Surely each of us has heard about the disease heart failure. But not everyone knows that there is a cardiopulmonary form of the disease. This disease combines a violation of the cardiovascular and pulmonary functions of the body. The catalyst contributing to the development of the disease is increased pressure in the pulmonary circulation. This is a rather complex disease, which includes a lot of symptoms and signs that are not always successfully treatable. Remember that cardiopulmonary failure is a serious condition that requires immediate treatment once diagnosed.
Causes
A disruption in the functioning of the cardiopulmonary system occurs due to one of the following situations:
- Spasm or blockage of the pulmonary artery by blood clots.
- The occurrence of blood clots in the heart cavity.
- Acute stage of bronchial asthma.
- Rapid development of pneumonia.
- Lung injury.
The root cause of the development of cardiopulmonary failure is serious changes in the functioning of the heart. This could be ischemia, heart attack, or valve dysfunction. With the development of this disease, gradual, but sometimes irreversible changes occur in the pulmonary system of the body. These include:
- Pulmonary hypertension, which is hereditary.
- Development of an inflammatory process in the lungs.
- Exacerbation of chronic diseases.
Diagnosis of the disease
As a result of the development of cardiac failure against the background of pulmonary pathology, patients require consultation and observation of several specialists - a cardiologist and a pulmonologist. First, a detailed medical history is collected, the patient is asked about complaints, past illnesses, bad habits, living conditions and professional activities.
Afterwards, the heart is listened to, its boundaries are determined by percussion (by tapping with fingers), and blood pressure is measured. Developing hypertrophy of the right ventricle against the background of high pulmonary pressure gives muffled tones, increased heart rate, and decreased blood pressure. In case of congestion in the lungs, arterial hypertension can be determined.
Expansion of the borders of the heart and changes in lung tissue on radiography
Before starting treatment, instrumental diagnostic methods are prescribed.
- X-ray of the chest organs makes it possible to determine pathological changes in the lung tissue and expansion of the mediastinum to the right.
- Computed tomography is prescribed for an in-depth study of the changed areas of the heart and lungs.
- Echocardiography allows us to identify functional disorders in the functioning of the valve apparatus, myocardial contractility, and changes in cardiac output.
- Electrocardiography provides information about the excitability and conduction function of the heart. Identifies areas of myocardial hypertrophy, localization of ischemic foci, rhythm disturbances. In doubtful cases, monitoring is carried out using a Holter device, which takes ECG readings at short intervals over 24 hours.
- Angiography of pulmonary vessels allows you to visualize the shape and lumen of the vessel, detects blood clots, fusion, and atherosclerotic changes.
- Catheterization with a pressure gauge is carried out to measure pressure in the cardiac cavities and large pulmonary vessels, and is used in the treatment of thrombosis by administering clot-dissolving drugs.
- Spirometry determines the degree of respiratory failure.
Diagnosis of the disease should be carried out in the early stages of the disease. This allows you to avoid the development of irreversible changes in the myocardium, lung tissue, kidneys, liver, and brain. In case of concomitant ailments that contribute to the development of pulmonary hypertension and heart failure, it is necessary to undergo examination at the preclinical stage of the development of the pathology.
Symptoms
In an acute state, cardiopulmonary failure manifests itself as follows:
- The patient's breathing becomes shallow.
- A person experiences suffocation and an acute lack of oxygen.
- Pallor of the skin appears.
- The patient breaks out in a cold sweat.
- There is a sharp pain in the sternum area.
If the disease becomes chronic, the symptoms manifest themselves somewhat differently. At first, the disease develops almost unnoticed by the patient. Over time, the following appear:
- dyspnea,
- cardiopalmus,
- pulsation of the veins in the neck,
- pain in the heart area,
- neurological disorders,
- swelling.
At first, these symptoms appear only after physical activity. As the disease progresses, obvious signs become more pronounced.
Manifestations of chronic form of insufficiency
Clinical signs of the disease depend on the stage of development. When compensating for the pathological process, symptoms of the disease leading to hypertension in the pulmonary circulation are revealed. Chronic failure of the cardiac and pulmonary systems usually develops over several months or years and is characterized by the following manifestations:
- shortness of breath on exertion;
- fast fatiguability;
- pulsation in the epigastric region;
- acrocyanosis (blueness of the fingertips, nasolabial triangle);
- dizziness;
- heartbeat.
