What is staphylococcus
This term usually refers to microorganisms - cocci, which have the appearance of oval or round bacteria. There are 27 species of staphylococci, but only a few of them pose a real threat to the body. Staphylococcal infection is resistant to temperature and treatment. Therefore, drugs produced 5-6 years ago are useless today.
Causes
Staphylococcus can enter the vagina in several ways:
- airborne (you can become infected during an acute respiratory viral infection or influenza epidemic);
- contact and household (non-compliance with personal hygiene rules);
- airborne dust (inhalation of potentially dangerous street dust, animal hair, plants, etc.);
- fecal-oral (“disease of unwashed hands”, eating vegetables and fruits that they forgot or did not want to wash).
Staphylococcus is present everywhere, including on human skin and in the intestines. If the bacterium gets on the mucous membranes, then under favorable conditions it will begin to multiply intensively. There have been cases of infection in the gynecological office, during the examination, but the most common reasons are: unprotected sexual intercourse and frequent use of tampons. These feminine hygiene products are made from synthetic materials and create favorable conditions for the development of bacteria.
If staphylococcus is detected in the smear, this may indicate:
- The presence of diseases of the reproductive organs.
- Hormonal disbalance.
- Injury to the mucous membranes of the vagina.
- Venereal diseases.
- Exacerbation of chronic diseases.
- The beginning of the inflammatory process.
The detection of staphylococcus in a smear is not always a sign of disease. After all, this is how a woman’s body can react to wearing synthetic underwear or taking any medications for a long time.
Secret weapon
The product of the lug operon isolated by Zipperer turned out to be a non-ribosomal cyclic peptide consisting of five amino acids (two D-valines, L-valine, D-leucine and L-tryptophan) and a thiazolidine heterocycle (Fig. 4). The antibiotic was named lugdunin.
Figure 4. Gene cluster, biosynthetic pathway, and chemical structure of lugdunin. a — Genes of “subunits” (not modules!) of non-ribosomal peptide synthetase of S. lugdunensis: lugA, B, C and D. b — Functional domains of operon products: A - adenylating, P - peptidyl, C - condensing, E - epimerizing, R - reductase. Their specific combinations make up modules—the individual catalytic units of an enzyme. The biosynthesis of lugdunin apparently begins in the initiator module LugD and continues sequentially with the help of LugA-C. c — Structural formula of lugdunin.
[1]
By chemical synthesis, it was possible to obtain a product with chemical properties and antibacterial effect identical to natural lugdunin. Scientists have suggested that this antibiotic inhibits the synthesis of bacterial biopolymers - proteins, DNA and peptidoglycans [5].
Non-ribosomal peptides
This class of peptides is synthesized in the cells of lower fungi and bacteria without the participation of ribosomes. Non-ribosomal peptides (NRPs) are also found in higher organisms that have commensal bacteria [12].
NRPs are divided into several functional groups [13]:
- antibiotics (vancomycin);
- antibiotic precursors (ACV tripeptide - a precursor to penicillin and cephalosporin);
- immunosuppressants (cyclosporine);
- antitumor peptides (bleomycin);
- siderophores (pyoverdine);
- toxins (HC-toxin);
- surfactants (surfactin).
Structure
Nonribosomal peptides range from 2 to 50 amino acids in length and often have a cyclic or branched structure. They contain both “regular” proteinogenic and non-proteinogenic amino acids - D-forms or residues modified by the addition of N-methyl and N-formyl groups, glycosylation, hydroxylation, acylation or halogenation. Cyclization occurs through the formation of oxazolines and thiazolines in the peptide backbone [12].
Synthesis
NRPs are synthesized by non-ribosomal peptide synthetases (NRPS), which do not follow “foreign” instructions in their work, that is, they do without mRNA. NRPS are giant multimodular enzymes, each of which can synthesize only one type of peptide. A separate enzyme module is responsible for the inclusion of one amino acid in the peptide chain; therefore, the number of modules corresponds to the length of the peptide [14].
Each module consists of at least three domains:
- condensing (accepting the peptide chain from the previous module);
- adenylating (selecting the desired amino acid);
- peptidyl (forming a peptide bond).
Modules often include other domains, including the epimerizing domain, which converts L-amino acids into D-forms [14].
By analogy with the triplet ribosomal code for protein synthesis, there is also a non-ribosomal NRPS code, determined by 10 amino acid residues in the substrate-binding pocket of the adenylation domain. The combination of these residues determines which amino acid will be integrated into the peptide by a specific NRPS module. Knowing this code, it is possible to predict the substrate specificity of adenylation domains and even arbitrarily change it by replacing amino acids in the domain [14].
