How can a baby become infected?
According to statistics from the Ministry of Health, most cases of staphylococcal infection occur within the walls of the maternity hospital.
The bacterium is very tenacious, and it is extremely difficult to fight it, despite the maximum range of measures carried out in maternity hospitals (sterilization of diapers, bed linen and other household items used in the ward).
It is precisely because of the frequent infection with Staphylococcus aureus that in some institutions women in labor are prohibited from using their own clothing, with the exception of underwear, and there are also restrictions on washing wardrobe items.
A newborn can become a carrier of staphylococcus after passing through the mother's birth canal, so all women at 36-38 weeks are recommended to undergo complete vaginal sanitation.
At home, a baby can “catch” an infection from one of the family members through toys, common objects, or tactile contact (for example, by kissing).
If the child is breastfed, the mother should carefully monitor her health and hygiene, since Staphylococcus aureus can penetrate into mother's milk, actively multiplying in the nutrient medium.
Who's at risk
Generally speaking, this includes all babies under the age of one year, since their immune system is just being formed and cannot cope with pathogens on its own.
The most vulnerable groups of children, whose risk of infection increases by 50-70 percent compared to their peers, include:
- born prematurely;
- having a critical body weight at birth;
- those who underwent surgery in the first year of life;
- having congenital defects and developmental pathologies;
- those who are bottle-fed;
- often sick;
- recently vaccinated;
- not receiving sufficient hygienic care.
The main cause of staphylococcal infection is decreased immunity.
If the child is strong, healthy, and his immune system works well, then the body will cope with the bacteria on its own, and more precisely, it will not allow opportunistic organisms to grow, multiply and leave their waste products.
What is staphylococcus
It is a nonmotile, spherical, Gram-positive microorganism that forms numerous colonies. Staphylococci are anaerobic - they can exist and reproduce without oxygen, in a closed environment. There are more than twenty strains of bacteria. Some of them are quite harmless, while others cause powerful pathological reactions in the human body. Parts of the body and organs most vulnerable to staphylococci:
- leather;
- mucous membranes;
- connective tissue;
- subcutaneous tissue;
- nerve tissue;
- heart muscle.
By infecting them, microbes produce toxic substances and provoke inflammation, which in severe cases leads to sepsis, irreversible changes in structures or permanent dysfunction.
Why is Staphylococcus aureus dangerous for babies?
Staphylococcus in itself does not pose a threat to the child, since it is part of his natural microflora. But this only applies to healthy children with a good defense system.
If the baby’s health is undermined (for example, by a cold), then favorable conditions are created in the body for the growth of a pathogenic mass of bacteria, including Staphylococcus aureus. This type of microorganism can provoke the appearance of any diseases, as it is localized on the skin and mucous membranes of the eyes, intestines, stomach, etc.
If the infection is not treated completely, serious complications may occur, for example:
- chronic conjunctivitis;
- pneumonia;
- inflammation of the meninges (meningitis);
- blood poisoning as a result of Staphylococcus aureus entering it (sepsis);
- otitis;
- sinusitis;
- damage to internal organs.
Sepsis and meningitis are extremely serious diseases for infants, which can result in the death of the child. For this reason, you should not self-medicate - you should immediately contact your pediatrician if any symptoms indicating the presence of staphylococcus appear.
Forms of the disease and accompanying symptoms
Staphylococcus aureus on the skin
If this representative of the staphylococcus family infects the skin of infants, characteristic symptoms appear:
- redness and peeling of the skin;
- rashes that have a shiny tint;
- blisters and pustules;
- boils;
- acne;
- “scalded skin syndrome” (severe redness and swelling of individual areas of the skin with blisters filled with fluid or pus).
Similar phenomena occur as a result of the release of the toxic substance exfoliatin into the skin. In this case, it is very difficult to suspect staphylococcus, since outwardly it resembles the symptoms of urticaria, diathesis and dermatitis, which are often diagnosed in infants. It is impossible to determine it yourself, without conducting the necessary research.
If the baby becomes capricious and signs of an allergic reaction appear on the body, do not rush and give him antihistamines. It would be wiser to go to a children's clinic and get the necessary tests.
Infection on the mucous membranes
In such a situation, a baby develops inflammatory diseases of the eyes (conjunctivitis), nasopharynx and throat, which are accompanied by a high temperature and are quite acute, causing discomfort and pain.
Doctor's advice
Today, bacteriophages are the most optimal means of therapy, but have one drawback - price. The solution is used depending on the affected area - internally, externally in the form of lotions, rinsed the mouth with it and made enemas. The main advantage is that bacteriphages destroy staphylococcus, die and leave the body without being involved in other processes.