In the chronic form of failure, heart pain and shortness of breath occur at rest
In the decompensated stage, symptoms of insufficiency increase and lead to irreversible consequences in all organs and tissues. Manifestations of disease progression include the following signs:
- shortness of breath at rest, worsening when lying down;
- ischemic pain in the cardiac region;
- swelling of the veins of the neck, which persists during inspiration;
- decreased blood pressure, tachycardia;
- bluish tint of the skin;
- enlarged liver, feeling of heaviness in the right hypochondrium;
- edema resistant to treatment.
In the terminal stages of pathology development, against the background of severe hypoxia, toxic encephalopathy (brain damage) and nephropathy (kidney damage) develop. This is manifested by the development of lethargy, apathy, drowsiness, impaired mental functions, and a decrease in diuresis, sometimes until the complete cessation of urine output. In the blood against the background of hypoxia, the content of hemoglobin and red blood cells increases.
Detection methods
Since symptoms of cardiopulmonary failure may indicate a number of other diseases, cardiologists, to determine an accurate diagnosis, carry out a number of necessary measures, which include:
- Study of patient complaints.
- X-ray examination of the lungs, which allows you to determine changes in the pulmonary system and the size of the heart.
- If the previous study did not lead to an accurate diagnosis, an additional CT scan of the chest is performed.
- An ultrasound is required to determine the extent of heart damage.
- To determine the pressure in the lungs and heart, invasive manometry and catheterization are performed.
- In advanced cases, it is necessary to conduct an ECG, which will show the degree of changes in the organs.
3. Symptoms and diagnosis
Following specially developed criteria, three stages of acute respiratory failure are distinguished - from the first, relatively compensated, to the third, which is actually the beginning of agony, the so-called. proceeds to hypoxic coma, convulsions, loss of pupillary reflexes and rapid death.
The most typical symptoms of acute respiratory failure are a feeling of suffocation, reflex tachycardia and tachypnea (respectively, increased heart rate and respiration). Of the mental disorders in the early stages, even euphoria is possible, but then confusion sets in, psychomotor agitation with hallucinatory-delusional inclusions that barely have time to form. Harbingers of the third stage and imminent cardiac arrest are a sharp slowdown in respiratory rate (respiratory rate) to deep bradypnea, arrhythmia at a very high heart rate, and a drop in blood pressure.
In diagnostic terms, the main problem is that there may simply be no time left for diagnosis. Here, often everything depends on the qualifications, experience and, last but not least, the intuition of the doctor and/or members of the resuscitation team: every mistake can be fatal, and every insight (insight) can be life-saving, even if the health worker at that moment does not have time to indulge in logical reasoning . If acute respiratory failure develops, say, in the operating room or intensive care ward, then there are immeasurably more opportunities to assess the situation and respond according to the protocol than when diagnosing ARF in the field, where only the most primitive tools are available (stethophonendoscope, tonometer, portable electrocardiograph) . In the initial stages of acute respiratory failure, an interview is performed (if the patient is conscious and can speak), examination, and auscultation; in a medical facility - emergency laboratory tests, spirometry, EEG, X-rays, ultrasound and other studies, as they say, according to the situation, according to indications and whenever possible.
About our clinic Chistye Prudy metro station Medintercom page!
How to treat?
If cardiopulmonary failure has entered an acute form, treatment is carried out in a hospital under the supervision of cardiologists. Often the patient is admitted to intensive care. Here the patient remains completely at rest and breathes enriched oxygen.
If thromboembolism is detected, streptokinases and actilises are used to help dissolve the thrombotic mass. When using these drugs in the first two to three hours from the onset of an exacerbation of the disease, excellent results can be achieved. In some cases, surgery is performed. However, given the serious condition of the patient, this method is not always appropriate.
If pulmonary heart failure has become chronic, antibiotics and hormone-containing drugs are used to avoid the development of infectious diseases.
Simultaneously with the treatment of pulmonary disease, therapy is carried out aimed at maintaining cardiac activity. Diuretics are prescribed to remove excess fluid from the body, and drugs that stabilize blood pressure.
Thus, cardiopulmonary failure is a serious disease that requires an integrated approach to treatment. In addition to medicinal maintenance of the body, it is important that the patient himself follows all the recommendations of cardiologists, adheres to a certain diet, and gives up drinking alcohol and smoking. At the first manifestations of the disease, you should immediately seek medical help. In case of detection of serious diseases, timely treatment and subsequent prevention play an important role.
