The human body consists of many cells. They all have different structures and perform different functions. But there is something that unites all their diversity - this is a constant process of renewal. It can be considered using the example of bone structures. Osteoclast and osteoblast cells are like asphalt-laying crews: some remove old asphalt, others lay new ones. Bone tissue is continuously renewed, and the brain controls this work.
When a failure occurs, there is always a reason: either the brain gave the wrong command, or there was not enough building material, or osteoblasts (cells that build tissue) have decreased in number. And osteoclasts (destroyers) remained in the same number. This leads to various diseases, in particular osteoporosis.
Bone. Functions of bone tissue. The structure of bone tissue
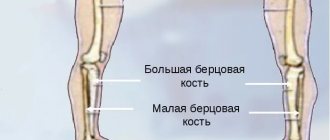
The skeleton of any adult human includes 206 different bones, all of them different in structure and role. At first glance, they appear hard, inflexible and lifeless. But this is a mistaken impression; various metabolic processes, destruction and regeneration continuously occur in them. They, together with muscles and ligaments, form a special system called “musculoskeletal tissue,” the main function of which is musculoskeletal. It is formed from several types of special cells that differ in structure, functional features and significance. Bone cells, their structure and functions will be discussed further.
What are osteoclasts?
Current version of the page so far
experienced participants and may differ significantly from
, accessed October 20, 2017; requires verification
Current version of the page so far
experienced participants and may differ significantly from
, accessed October 20, 2017; requires verification
Osteoclasts and osteoblasts on the trabecula of the lower jaw of a cow embryo
Osteoclasts
- giant multinucleated cells of vertebrate animals that remove bone tissue by dissolving the mineral component and destroying collagen. The diameter of the osteoclast is about 40 microns, they contain 15-20 closely spaced nuclei. In combination with osteoblasts, osteoclasts control the amount of bone tissue (osteoblasts create new bone tissue, and osteoclasts destroy old bone).
An osteoclast is a bone macrophage (in other words, a monocyte differentiated within bone tissue). It usually has many lysosomes. When hydrolytic enzymes contained in lysosomes are released, resorption of the basic substance of bone and calcified cartilage occurs.
The human body consists of many cells. They all have different structures and perform different functions. But there is something that unites all their diversity - this is a constant process of renewal. It can be considered using the example of bone structures. Osteoclast and osteoblast cells are like asphalt-laying crews: some remove old asphalt, others lay new ones. Bone tissue is continuously renewed, and the brain controls this work.
When a failure occurs, there is always a reason: either the brain gave the wrong command, or there was not enough building material, or osteoblasts (cells that build tissue) have decreased in number. And osteoclasts (destroyers) remained in the same number. This leads to various diseases, in particular osteoporosis.
Bone is an organ of the body that is constantly renewed. It consists of several types of tissues, the most important of which is bone. In the developed intercellular substance of bone, rich in salts, three types of cells work:
To describe them briefly, they are guardians, creators and destroyers.
The name of these cells comes from the ancient Greek words “bone” and “sprout”. These are young cells that form bone tissue. First they create a matrix, a network of intercellular substance. After this stage, osteoblasts calcify the matrix, while themselves turning into osteocytes.
Osteoblasts have a cubic or pyramidal shape. They have a developed granular endoplasmic reticulum that synthesizes proteins. The Golgi complex brings them into the developing bone. Mitochondria ensure the normal functioning of the cell, providing it with energy. Osteoblasts can divide by mitosis.
The main task of osteoblasts is the formation of matrix proteins, which include collagen, osteocalcin and osteopontin. After their synthesis, the deposition of mineral substances in the matrix begins. They also secrete ossein, which glues calcium salts together. As a result, the bone becomes a mineral-organic structure.
Osteoblasts help transport calcium and phosphate, which helps in alkalizing the body. During bone formation, they are found on the entire surface of bone beams, and after that - in places of destruction and regeneration after injury, as well as in the periosteum.
