Body temperature is an indicator of the internal environment of the body. Constancy of temperature is one of the main conditions for normal human life.
The body spends energy on digestion, brain activity, heart beats, muscle contraction and other physiological processes. This energy turns into heat, which is released by the body. The physiological mechanism responsible for body temperature is thermoregulation. Heat balance is controlled by a small region in the brain called the hypothalamus. It monitors the body’s energy expenditure: it can increase or decrease heat transfer.
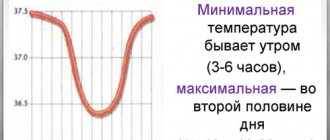
Normal body temperature ranges from 36.5 to 37.5 0C in different parts of the body. During the day, the temperature can fluctuate: at 4–6 am it drops to 35.5–36 0С, in the evening it can rise to 37 0С. This is a daily rhythm, which is caused by different hormonal activity in the evening and morning.
Body temperature is measured in the anus, mouth and armpit. The last option is the most common: when it comes to body temperature, we usually mean measuring the temperature in the armpit. There the average is 36.6 0C.
Stable normal temperature of internal organs and blood maintains the constancy of biochemical reactions, the movement of electrolytes, the viscosity of intracellular fluid and the transport of biological fluids. Temperature also affects the processes of excitation and inhibition in the nervous system, protective reactions of the immune system, the release of hormones and the absorption of nutrients in the digestive tract.
In diseases and pathological conditions, body temperature increases (fever or hyperthermia) or decreases (hypothermia). Based on the dynamics and daily temperature fluctuations, one can suspect the type of infection, the stage of the disease and the degree of its severity.
Reasons for rising temperature
An increase in temperature is an adaptive reaction in response to exposure to pathological factors: bacteria, viruses, parasites, tumors, injuries, poisoning, electric current or endotoxins. An elevated temperature is considered to be an indicator that exceeds 37 0C when measured in the armpit. There are two types of fever - fever and hyperthermia (overheating).
Fever
Fever is a complex process that is activated when the body is exposed to pathogenic factors. Fever involves immune cells and certain hormones.
Fever is characteristic of many infectious diseases and pathological conditions:
- infections: malaria, brucellosis, typhus, tuberculosis, influenza, parainfluenza, measles, rubella, scarlet fever, viral hepatitis, diphtheria, whooping cough, tetanus, polio, cholera, dysentery, salmonellosis, escherichiosis, enterovirus, plague, streptococcus, staphylococcus, cytomegalovirus, parasitic diseases;
- respiratory system: pneumonia, bronchitis, otitis media, sinusitis, laryngitis;
- gastrointestinal tract: appendicitis, gastroenteritis, acute cholecystitis, acute pancreatitis;
- rheumatoid arthritis, reactive and psoriatic arthritis, systemic lupus erythematosus;
- urinary system: pyelonephritis and glomerulonephritis;
- central nervous system: meningitis, encephalitis, meningoencephalitis;
- purulent diseases;
- sepsis;
- malignant tumors;
- recent vaccination.
It is difficult to list all the diseases that cause fever. Almost all of them, which are accompanied by inflammation and cell damage, are manifested by fever. Examples of pathological conditions that can manifest as fever:
- heavy metal intoxication or food poisoning;
- withdrawal syndrome;
- fracture of a limb, dislocation, deep wound, bruise of internal organs;
- electrical injury;
- neuroleptic malignant syndrome;
- teething.
Body temperature can rise even with mental disorders. For example, in febrile schizophrenia, the body temperature exceeds 40 0C.
It is not always possible to determine the cause of fever. For example, there is a pathological condition called fever of unknown origin. It is manifested by one symptom - an increase in body temperature above 380C for more than 3 weeks.
Fever is experienced differently by people. Some people have individual intolerance to high body temperature and experience convulsions. But fever always has common symptoms:
- heart rate increases;
- blood pressure increases;
- sweating increases;
- metabolism accelerates.