Victoria Druzhikina Neurologist, Therapist
The signs are identical to ARVI and acute respiratory infections:
- runny nose, nasal congestion;
- cough, sneezing;
- fever;
- chills;
- irritability and tearfulness.
Staphylococcus in the intestines
Enterocolitis is a common problem in infants infected with staphylococcus. The disease is accompanied by symptoms of intestinal poisoning, intoxication and eating disorders.
When staphylococcus occurs in the intestines, the following symptoms appear:
- bloating;
- frequent attacks of intestinal colic;
- vomiting (not to be confused with regurgitation);
- diarrhea (the stool is watery, bright yellow with greens);
- pain in the abdominal area;
- elevated temperature (up to 38.3-38.5 degrees).
Treatment of enterocolitis does not always require the use of antibiotics - in most cases, symptomatic treatment and taking bifid medications are sufficient.
Staphylococcal infection in children
A staph infection can cause many symptoms. This depends on the location of the infection in the body and the severity of the primary inflammatory focus. Staphylococcal infection in children can be generalized or localized in form.
Most cases are localized mild forms, for example, nasopharyngitis or rhinitis. Minor inflammatory changes are observed, there is no intoxication. In infants, these forms may manifest as poor appetite and insufficient weight gain. Blood cultures can isolate staphylococcus.
But localized forms do not always go away easily; they can be accompanied by severe symptoms, severe intoxication and bacteremia, which is why it may be necessary to differentiate them from sepsis.
The disease can occur in an asymptomatic or erased form. They are not diagnosed, but are dangerous for the child and others, since an infected child spreads the infection. In some cases, another disease is added to the disease, for example, ARVI, which leads to an exacerbation of staphylococcal infection and complications, in some cases very severe.
For staphylococcal infection, the incubation period lasts from 2-3 hours to 3-4 days. The shortest incubation period for the gastroenteroscolitic form of the disease.
Most often, staphylococcal infection in children is localized on the skin and subcutaneous cells. With a skin staphylococcal infection, an inflammatory focus quickly develops with a tendency to suppuration and a reaction of regional lymph nodes such as lymphadenitis and lymphangitis. In children, staphylococcal skin lesions usually take the form of folliculitis, boils, pyoderma, phlegmon, carbuncle, and hidradenitis. Newborns may have Ritter's exfoliative dermatitis, neonatal pemphigus, and vesiculopustulosis. If the infection affects the mucous membranes, symptoms of purulent conjunctivitis and tonsillitis appear.
Staphylococcal tonsillitis in children as an independent disease is a rather rare phenomenon. This usually occurs against the background of acute respiratory viral infection, in some cases due to exacerbation of chronic tonsillitis or as a result of sepsis.
With staphylococcal tonsillitis in children, continuous overlays appear on the palatine tonsils, sometimes they also affect the arches and uvula. In some cases, tonsillitis is follicular. Overlays with staphylococcal tonsillitis in most cases are purulent-necrotic, whitish-yellowish, loose. It is relatively easy to remove them, as well as to grind them between glass slides.
There are extremely rare cases when, due to a staphylococcal infection, the overlays are dense, it is difficult to remove them, and removal causes bleeding of the tonsils. Staphylococcal tonsillitis is characterized by diffuse, bright hyperemia and hyperemia of the mucous membranes of the pharynx without clear boundaries. The child may complain of severe pain when swallowing. The reaction of regional lymph nodes is pronounced. Staphylococcal tonsillitis takes quite a long time to resolve. Symptoms of intoxication and elevated body temperature persist for about 6-7 days. The pharynx is cleared on days 5-7 or on days 8-10. Without laboratory methods, it is impossible to understand that a sore throat is staphylococcal.
Staphylococcal laryngitis and laryngotracheitis are common mainly in children 1-3 years old. They develop against the background of ARVI. The disease is characterized by an acute onset, elevated temperature, and laryngeal stenosis quickly appears. Morphologically, a necrotic or ulcerative-necrotic process in the larynx and trachea is noted. Staphylococcal laryngotracheitis often occurs with obstructive bronchitis and, in rare cases, pneumonia. The symptoms of staphylococcal laryngotracheitis in children are almost no different from laryngotracheitis caused by other bacterial flora. The disease is very different only from diphtheria croup, which develops slowly, with a gradual change of phases, a parallel increase in symptoms (hoarseness, aphonia, dry, rough cough and a gradual increase in stenosis).
Staphylococcal pneumonia is a special form of lung damage with a characteristic tendency to abscess formation. Young children are more susceptible to the disease than others. It begins in most cases during or after ARVI. As an independent disease not accompanied by others, staphylococcal pneumonia is extremely rare.
