement). Used in parallel with a course of tablets for arthritis.
As additional methods of drug treatment, it is permissible to use local remedies - ointments/gels for arthritis. They may have anti-inflammatory and analgesic effects. Voltaren, Fastum-gel and Capsicam are considered to be the most effective.
To relieve spasms and pain, muscle relaxant drugs are used that normalize muscle tone (Sirdalud, Mydocalm).
It is important to note that taking painkillers for arthritis without consulting a doctor should not exceed 3 days, as this may lead to missing the moment of development of serious complications.
Folk remedies
Before using traditional methods for arthritis, be sure to consult with your doctor.
- Birch leaves (2.5 teaspoons), stinging nettle leaves (2.5 teaspoons), tricolor violet grass (2.5 teaspoons). Take the infusion 1/2 cup 4 times a day before meals.
- Lubricate the knee with honey, apply mustard plaster and tie it. Hold until a burning sensation appears, then remove the mustard plaster, and wrap the knee with honey, as with a compress, and keep it overnight.
- Mash the ranunculus flowers and apply to the knee for 2 hours, then remove and wrap the sore spot overnight.
- Grate the radish or horseradish on a fine grater. Apply the paste or the juice itself to the painful area. Leave for 40 minutes. The course for arthritis is 10 procedures every other day.
- If salts are deposited in the joint, cut the onion head in half. Pour one drop of tar into the middle of each half and apply to the sore spot.
- Beat the yolk with apple cider vinegar. Apply the application until dry. Use several times a week for a month.
- Garden purslane for arthritis. Grind the grass. Mix with cold water, in a ratio of one spoon per glass of liquid. Place on the fire and boil for ten minutes. Cover the container with a towel and place in a warm place for two hours. Then strain. Take the finished infusion three times a day, one tablespoon.
Complications and possible consequences of arthritis
The likelihood of early complications of arthritis in the form of panarthritis (acute purulent arthritis), phlegmon (diffused purulent inflammation) and other processes is possible mainly with an infectious form of the disease.
Late complications usually include:
- contractures;
- pathological dislocations;
- osteomyelitis (purulent-necrotic process of bone or bone marrow);
- generalized sepsis (inflammation).
Lack of proper treatment for progressive arthritis can lead to loss of self-care and free movement - disability.
Prevention
The best treatment for any type of arthritis is prevention. Preventive measures are primarily necessary for people who are at risk for one of the reasons:
- heredity;
- reduced immunity;
- excess body weight;
- Professional activities involve heavy loads on the joints.
There are two current types of arthritis prevention:
- primary prevention is aimed at preventing the onset and development of the disease, as well as preventing the reasons why it may occur. Involves: timely diagnosis and treatment of various viral and colds;
- quality treatment of chronic infectious diseases;
- the use of measures to strengthen the body's immunity;
- maintaining a healthy lifestyle.
- the use of a course of drug treatment with drugs prescribed by the attending physician;
Timely contact with a professional specialist allows you to promptly identify the disease, determine its degree of development and prescribe the most appropriate treatment.
Self-medication can aggravate inflammatory processes and lead to irreversible consequences, including disability.
General clinical recommendations
To prevent the development of arthritis and their relapses, the following recommendations should be followed:
- monitor your weight, avoid heavy physical activity;
- lead an active lifestyle, do gymnastics, swimming, yoga, etc.;
- break bad habits;
- always get enough sleep, avoid prolonged stress;
- timely treat under the supervision of a doctor all diseases, colds, chronic foci of infection;
- for chronic arthritis, regularly undergo courses of anti-relapse treatment.
A nutritious, varied diet is of great importance for joint health. But it is recommended to exclude from the diet foods that can cause an exacerbation of the pathological process, these are: onions, garlic, meat, fish, mushroom concentrated broths, fatty, fried, smoked foods, alcohol, sweets, baked goods.