An osteocyte is called a cell of mature bone tissue. This is a definitive cell, that is, one that has arrived at its final form. It does not have the ability to divide through mitosis. When the matrix structure is completely filled with mineral matter, the osteoblast stops working and the cell becomes an osteocyte. The function of osteocytes is to ensure the maintenance and regeneration of bones, as well as the regulation of mineral composition.
There are gaps in the bone structure in which osteocytes are located. During the process of embedding, osteoblasts create long processes of osteocytes that touch each other with nexuses. The processes located near the vessel receive nutrition and oxygen from it. The number of such processes can be very large, up to several hundred. The osteocyte has a star shape due to the many processes that are located in the bone tubules. After aging and apoptosis (self-destruction), the tubules become empty.
Osteoclasts are giant (40 µm in diameter) multinucleated cells. They destroy bone by dissolving mineral salts and destroying the collagen matrix. They have several nuclei (from 5 to 20), many Golgi complexes, mitochondria and lysosomes. Lysosomes release enzymes that initiate bone resorption.
In other words, an osteoclast is a bone macrophage. It approaches the bone, attaches to it with a corrugated border and forms a membrane that protects the environment of the osteoclast from the action of hormones. It then produces an acidic environment that dissolves the mineral salts. Afterwards, with the help of lysosome enzymes, the old cells are digested. Some of the substances go into the blood, the rest is used to support the process of bone destruction.
Osteoclasts work as a group. They eat into the old bone and create a tunnel in it. The daily passage of such a group is 50 microns. After the passage of the first group, the second, consisting of osteoblasts, begins to move. They are located along the walls of the tunnel and fill their surface. After this, they begin to synthesize the matrix at a rate of 1 micron per day. At the same time, capillaries begin to grow along the axis of the tunnel.
Having built the matrix, osteoblasts begin to wall themselves up, creating a mineral-protein structure around themselves. Upon reaching the goal, when the bone is already built, osteocytes remain in the gaps. They live for some time, after which they end their lives by self-destruction (apoptosis).
The process of two types of bone cells working in tandem is called remodeling. It is regulated by hormones of the parathyroid glands, which activate osteoclasts. This is parathyroid hormone. The thyroid gland produces calcitonin, which stimulates bone formation. In addition to these, many other hormones that are produced by the gonads, pituitary gland and pancreas are involved in remodeling.
If hormones are disrupted, a lack of osteoblasts or their inhibition may occur. Together with osteoclast activity, this can lead to disease. For example, osteoporosis and its consequences: fractures and joint damage.
Life requires the proper functioning of all parts of the body, even such small structures as osteoclasts. This allows all the organs of the human body, from the thyroid gland to the bones, to communicate with each other. That is why knowledge about a healthy lifestyle, proper nutrition and staying healthy is needed. Then premature osteoporosis will not be scary.
OSTEOCLASTS - (from osteo... and Greek klao I break, break), bone crushers, usually multinucleated large cells that destroy (resorb) bone tissue and calcified cartilage with the help of hydrolytic substances released from them. enzymes concentrated in... ... Biological encyclopedic dictionary
osteoclasts - (osteo... gr. klao I destroy) multinuclear formations that arise during the development and restructuring of bone tissue; take part in the resorption of the basic substance of bone. New dictionary of foreign words. by EdwART, 2009. osteoclasts (te), ov, units... ... Dictionary of foreign words of the Russian language
Osteoclasts - (from osteo... (See Octeo...) and Greek, kláō I break, break) cells that destroy bone tissue during its restructuring in vertebrates and humans. They contain from three to several dozen nuclei and a lot of lysosomes (See Lysosomes), ... ... Great Soviet Encyclopedia
Osteoclasts - see Bones... Encyclopedic Dictionary F.A. Brockhaus and I.A. Ephron
osteoclasts - osteoclasts, ov, units. part l ast, a... Russian spelling dictionary
osteoclasts - pl., R. osteoclasts; units osteocla/st (2 m) ... Russian spelling dictionary
Osteoclast - Osteoclasts and osteoblasts on the trabecula of the lower jaw of a cow embryo. Osteoclasts are giant multinucleated cells of vertebrate animals that appear in places where bone structures are reabsorbed. Osteoclase diameter ... Wikipedia