The disease begins acutely or violently, body temperature is greatly elevated, and severe symptoms of toxicosis are observed. In more rare cases, staphylococcal pneumonia in children may begin gradually, initially followed by minor catarrhal symptoms. But even in these rare cases, the patient’s condition quickly deteriorates sharply, the temperature “jumps” greatly, intoxication intensifies, and respiratory failure increases. The child is lethargic and pale, he is drowsy, does not want to eat, spits up, and often vomits. Shortness of breath, shortening of the percussion sound, a moderate amount of fine moist rales on one side and weakened breathing in the affected area are recorded.
With staphylococcal pneumonia, bullae form in the lungs. These are air cavities, the diameter of which is 1-10 cm. They can be identified by taking an x-ray. Infection of the bulla threatens lung abscess. Breakthrough of a purulent focus leads to purulent pleurisy and pneumothorax. Deaths are common with staphylococcal pneumonia.
, scarlet fever-like syndrome may appear . Most often this happens with staphylococcal infection of a wound or burn surface, lymphadenitis, phlegmon, osteomyelitis.
The disease manifests itself as a scarlet-like rash. It occurs on a hyperemic (reddened) background, is formed from small dots, and is located, as a rule, on the lateral surfaces of the torso. When the rash disappears, abundant lamellar peeling is observed. During this form of the disease, the child’s body temperature is high. The rash appears 2-3 days after the onset of the disease and later.
Lesions of the gastrointestinal tract by staphylococcus can be located in various places (in the stomach, intestines, on the mucous membranes of the mouth, in the biliary system). The severity of such diseases also varies.
Staphylococcal stomatitis mainly affects young children. There is a pronounced hyperemia of the oral mucosa, the appearance of aphthae or ulcers on the mucous membrane of the cheeks, on the tongue, etc.
Staphylococcal gastrointestinal diseases are gastritis, gastroenteritis, enteritis, enterocolitis, which occur when infected through food. In children under 12 months of age, enteritis and enterocolitis often occur as secondary diseases against the background of another staphylococcal disease. If the route of infection is contact, and enteritis or enterocolitis occurs, a small amount of the pathogen is in the body. Staphylococci cause local changes when multiplying in the intestines, as well as general symptoms of intoxication when the toxin enters the blood.
With gastritis or gastroenteritis of staphylococcal nature, the incubation period lasts 2-5 hours, followed by an acute onset of the disease. The most striking symptom is repeated, often uncontrollable vomiting, severe weakness, severe pain in the epigastric region, and dizziness. Most sick children have a fever. The skin is pale and covered with cold sweat, the heart sounds are muffled, the pulse is weak and rapid. In most cases, damage occurs to the small intestine, which leads to bowel dysfunction. Bowel movements occur 4 to 6 times a day, the stool is of a liquid consistency, watery, and contains some mucus.
The most severe manifestation of staphylococcal infection is staphylococcal sepsis. It occurs more often in young children, mainly in newborns; premature infants are at particular risk. The pathogen can enter the body through the umbilical wound, gastrointestinal tract, skin, tonsils, lungs, ears, etc. This causes the type of sepsis.
If staphylococcal sepsis is acute, the disease develops rapidly, and the patient’s condition is characterized as very severe. The body temperature is greatly elevated, and symptoms of intoxication are pronounced. Petycheal or other rashes may appear on the skin. Secondary septic foci appear in various organs (abscesses, abscess pneumonia, purulent arthritis, skin phlegmon, etc.). A blood test reveals neutrophilic leukocytosis with a shift to the left, ESR is increased.
There is a (very rare) fulminant course of the disease, which ends in death. But in most cases the course is sluggish, with low-grade fever and mild symptoms of intoxication. Children sweat, pulse instability is noted, abdominal bloating occurs, the liver and spleen may be enlarged, dilated veins are noted on the anterior abdominal wall and chest, and stool disorders are often among the symptoms. Sepsis in young children can manifest itself with various symptoms, which complicates its diagnosis.
Staphylococcal infection in newborns and children of the 1st year of life is associated primarily with maternal illness. Infection of a child occurs at any stage of pregnancy, during and after childbirth.
Diagnosis of the disease
It is extremely difficult to recognize an infection, since the clinical picture of the disease is absolutely identical to respiratory (cold) diseases and intestinal poisoning. It is possible to make a correct diagnosis and begin the necessary treatment in a timely manner only after a complete examination of the child and collection of a medical history.
Analysis of stool for dysbacteriosis is not very informative in infants in the first months of life. The intestinal microflora is just being formed; everything that gets into the baby’s mouth from a pacifier, toy, hands, mother’s clothes and others passes through the intestines in transit without staying there. The composition of the microflora can change every few days.
Victoria Druzhikina
Neurologist, Therapist
To diagnose staphylococcal infection in infants, the following methods are used:
- Blood test for antibodies . When pathogenic microorganisms begin to grow and release toxic substances, the body reacts by producing antibodies that can fight the foreign agents. Clinical examination of blood serum allows the detection of these antibodies and the presence of a bacterial infection.