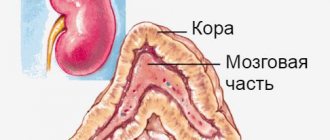
Mechanism of development of SLI
SLN often develops as a complication after diseases that lead to pulmonary hypertension and right-sided heart failure. The first version of the development of SLN begins with a pathology of the lungs, leading to an increase in the stiffness and density of the lung tissue, which is why the right ventricle requires more effort for systole. Subsequently, its wall hypertrophies, and the cavity expands, forming the so-called “pulmonary heart” (CP). Another variant of pathogenesis is associated with the progression of left ventricular heart failure to the last stage, as a result of which blood stagnates in the large and then small circle, increasing the pressure in the pulmonary vessels.
Diagnosis and treatment
The main purpose of the examination is to identify the disease that caused pulmonary heart failure. As part of the diagnosis, the following is prescribed:
- consultations with a pulmonologist and cardiologist;
- chest x-ray;
- study of external respiration function (RPF) - spirometry, pneumotachometry, gas analytical study of external respiration;
- electrocardiography, echocardiography;
- right heart catheterization;
- Ultrasound of the heart;
- if pulmonary embolism is suspected, pulmonary angiography and ventilation-perfusion scintigraphy of the lungs are performed.
Pulmonary heart failure is eliminated with the help of oxygen therapy and medications. It is possible to perform operations - balloon atrial septostomy, sympathectomy, lung tissue reduction, lung transplantation. In acute pulmonary heart failure caused by pulmonary embolism, thromboembolectomy is indicated.
The reception is being conducted
General practitioner, family doctor, cardiologist, doctor of the highest category
Malashkina Irina Borisovna
Make an appointment (video consultation available)
Your message has been sent
Thank you for contacting Multidisciplinary Medical!
Your message will be processed shortly and we will contact you to clarify the details.
Be healthy!
Join us on social networks!
Current news, promotions, useful information.
How to find us
OUR ADDRESS
Moscow, st. Shchukinskaya, 2
Shchukinskaya, Streshnevo, Sokol
TELEPHONE
+7
Respiratory failure - symptoms, classification, degrees, treatment and prolongation of the patient’s life.
Respiratory failure (RF) is a pathological syndrome that includes several diseases based on impaired gas exchange in the lungs. External respiration maintains constant gas exchange in the body, i.e. supply of oxygen from the atmosphere and removal of carbon dioxide. Any disruption of the function of external respiration leads to disruption of gas exchange between the alveoli of air in the lungs and the gas composition of the blood. As a result of these disorders, the carbon dioxide content in the blood sharply increases, while the oxygen content decreases, which leads the patient’s body to oxygen starvation (hypoxia) of vital organs such as the heart and brain. This is a dangerous and developing condition for the patient’s body in case of respiratory failure, characterized by a decrease in the partial pressure of oxygen in arterial blood < 60 mm Hg, while the partial pressure of carbon dioxide increases > 45 mm Hg.
Causes and classification of respiratory failure
Impaired pulmonary ventilation and the development of respiratory failure leads to a number of acute and chronic diseases of the bronchopulmonary system (pneumonia, atelectasis, disseminated processes in the lung, abscesses, etc.), damage to the central nervous system, anemia, hypertension in the pulmonary circulation, vascular pathology of the lungs and heart, lung tumors, etc.
Respiratory failure is classified according to the following criteria:
1. According to the mechanism of occurrence (pathogenesis):
• parenchymal (respiratory or pulmonary failure of the 1st type) Respiratory failure of the parenchymal type is characterized by a decrease in the oxygen content, as well as the partial pressure of oxygen in the arterial blood (so-called hypoxemia), while it is difficult to correct with oxygen therapy. The most common causes of this type of respiratory failure include the following diseases: pneumonia, respiratory distress (also called “shock lung” syndrome), cardiogenic pulmonary edema.
• ventilation (hypercapnic or respiratory failure type 2) Manifests itself in the event of an increase in the partial pressure of carbon dioxide in the arterial blood (so-called hypercapnia). The presence of hypoxemia is also observed in the blood, but it can be easily cured with sessions of long-term oxygen therapy. The development of ventilation respiratory failure occurs in patients with weakened respiratory muscles, as a result of any defects in the muscular and rib cage of the chest, a violation of the regulatory function of the respiratory center.
2. For reasons: • obstructive • restrictive or restrictive • mixed or combined • hemodynamic • diffuse
3. According to the rate of growth of symptoms: • acute • chronic
4. In terms of blood gas composition: • compensated (blood gas composition is normal); • decompensated (ie, the presence of hypoxemia and/or hypercapnia of arterial blood).