Fever is especially difficult for people with cardiovascular, endocrine and neurological diseases. The same applies to older people.
Hyperthermia
Hyperthermia (overheating) is a pathological condition in which the functioning of the thermoregulation center is disrupted and body temperature rises uncontrollably. The endocrine and immune systems do not participate in this process. In this case, anti-inflammatory and antipyretic drugs have no effect. In other words, hyperthermia is a malfunction in the thermoregulation center, and fever is a natural response to a pathogenic factor.
Hyperthermia occurs when compensatory heat exchange mechanisms are strained to the maximum. If you do not create conditions for heat transfer, for example, do not leave the bathhouse or continue to be under the scorching sun, heat stroke occurs.
Causes of hyperthermia:
- thyrotoxicosis – excessive accumulation of thyroid hormones in the blood;
- pheochromocytoma - tumor of the adrenal glands;
- use of muscle relaxants and anesthesia;
- medications: some antidepressants, antipsychotics, drugs against Parkinson's disease, m-anticholinergics.
- long stay in the sun, in a sauna or bath;
- work in a heating microclimate: in a hot workshop or thick clothing.
An increase in body temperature should not always be considered a pathological condition. For example, your temperature may rise during prolonged exercise or while soaking in a hot bath. Body temperature can rise to 37 0C in women during ovulation. This is due to changes in hormonal levels. When menstruation begins, body temperature returns to normal.
Hyperthermia is more difficult for people to deal with than fever. The pathological condition is accompanied by loss of blood electrolytes, convulsions, circulatory disorders, decreased oxygen delivery to the brain, loss of consciousness or psychomotor agitation. In particularly severe cases, hyperthermia leads to death.
How to distinguish hyperthermia from fever
To choose the most effective treatment, you need to know the difference between fever and non-infectious hyperthermia. Main signs of fever:
- body temperature rises when the first symptoms of the disease appear: cough, runny nose, chills;
- increased heart rate and breathing;
- antipyretic drugs are effective;
- symptoms of intoxication are observed: headache, fatigue, increased sensitivity, nausea, loss of appetite.
The main signs of hyperthermia (heat, sunstroke):
- there is a feeling of stuffiness;
- dizziness;
- general weakness;
- strong thirst;
- feeling of squeezing in the heart area;
- aching back pain;
- headache;
- heavy sweating;
- irregular pulse.
Knowing the difference between pathologies means choosing the right treatment tactics and providing first aid as effectively as possible.
Thermoneurosis
Some people note an increase in temperature during psycho-emotional stress. This is how the body reacts to stress. Experts call this manifestation temperature neurosis.
To make a diagnosis, it is necessary to exclude other possible factors that lead to the appearance of low-grade fever: infections, chronic diseases. The patient is given a so-called “aspirin test”. If the temperature decreases after taking aspirin, then the cause is an infection. With thermoneurosis, temperature readings after taking aspirin remain unchanged.
Low-grade fever in this case is due to the reaction of the nervous system to physical and psychological overload. This phenomenon is most often encountered by teenagers and people of a neurotic type, who react more severely to stress than others. A previous illness or injury can give impetus to the development of thermoneurosis. In the treatment of thermoneurosis, priority is given to the patient changing his lifestyle, the ability to relax, and cope with stress. Reflexology, meditation, taking soothing herbal remedies, and moderate physical activity have a positive effect. In severe cases, consultation with a psychologist or psychotherapist may be required. The specialist’s task is to teach the patient to cope with stressful situations that provoke thermoneurosis.
When to lower the temperature
Body temperature should be reduced when it exceeds 38.5 0C in children and adults. However, there are conditions when body temperature needs to be reduced if it has reached 38.0 0C:
- child under 2 months;
- presence of cardiovascular pathology;
- oncological diseases;
- epilepsy;
- hypertonic disease.