Bone - I Bone (os) is an organ of the musculoskeletal system, built primarily from bone tissue. The totality of cells connected (continuously or continuously) by connective tissue, cartilage, or bone tissue forms the skeleton. The total number of K. skeleton ... ... Medical encyclopedia
BONE is a dense connective tissue found only in vertebrates. Bone provides structural support for the body and helps the body maintain its overall shape and size. The location of some bones is such that they serve as protection for soft... ... Collier's Encyclopedia
Bone - This term has other meanings, see Bone (meanings). This term has other meanings, see Bones (meanings). Bone, as an organ of a living organism, sucks ... Wikipedia
The structure of bone tissue
This is a separate type of connective tissue; all bones in the human body are formed from it. It consists of special cells and intercellular substance. The latter includes an organic matrix consisting of collagen fibers (90-95% of the total mass) and mineral components, mainly calcium salts (5-10%). Thanks to this composition, human bone tissue has a harmonious combination of hardness and elasticity. There are three groups of cells: osteoclasts (left), osteoblasts (middle), osteocytes (right in the photo).
Let's look at them in more detail below. The collagen contained in the matrix differs from its counterparts found in other tissues, mainly due to the fact that it contains more specific polypeptides. The fibers are located, as a rule, parallel to the level of the most probable loads on the bone. It is thanks to it that elasticity and firmness are preserved.
If the bone is exposed to hydrochloric acid, the mineral substances will be dissolved, but the organic substances (ossein) will remain. They will retain their shape, but will become overly flexible and highly susceptible to deformation. This condition is typical for young children. They have a high ossein content, so their bones are more elastic than those of adults. And the opposite case occurs when organic substances are lost, but mineral substances remain. This happens if, for example, a bone is burned: it will retain its shape, but at the same time it will become very fragile and can collapse even from a slight touch. The composition of bone tissue undergoes such changes in old age. The share of mineral salts reaches 80% of the total mass. Therefore, older people are more susceptible to various types of fractures and injuries.
If you establish bone tissue density (volume), this will allow you to evaluate the strength of the skeleton and its individual parts. Such studies are carried out using computed tomography. Timely diagnosis allows you to start treatment or maintenance therapy on time.
Working in tandem
Osteoclasts work as a group. They eat into the old bone and create a tunnel in it. The daily passage of such a group is 50 microns. After the passage of the first group, the second, consisting of osteoblasts, begins to move. They are located along the walls of the tunnel and fill their surface. After this, they begin to synthesize the matrix at a rate of 1 micron per day. At the same time, capillaries begin to grow along the axis of the tunnel.
Having built the matrix, osteoblasts begin to wall themselves up, creating a mineral-protein structure around themselves. Upon reaching the goal, when the bone is already built, osteocytes remain in the gaps. They live for some time, after which they end their lives by self-destruction (apoptosis).
The process of two types of bone cells working in tandem is called remodeling. It is regulated by hormones of the parathyroid glands, which activate osteoclasts. This is parathyroid hormone. The thyroid gland produces calcitonin, which stimulates bone formation. In addition to these, many other hormones that are produced by the gonads, pituitary gland and pancreas are involved in remodeling.
If hormones are disrupted, a lack of osteoblasts or their inhibition may occur. Together with osteoclast activity, this can lead to disease. For example, osteoporosis and its consequences: fractures and joint damage.
Osteoblasts (active): structural features
Osteoblasts are bone tissue cells located in its upper layers, having a polygonal, cubic shape with various types of processes. The internal contents are not much different from others. A well-developed granular endoplasmic reticullum contains various elements, ribosomes, the Golgi apparatus, a round or oval-shaped nucleus rich in chromatin and containing a nucleolus. On the outside, these bone tissue cells are surrounded by the finest microfibrils.