- Bacterial culture . The analysis proceeds as follows: a scraping (smear) of the contents is taken from the baby’s mucous membranes and sent to the laboratory to determine the pathogenic microflora. The same method is used to determine the resistance of staphylococcus to various groups of antibiotics. In addition to scraping from the mucous membranes, the baby's feces are sown on nutrient media to detect the growth of staphylococcus and determine its quantity.
- PCR . It is used as a clarifying component of diagnosis if previous methods did not provide a complete picture of the child’s condition. The accuracy of PCR is 98 percent and virtually eliminates the possibility of error.
If the baby is breastfed, the mother's milk must be tested for the presence of this type of bacteria. If they are detected, lactation will have to be temporarily stopped, and the mother will have to undergo a course of treatment using antibiotics.
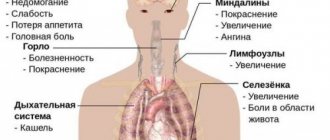
Symptoms of staphylococcus
The clinical picture of the disease in children can vary significantly. With sufficiently active immunity, the phenomenon of asymptomatic bacteremia can even be observed, when the pathogen is detected in the patient’s blood, but does not affect his well-being and the functioning of his internal organs. Factors that influence the severity of the pathological process are the individual characteristics of the child’s immune defense, his age, the type of bacteria, and the amount of pathogen that has entered the body. Possible symptoms of the disease are:
- pustular skin lesions with the formation of boils or even carbuncles;
- itching of the skin, the appearance of red rashes or areas of increased pigmentation;
- local inflammation of the oral mucosa (stomatitis), eye conjunctiva (conjunctivitis) and the like;
- increased body temperature;
- emotional lability;
- general weakness, loss of appetite, disruption of normal sleep rhythm;
- nausea, vomiting, abdominal pain, flatulence, diarrhea;
- enlarged tonsils and redness of the throat.
If at least a few of these symptoms are detected in a child, you should immediately seek help. Specialists will be able to quickly determine the type of pathogen and the cause of the deterioration of the baby’s condition, and will also prescribe adequate drug treatment.
Treatment
If staphylococcus is detected in the stool of an infant, specific treatment is usually not prescribed. This applies to those cases when the child is active, gains weight well and eats with appetite. If the baby often cries and refuses to eat, then the pediatrician may prescribe a course of treatment to eliminate the symptoms of intoxication and restore beneficial microflora.
Treatment of Staphylococcus aureus in children under one year of age can take place in an infectious diseases hospital (if there are complications in the form of severe intoxication or infection of internal organs) or at home if the infection is mild.
The following groups of drugs are usually used:
- Antibiotics . The choice of drug depends on the age of the child, as well as the sensitivity of the strain of staphylococcal bacteria to a specific type of drug (determined using a laboratory test). Antibiotics must be taken for any form of staphylococcus that affects the skin or mucous membranes.
- Immune stimulants (immunomodulators) . Can only be taken as prescribed by a doctor, despite the fact that the drugs of this pharmacological group are sold without a special prescription.
- Bacteriophages . Expensive drugs used to destroy staphylococcus in cases where therapy with standard antibiotics is ineffective. Most pediatricians prefer to immediately prescribe bacteriophages to minimize the toxic effect on the child’s liver.
- Bifid drugs (prebiotics) . Prescribed simultaneously with antibiotics to prevent dysbiosis and restore the normal balance of intestinal microflora.
The condition in which the child is a carrier of Staphylococcus aureus should not be confused with a bacterial infection. Staphylococcus can peacefully coexist with other types of bacteria that populate the human intestine throughout its life, without manifesting itself in any way. An infection is said to occur when pathogenic organisms begin to actively grow and release toxins, infecting organs and poisoning the body.
Treatment of Staphylococcus aureus in infants is a very complex topic and has not yet been fully studied. World-famous pediatricians still cannot come to a unanimous opinion on whether this infection should be treated. If you detect signs of staphylococcus infection, it is important to consult a doctor to avoid dangerous complications and negative consequences for the baby’s health.
For information on the treatment of Staphylococcus aureus in children, see the video “Doctor Komarovsky’s School”:
This article has been verified by a current qualified physician, Victoria Druzhikina, and can be considered a reliable source of information for site users.
Bibliography
1. https://med.wikireading.ru/3098 https://vmede.org/sait/?page=35&id=Infekcionnie_bolezni_ped_y4aikin_2013&menu=Infekcionnie_bolezni_ped_y4aikin_2013
Rate how useful this article was
4.3 6 people voted, average rating 4.3
Did you like the article? Save it to your wall so you don’t lose it!