If the patient previously experienced convulsions or impaired consciousness at a body temperature of 38.5 0C or higher, medications should be taken at 38.0 0C.
Daily body temperature fluctuations
In the absence of pathology, the difference between morning and evening temperatures reaches 0.5-1.0 °C. Daily fluctuations in core temperature occur in accordance with the so-called “biological clock”. If you measure your temperature in the early morning hours, immediately after sleep, its value will be in the range from 35.60C to 36.10C, and this is completely normal. During the day, with increased physical activity, the thermometer shows the usual value around 36.60C. In the evening, the temperature of healthy people tends to rise slightly. This usually occurs between 16.00 and 18.00. For some, the fluctuations are quite significant: in the evening the temperature reaches the borderline level of 37.20C.
Physiological low-grade fever is easily tolerated and does not require taking antipyretics.
How to reduce a high temperature
7 tips on how to bring down a high fever with a cold or flu:
- the key to everything is sleep and rest;
- drink plenty of fluids - from 2 to 2.5 liters per day;
- choose light or blended food;
- take probiotics;
- don't wrap yourself in clothes.
The following recommendations are general and are not intended for a specific child. Only a doctor can give precise instructions with individual selection of treatment. Self-medication can lead to serious consequences. If a child has a high temperature that rises quickly, call your local pediatrician or an ambulance.
The pathogenetic mechanism of fever is closely related to inflammation. Therefore, anti-inflammatory drugs with an antipyretic (antipyretic) effect are used to lower the temperature. It should be remembered: treatment of fever is the elimination of the symptom, and not the treatment of the disease itself.
There are methods to physically lower body temperature, especially in children. These include: cold heating pads, cold enemas and wiping with cold water. However, it should be remembered that such methods do not have an evidence base. These methods are unsafe and are therefore excluded from protocols for the symptomatic treatment of fever.
The World Health Organization recommends two medications to treat fever: ibuprofen and paracetamol. WHO offers these drugs as the most studied, safe and effective. They rarely have side effects and have the least effect on the liver, so ibuprofen and paracetamol are indicated for children and adults.
How to reduce the temperature of an adult (one of the drugs):
- paracetamol – 650–1000 mg every 6 hours;
- ibuprofen – 400–600 mg every 6 hours.
In this case, the maximum daily dose should not exceed 4 g to avoid toxic manifestations. Take the tablets with plenty of warm water, do not dissolve or chew, or dissolve in water. It is best to take the tablets during or after meals. When taking paracetamol and ibuprofen, you should temporarily avoid other medications against influenza or other infections if they contain acetaminophen, aspirin, naproxen, or any other drug from the group of non-steroidal anti-inflammatory drugs.
How to bring down a child’s temperature (one of the drugs):
- paracetamol – a single dose of 10 mg/kg body weight;
- ibuprofen - a single dose of 5-10 mg/kg body weight (for children over 3 months).
The next dose of one of the medications is after 4–5 hours. Taking the drug is considered effective if after 30 minutes the body temperature has dropped by 0.5–1 0C when measured in the armpit. Remember, you should not self-medicate. To accurately assess your child's condition and give him the right medications, you need to consult a doctor.
In children, fever can be malignant - this is called “pale” fever. It is accompanied by centralization of blood circulation, impaired microcirculation, deterioration of the child’s well-being, severe chills, cold feet and hands, and pale skin. In the case of pale fever, paracetamol or ibuprofen is administered intravenously at a dose of 15 mg/kg body weight.
If there is no paracetamol or ibuprofen at home, you need to use “backup” therapy - a 50% analgin solution intramuscularly at a rate of 0.1 ml per 1 year of the child’s life. However, after administration of the medicine, side effects may occur: allergic reactions and changes in blood tests. However, before you administer analgin, call a doctor. He will assess the child’s condition and tell you exactly whether the medicine needs to be administered.