The main function of osteoblasts is the synthesis of components of the intercellular substance. These are collagen (mainly the first type), matrix glycoproteins (osteocalcin, osteonectin, osteopontin, bone sialoprotein), proteoglycans (biglycan, hyaluronic acid, decorin), as well as various bone morphogenetic proteins, growth factors, enzymes, phosphoproteins. Impaired production of all these compounds by osteoblasts is observed in some diseases. For example, vitamin C deficiency (scurvy) in children is characterized by impaired bone development and growth due to a defect in the synthesis of collagen and glycosaminoglycans. For the same reason, the restoration of bone tissue and healing of fractures slows down. Since osteoblasts are actually responsible for growth, they are present exclusively in developing bone tissue.
Mechanism of mineralization of organic matrix by osteoblasts
There are two ways:
- Deposition of hydroxylate crystals along collagen fibrils from supersaturated extracellular fluid. A special role is assigned to certain proteoglycans, which bind calcium and retain it in gap areas.
- Secretion of special matrix vesicles. These are small membrane structures that are synthesized and secreted by osteoblasts. They contain high concentrations of calcium phosphate and alkaline phosphatase. The special microenvironment created inside the bubbles favors the formation of the first hydroxyapatite crystals.
The rate of mineralization of osteoid (bone tissue at the stage of formation) can vary significantly; normally it takes about 15 days. Disturbances can occur when the concentration of calcium or phosphate ions in the blood decreases. The result of this is softening and deformation of the bones - osteomalacia. Similar disorders are observed, for example, with rickets (vitamin D deficiency).
Inactive (resting) osteoblasts
They are formed from active osteoblasts; in non-growing bone they cover about 80-95% of its surface. They have a flattened shape with a fusiform nucleus. The remaining organelles are reduced. But receptors that respond to various hormones and growth factors are preserved. The connection between resting osteoblasts and osteocytes is maintained and thus a system is formed that regulates mineral metabolism. If any damage occurs (injuries, fractures), they are activated, and active collagen synthesis and the production of an organic matrix begin. In other words, due to them, bone tissue regeneration occurs. At the same time, they can cause a malignant tumor - osteosarcoma.
Osteocytes: structure and functions
These cells form the basis of mature bone tissue. Their shape is spindle-shaped, with many branches. The organelles are significantly smaller compared to osteoblasts; there is a rounded nucleus (heteochromatin predominates in it) with a nucleolus. Osteocytes are located in lacunae, but do not directly contact the matrix, but are surrounded by a thin layer of bone fluid. It provides nutrition to the cells.
Their processes, which are quite long, up to 50 µm, and located in special tubules, are similarly separated. There are a lot of them, bone tissue is literally permeated with them, they form its drainage system, which contains tissue fluid. Through it, the exchange of substances between the intercellular substance and cells occurs. It is also worth noting that they do not divide, but are formed from osteoblasts and are the main components in the formed bone tissue.
The main function of osteocytes is to maintain the normal state of the bone matrix and the balance of calcium and phosphorus in the body. They are able to perceive mechanical stress and are sensitive to electrical potentials arising from the action of deforming forces. Reacting to them, they trigger a local process in which the connective bone tissue begins to rebuild.
Osteoblasts
The name of these cells comes from the ancient Greek words “bone” and “sprout”. These are young cells that form bone tissue. First they create a matrix, a network of intercellular substance. After this stage, osteoblasts calcify the matrix, while themselves turning into osteocytes.
Osteoblasts have a cubic or pyramidal shape. They have a developed granular endoplasmic reticulum that synthesizes proteins. The Golgi complex brings them into the developing bone. Mitochondria ensure the normal functioning of the cell, providing it with energy. Osteoblasts can divide by mitosis.
The main task of osteoblasts is the formation of matrix proteins, which include collagen, osteocalcin and osteopontin. After their synthesis, the deposition of mineral substances in the matrix begins. They also secrete ossein, which glues calcium salts together. As a result, the bone becomes a mineral-organic structure.