5. According to the severity of symptoms of DN (respiratory failure): • 1st degree DN – mainly characterized by shortness of breath under moderate or heavy exertion; • 2nd degree DN – shortness of breath can be observed with minor exertion; • DN 3rd degree – manifested by shortness of breath and “bluish” coloration of the skin at rest, hypoxemia.
Symptoms of respiratory failure (RF)
Signs of respiratory failure may directly depend on the causes of its occurrence, type and severity. Characteristic signs of respiratory failure include: • detection of hypoxemia; • detection of hypercapnia; • weakness syndrome and/or fatigue of the respiratory muscles; • shortness of breath • edema Hypoxemia mainly manifests itself in the form of a “bluish” coloration of the skin, the degree of which expresses the severity of DN. It is observed when the partial pressure of oxygen in arterial blood decreases to <60 mmHg. When the partial pressure of oxygen in arterial blood decreases to 55 mm Hg, the patient experiences memory impairment for current events, but if the partial pressure drops to 30 mm Hg, the patient simply loses consciousness. If a person has chronic hypoxemia, it manifests itself in the form of pulmonary hypertension.
Hypercapnia causes an increase in heart rate (tachycardia), sleep disturbances (apnea), nausea, or brain spasms. A rapid increase in the partial pressure of carbon monoxide (carbon dioxide) in arterial blood can lead to a state of so-called hypercapnic coma, which can lead to the development of cerebral edema.
With the syndrome of weakness and/or fatigue of the respiratory muscles, an increase in respiratory frequency (RR) occurs, which leads to the active involvement of auxiliary muscles in the inhalation process (the muscles of the upper respiratory tract, neck muscles and abdominal muscles are involved). A respiratory rate of more than 25 breaths per minute can serve as an initial sign of fatigue of the respiratory muscles. If the respiratory rate is < 12 breaths per minute, this may cause complete respiratory arrest.
The patient's shortness of breath is mainly felt as a lack of air (oxygen) due to excessive breathing efforts. Shortness of breath in a patient, if he has respiratory failure, is observed both during physical activity and in a state of calm.
The patient's edema appears in the late stages of chronic respiratory failure with manifestations of heart failure.
Complications of respiratory failure
Respiratory failure is an emergency condition that threatens the health and life of the patient. If timely resuscitation is not provided, DN can lead to the death of a person. Long-term course, as well as progression of chronic respiratory failure (CRF), can lead to the development of heart failure. This occurs as a result of not complete, but partial supply of oxygen to the heart muscle and its constant overload. A decrease in the partial pressure of oxygen in the alveolar air and abnormal ventilation of the patient's lungs during respiratory failure can cause the development of pulmonary hypertension. Excessive growth of the right ventricle of the heart, as well as a further decrease in its contractions lead to the development of cor pulmonale, which manifests itself in an increase in pressure in the pulmonary circulation.
Diagnosis of respiratory failure
At the beginning of the diagnosis of DN, a medical specialist thoroughly collects information on the physical, mental and social development of the patient and his concomitant diseases in order to detect possible causes of the development of respiratory failure. As a result of examining the patient, the doctor observes whether there are signs of “bluish” coloration of the skin (signs of cyanosis), counts the frequency of the respiratory muscles, and checks whether auxiliary muscle groups are involved in breathing. skin color (signs of cyanosis), counts the frequency of the respiratory muscles, checks whether auxiliary muscle groups are involved in breathing. The next stage of diagnosis is conducting functional tests to study the functions of external respiration. Carrying out spirometry and peak flowmetry, which allow assessing the ability of the lungs to ventilate. In this case, the following is measured: • the maximum amount of air that can be taken into the lungs after maximum exhalation, • the volume of breathing per minute, • the speed of air movement through different parts of the respiratory tract during deep exhalation “through force” at high speed, etc. Laboratory gas analysis blood composition is a necessary diagnostic test for diagnosing respiratory failure.
Prognosis and prevention of respiratory failure
Respiratory failure can lead to serious complications of various diseases, and often leads to death. Respiratory failure develops in 30% of patients with chronic obstructive pulmonary disease (COPD).
Poor prognosis in patients with respiratory failure in whom neuromuscular diseases progress (amyotrophic lateral sclerosis, myotonia, etc.). If you do not adhere to the doctor's recommended therapy, death can occur within 1 year.