Due to excessive sweating, fever is accompanied by dehydration. Therefore, during a fever, you should drink a lot of mineral water, tea, fruit drinks, decoctions and juices. In addition, a large amount of fluid promotes detoxification - waste products of viruses or bacteria are eliminated from the body faster. With a fever, appetite decreases. However, you still need to eat. In this state, easily digestible carbohydrates are best: baked goods, sweet drinks, jam or cakes.
If overheating occurs due to sun or heatstroke, the patient must be taken away from the heat source and direct sunlight. The patient should be placed on a bed or sofa in a cool and ventilated room. Next, remove outer clothing and ensure adequate heat transfer. Spray a large amount of room temperature water on your face. Now that the person is safe, call an ambulance. Meanwhile, fan your body with a newspaper or towel, or turn on a fan.
Fever without symptoms: what to do
Sometimes there may be no symptoms of fever: no cough, headaches, runny nose, fatigue or chills. Fever without symptoms can occur in two cases: fever without a source of infection and fever of unknown origin.
Fever without a source of infection affects children under 3 years of age who do not have catarrhal symptoms (runny nose, cough, sputum) and other signs that indicate the cause of the pathology and its location. Fever without a focus of infection occurs with viral and bacterial diseases, most often with pneumococcal infection, Haemophilus influenzae, typhoid and salmonella. In this case, you need to show the child to a pediatrician or call an ambulance, as it is necessary to quickly establish the cause and begin treatment.
Fever of unknown origin is a syndrome in which fever (38.5 0C and above) does not go away on its own and lasts longer than 3 weeks. However, the cause could not be determined after using routine diagnostic methods. Probable causes: infections (most often tuberculosis), autoimmune diseases, malignant neoplasms, medications, alcoholic cirrhosis, Crohn's disease. If you have a fever of unknown origin, you need to see a doctor and be hospitalized so that doctors can monitor the patient constantly.
Classification
Body temperature up to 39°C is considered elevated. She may be:
- subfebrile - no more than 38.0°C;
- febrile - from 38.1 to 39.0°C.
If the temperature rises above 39.1°C, it is considered high (pyretic up to 41°C and hyperpyretic above 41°C).
Body temperature becomes elevated when pyrogens appear in the blood. These may be components of infectious agents or substances whose production is regulated by the immune system. An increase in temperature is most often a normal defensive reaction, and therefore it is not always necessary to bring it down.
Temperature does not go down - when to call an ambulance
After using paracetamol or ibuprofen, body temperature should decrease at a rate of 0.5–1 0 C per hour. However, sometimes the fever remains at the same level, while the patient’s well-being worsens. In what cases should you call an ambulance or go to the hospital yourself if:
- taking medications according to the regimens described above did not produce any effect;
- for “white” fever, analgin had no effect;
- fever is combined with concomitant pathologies: epilepsy, intracranial hypertension, hydrocephalus, congenital heart defects;
- against the background of fever, the patient refuses to drink and eat, has difficulty breathing and cannot sleep;
- fever is accompanied by severe abdominal pain and incessant vomiting.
If the temperature rises, even despite taking medications, most likely this is a pathological variant of fever - hyperthermic syndrome, in which antipyretic drugs are not effective. This is also one of the reasons to call an ambulance and be hospitalized.
5
1
6
Article rating:
5 out of 5 based on 9 ratings
Author: Atamanenko Alena Valerievna
General practitioner, endocrinologist, physiotherapist. Second category. Work experience more than 9 years.
Diagnosis and treatment of fever at the clinic of JSC "Medicine" in Moscow
If signs of fever persist for several days without other visible symptoms, it is recommended to stop self-medicating and seek medical help. You can get it at the clinic of JSC "Medicine" in the Central Administrative District of Moscow, which has its own diagnostic center and outpatient clinic for undergoing prescribed procedures. Patients of the clinic invariably receive attentive attention, the opportunity to save time and money on undergoing research, as well as a guarantee of the security and confidentiality of personal information. Appointments can be made by phone or on the center's website.