Osteoblasts help transport calcium and phosphate, which helps in alkalizing the body. During bone formation, they are found on the entire surface of bone beams, and after that - in places of destruction and regeneration after injury, as well as in the periosteum.
An osteocyte is called a cell of mature bone tissue. This is a definitive cell, that is, one that has arrived at its final form. It does not have the ability to divide through mitosis. When the matrix structure is completely filled with mineral matter, the osteoblast stops working and the cell becomes an osteocyte. The function of osteocytes is to ensure the maintenance and regeneration of bones, as well as the regulation of mineral composition.
There are gaps in the bone structure in which osteocytes are located. During the process of embedding, osteoblasts create long processes of osteocytes that touch each other with nexuses. The processes located near the vessel receive nutrition and oxygen from it. The number of such processes can be very large, up to several hundred. The osteocyte has a star shape due to the many processes that are located in the bone tubules. After aging and apoptosis (self-destruction), the tubules become empty.
Osteoclasts
This name was given to large cells containing from 5 to 100 nuclei, having a monocytic origin, destroying bones and cartilage or, in other words, causing their resorption. The cytoplasm of osteoclasts contains many mitochondria, elements of the ER (granular) and Golgi apparatus, ribosomes, as well as lysosomes of various functions. The nuclei contain a large amount of chromatin and have clearly visible nucleoli. There is also a sufficient number of cytoplasmic processes, most of them are located on the surface adjacent to the destroyed bone. They increase the area of contact with it. Bone tissue begins to break down when the level of a special hormone (parathyroid) increases, which leads to the activation of osteoclasts. The mechanism of this process is associated with the release of carbon dioxide, which, under the influence of a special enzyme (carbonic anhydrase), is converted into an acid called carbonic acid, which dissolves calcium salts.
Osteoclasts are bone destroyers
The human body consists of many cells. They all have different structures and perform different functions. But there is something that unites all their diversity - this is a constant process of renewal. It can be considered using the example of bone structures. Osteoclast and osteoblast cells are like asphalt-laying crews: some remove old asphalt, others lay new ones. Bone tissue is continuously renewed, and the brain controls this work.
When a failure occurs, there is always a reason: either the brain gave the wrong command, or there was not enough building material, or osteoblasts (cells that build tissue) have decreased in number. And osteoclasts (destroyers) remained in the same number. This leads to various diseases, in particular osteoporosis.
Mechanism of bone resorption
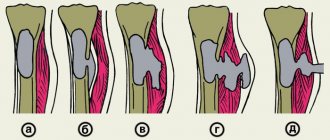
It is worth noting that the destruction process occurs cyclically, and periods of high activity of each cell are invariably followed by periods of rest. Resorption occurs in several stages:
- Attachment of the osteoclast to the destroyed bone surface, with a pronounced restructuring of its cytoskeleton observed.
- Oxidation of the contents of lacunae. This occurs either by the release of vacuole contents, which have an acidic environment, or as a result of the action of proton pumps.
- Destruction of the mineral component of the matrix.
- Dissolution of organic compounds as a result of the action of enzymes secreted by osteoclasts into the lacuna and activated by an acidic environment.
- Removal of bone tissue destruction products.
Regulation of osteoclast activity is determined by general and local factors. The first, for example, include parathyroid hormone and vitamin D, they stimulate activity. Calcitonin and estrogens are inhibitory. Local factors include such a factor as the creation of a local electric field under mechanical stress, to which these cells are very sensitive.
Osteoclast cells
Osteoclasts are giant (40 µm in diameter) multinucleated cells. They destroy bone by dissolving mineral salts and destroying the collagen matrix. They have several nuclei (from 5 to 20), many Golgi complexes, mitochondria and lysosomes. Lysosomes release enzymes that initiate bone resorption.