For other pathologies that cause the development of DN, the prognosis of doctors is different, although it cannot be denied that respiratory failure is a factor that shortens the life expectancy of patients if they do not adhere to the recommendations of the attending physician for its treatment.
Prevention of the development of DN involves eliminating the mechanism of origin, development of the disease and its individual manifestations, as well as the causes of its occurrence.
Treatment of respiratory failure
Treatment of patients with DN includes: • restoration and maintenance in optimal condition of ventilation of the lungs for life support of the body and the procedure for hardware saturation of the blood with oxygen; • treatment of a number of diseases that were the root cause of the development of respiratory failure (pneumonia, exudative pleurisy, pneumothorax, chronic inflammatory process in the bronchi and lung tissues, etc.). If signs are detected: • hypoxemia; • weakness and/or fatigue of the respiratory muscles; • shortness of breath; • in initial swelling of the body, experienced doctors recommend oxygen therapy sessions using oxygen cartridges or an oxygen concentrator. Inhaled oxygen should be given in concentrations that maintain arterial oxygen pressure between 55 and 60 mm Hg, with careful monitoring of the patient's arterial blood pH and partial pressure of carbon dioxide (PaCO2). If the patient is able to breathe on his own, then oxygen is supplied to him through a mask or through nasal cannulas; in a comatose state, oxygen is supplied together with an artificial lung ventilation device (ventilator). Along with oxygen therapy sessions (oxygen therapy), the following procedures should be carried out: • chest massage; • inhalation therapy (an inhaler with a nebulizer is required) • physical therapy; • bronchial secretions are “sucked in” through an endobronchoscope; • procedures that can improve the drainage function of the bronchi (it is necessary to prescribe antibacterial drugs, bronchodilators, mucolytics; The process of further treatment of respiratory failure is aimed at eliminating the causes that caused this respiratory failure.
What is the best choice for oxygen therapy for respiratory failure?
Oxygen cartridges are a cost-effective and convenient means of treating respiratory failure. They do not require setup, special handling or maintenance skills, and are convenient to take with you. Below is a selection of the most popular oxygen tank models:
However, it is worth considering that oxygen cans have some disadvantages. Firstly, canisters tend to run out - on average, a nine-liter canister is enough for 70 - 100 breaths, and if long-term treatment is necessary, then a large supply will be needed. Secondly, if DN is a concomitant effect of another disease, the cans are likely to be useless.
In such cases, oxygen concentrators have an undeniable advantage. These are devices that produce an oxygen-enriched mixture for breathing from the surrounding air. This oxygen therapy compensates for DN, which leads to a decrease in shortness of breath and intoxication:
———————————————————————
The article was prepared by Vadim Mikhailovich Gershevich (thoracic surgeon, candidate of medical sciences).
Still have questions? Call us now on our toll-free line 8 (800) 100-75-76 and we will be happy to provide expert advice and answer all your questions.
Causes of heart failure
A variety of diseases can lead to this disease, but more often its development is facilitated by:
- cardiac ischemia;
- arterial hypertension;
- heart defects;
- myocardial infarction;
- myocarditis;
- cardiomyopathy (including alcoholic);
- arrhythmias;
- thyroid diseases;
- diabetes.
Risk factors for developing heart failure include smoking, drinking alcohol or drugs, taking certain medications, and being overweight.
1 ECG for heart failure
2 Ultrasound for heart failure
3 ECHO-CG for heart failure
What is heart failure?
Our heart is like a pump that pumps blood and supplies oxygen and nutrients to all parts of the body. Impaired ability of the heart to pump blood leads to stagnation and leads to the development of heart failure .
Poor blood supply puts other organs and tissues at risk. In terms of prevalence, heart failure rivals the most well-known infectious diseases.
According to statistics, around 28 million people suffer from heart failure throughout Europe. In our country, the number of patients with this disease exceeds 9 million (more than 25% of them are under 60 years of age)! At the same time, Russians die from it 10 times more often than from myocardial infarction.
1 Tests for heart failure
2 Tests for heart failure
3 Tests for heart failure
Diagnosis of heart failure
When diagnosing a disease, it is extremely important to identify the true cause of its development - only then can treatment be as successful as possible.
After collecting an anamnesis and physical examination, a cardiologist may prescribe:
- general clinical, biochemical blood and urine tests;
- electrocardiography (at rest);
- Ultrasound of the heart (Echocardiography);
- chest x-ray;
- coronary angiography;
- Holter ECG monitoring and other studies.