In other words, an osteoclast is a bone macrophage. It approaches the bone, attaches to it with a corrugated border and forms a membrane that protects the environment of the osteoclast from the action of hormones. It then produces an acidic environment that dissolves the mineral salts. Afterwards, with the help of lysosome enzymes, the old cells are digested. Some of the substances go into the blood, the rest is used to support the process of bone destruction.
The structure of coarse-fiber bone tissue
Its second name is reticulofibrous. It is formed in the embryo as the future basis of bones. In an adult, its presence is minimal; it remains in the sutures of the skull after they heal and in areas where tendons are attached to bones, as well as in areas of osteogenesis, for example, during the healing of various types of fractures. The structure of the bone tissue of this species is specific. Collagen fibers are collected in dense bundles, which are arranged randomly and have “crossbars” between them. It has low mechanical strength, the content of osteocytes is significantly higher compared to the lamellar variety. In pathological conditions, this type of bone tissue growth occurs when a bone is fractured or in Paget's disease.
Features of lamellar bone tissue
It is formed by bone plates having a thickness of 4-15 microns. They, in turn, consist of three components: osteocytes, ground substance and collagen thin fibers. All bones of an adult are formed from this tissue. The collagen fibers of the first type lie parallel to each other and are oriented in a certain direction, while in neighboring bone plates they are directed in the opposite direction and intersect almost at a right angle. Between them are the bodies of osteocytes in the lacunae. This structure of bone tissue provides it with the greatest strength.
Cancellous bone
The name “trabecular substance” is also found. If we draw an analogy, the structure is comparable to an ordinary sponge, built from bone plates with cells between them. They are arranged in an orderly manner, in accordance with the distributed functional load. The epiphyses of long bones are mainly built from spongy substance, some are mixed and flat, and all are short. It can be seen that these are mainly light and at the same time strong parts of the human skeleton, which experience loads in different directions. The functions of bone tissue are in direct relationship with its structure, which in this case provides a large area for metabolic processes carried out on it, gives high strength combined with low mass.
Dense (compact) bone substance: what is it?
The diaphyses of the tubular bones consist of a compact substance; in addition, it covers their epiphyses from the outside with a thin plate. It is pierced by narrow channels, through which nerve fibers and blood vessels pass. Some of them are located parallel to the bone surface (central or Haversian). Others go to the surface of the bone (nutrient openings), through which arteries and nerves penetrate inward, and veins penetrate outward. The central canal, together with the bone plates surrounding it, forms the so-called Haversian system (osteon). This is the main content of the compact substance and they are considered as its morphofunctional unit.
Osteon is a structural unit of bone tissue
Its second name is the Haversian system. This is a collection of bone plates that look like cylinders inserted into each other, the space between them is filled by osteocytes. In the center is the Haversian canal, through which the blood vessels that ensure metabolism in bone cells pass. Between adjacent structural units there are intercalary (interstitial) plates. In fact, they are the remnants of osteons that existed previously and were destroyed at the moment when the bone tissue underwent restructuring. There are also general and surrounding plates; they form the innermost and outer layers of the compact bone substance, respectively.
Osteocytes
An osteocyte is called a cell of mature bone tissue. This is a definitive cell, that is, one that has arrived at its final form. It does not have the ability to divide through mitosis. When the matrix structure is completely filled with mineral matter, the osteoblast stops working and the cell becomes an osteocyte. The function of osteocytes is to ensure the maintenance and regeneration of bones, as well as the regulation of mineral composition.
There are gaps in the bone structure in which osteocytes are located. During the process of embedding, osteoblasts create long processes of osteocytes that touch each other with nexuses. The processes located near the vessel receive nutrition and oxygen from it. The number of such processes can be very large, up to several hundred. The osteocyte has a star shape due to the many processes that are located in the bone tubules. After aging and apoptosis (self-destruction), the tubules become empty.
Periosteum: structure and significance
Based on the name, we can determine that it covers the outside of the bones. It is attached to them with the help of collagen fibers, collected in thick bundles, which penetrate and intertwine with the outer layer of bone plates. It has two distinct layers:
- external (it is formed by dense fibrous, unformed connective tissue, it is dominated by fibers located parallel to the surface of the bone);
- the inner layer is well defined in children and less noticeable in adults (formed by loose fibrous connective tissue, which contains spindle-shaped flat cells - inactive osteoblasts and their precursors).
The periosteum performs several important functions. Firstly, trophic, that is, it provides the bone with nutrition, since it contains vessels on the surface that penetrate inside along with the nerves through special nutrient openings. These channels feed the bone marrow. Secondly, regenerative. It is explained by the presence of osteogenic cells, which, when stimulated, transform into active osteoblasts that produce matrix and cause the growth of bone tissue, ensuring its regeneration. Thirdly, the mechanical or support function. That is, ensuring the mechanical connection of the bone with other structures attached to it (tendons, muscles and ligaments).
Interaction between osteoclasts and osteoblasts
The article was published in: Lietal. (2016) Osteoclast-Derived Exosomal miR-214-3p Inhibits Osteoblastic Bone Formation.
Source: University of Western Australia; Photo: Shutterstock.
Warning:
Discovered by Professor Strukov V.I. The anabolic method of treating osteoporosis using the drugs “Osteomed” and “Osteo-vit” is consistent with human physiology. Professor Strukov V.I. opposes the use of bisphosphonates in the treatment of osteoporosis, since bisphosphonates inhibit the function of osteoclasts and thereby grossly interfere with human physiology. Professor Strukov V.I. believes that the human skeletal system is built very intelligently, and the osteoclast never destroys osteocytes unless the body requires it (the process of bone remodeling). Therefore, under no circumstances should you interfere with the work of the osteoclast. Research by Australian scientists confirms the correctness of Professor Strukov and shows that there is a signaling exchange between osteoclasts and osteoblasts. And increasing the activity of osteoclasts also increases the activity of osteoblasts. Therefore, the use of bisphosphonates that inhibit osteoclast function also leads to suppression of osteoblast function.
Blocking microRNAs to prevent osteoporosis.
Targeting microRNA (RNA - miR-214-3p), which is found to be elevated in older women, could help treat osteoporosis.
MicroRNA (microRNA, miRNA) are “small” non-coding RNA molecules 18-25 nucleotides long (22 on average), found in plants, animals and some viruses, taking part in the transcriptional and post-transcriptional regulation of gene expression by RNA interference. - Translator's note
Researchers from Hong Kong Baptist University have identified microRNAs (miRNAs) naturally produced by bone cells that stimulate bone growth. Their findings, published in Nature Communications, could lead to new treatments for osteoporosis.
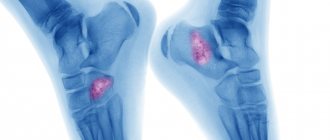
Osteoporosis is a common disease that makes bone brittle and leads to an increased risk of fractures. The main cause of bone fractures in older people is the so-called “silent disease”: you rarely know about it until you break a bone. Osteoporosis occurs when bones lose minerals, particularly calcium, much faster than the body can replace them, thereby causing loss of bone density.
To better understand the cellular mechanism of bone loss, the team focused on two types of cells: osteoclasts, which are responsible for bone resorption and cause bone fractures, and osteoblasts, which form bone and regularly cross-talk in the body.
“Bone remodeling is regulated by two types of cells, each in different ways,” says co-author XuJiake, a professor at the University of Western Australia.
“One classic way they do this is by making proteins, then producing them and binding them to a receptor on another cell or through cell-to-cell contact.”
In addition to protein-based cell signaling, the researchers found that osteoclasts could also produce smallsac-ike structures containing miRNAs that could communicate with other cells.
“We discovered that osteoclasts can send a signal to osteoblasts to stimulate bone growth, so if we could find a way to manipulate this, instead of promoting bone mass growth, it would lead to a new treatment for osteoporosis,” he said.
Read more in Asian Scientist Magazine: https://www.asianscientist.com/2016/03/in-the-lab/osteoporosis-microrna-mir-214-3p/