In experiments by German scientists, lugdunin acted not only on methicillin-resistant staphylococci, but also on glycoprotein-resistant, and even on other gram-positive bacteria such as listeria and vancomycin-resistant enterococcus (Table 1).
The minimum inhibitory concentration (MIC) of the new bacteriocin is 1.5–12 μg × ml−1, which indicates the high activity of the substance. However, such concentrations had no effect on human serum, did not cause lysis of neutrophils or red blood cells, and did not inhibit the metabolic activity of monocytes. Bacterial cells exposed to lugdunin at concentrations even below the MIC stopped synthesizing DNA, RNA, proteins and cell wall components. In this respect, lugdunin is similar to daptomycin, which has the same effect, but whose mode of action has not yet been studied. No resistance of S. aureus cells to lugdunin was observed even after they had been grown for a month at low concentrations. Table 1. Spectrum of activity of lugdunin
| Types and strains | Resistance | MIC of lugdunin (μg × ml−1) |
| Staphylococcus aureus USA300 (LAC) | MRSA | 1,5 |
| + 50% human serum | 1,5 | |
| Staphylococcus aureus USA300 (NRS384) | MRSA | 1,5 |
| Staphylococcus aureus Mu50 | GISA | 3 |
| Staphylococcus aureus SA113 | 3 | |
| Staphylococcus aureus RN4220 | 3 | |
| Enterococcus faecium BK463 | VRE | 3 |
| Enterococcus faecalis VRE366 | VRE | 12 |
| Listeria monocytogenes ATCC19118 | 6 | |
| Streptococcus pneumoniae ATCC49619 | 1,5 | |
| Bacillus subtilis 168 (trpC2) | 4 | |
| Pseudomonas aeruginosa PAO1 | >50 | |
| Escherichia coli DH5α | >50 | |
| Legend: MRSA - methicillin-resistant S. aureus; GISA—glycoprotein-resistant S. aureus; VRE—vancomycin-resistant Enterococcus. Table from [1]. | ||
Symptoms
A minimal amount of bacteria in a smear is not a cause for concern. If they begin to reproduce (if conditions are favorable for this), the following symptoms may appear:
- Nervousness and irritability.
- Burning sensation, itching, intensifying at night.
- Vaginal discharge, which may vary in color and smell.
- Pain and discomfort during and after sexual intercourse.
- Increased body temperature, feverish conditions.
- Decreased appetite.
- Pain in the lower abdomen during urination.
- Menstrual irregularities or painful periods with heavy (scanty) discharge.
Symptoms of staphylococcus in a smear in women
If the number of staphylococci detected in a woman’s smear is minimal, then she will not experience any signs of the disease.
However, in the presence of predisposing factors, staphylococci can begin to actively grow, which will lead to the following symptoms:
- Itching in the genital area.
- Discharge of various types, most often with an unpleasant odor.
- Painful sensations during sexual intercourse.
- The impossibility of a full night's rest, as the feeling of itching and burning intensifies at night.
- Increased irritability, nervousness.
- Rashes in the area of the labia minora, similar to pustules, are possible.
However, all these symptoms occur only if the number of staphylococci in the smear is significantly higher than normal. In addition, an overestimation of indicators often serves as a signal that a woman has some kind of sexually transmitted infection. Therefore, it makes sense to undergo a full examination and eliminate the cause of staphylococcus growth in the vagina. As a rule, against the background of growth of coccal flora, there is an increase in the number of leukocytes in the smear, with a minimum content of lactobacilli.
Types of staphylococcal infection
Golden . The most dangerous variety. This type of bacterium, like streptococcus, forms colonies on the mucous membranes and skin. It provokes the development of purulent-inflammatory diseases, produces toxins and coagulase. This pathogenic coccus received its name for its golden color.
Epidermal . Normally, it is present in acceptable quantities on the skin and mucous membranes of every person. But if “gaps” appear in the immunity, then this coccus becomes potentially dangerous. Its intensive reproduction causes serious diseases, including gynecological ones. It can provoke sepsis and endocarditis.
Saprophytic. This bacterium is sometimes called “genital” - based on its location. In the absence of provoking factors, she “behaves peacefully.” If present, saprophytic staphylococcus can have a negative effect on the kidneys and bladder, as well as other pelvic organs.
Hemolytic .
A facultative anaerobe, an opportunistic bacterium that can cause severe damage to the urogenital tract. It got its name because of its ability to destroy blood cells (hemolysis of red blood cells).
Infections caused by staphylococci
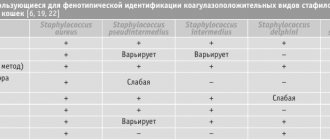
Staphylococci are well known as causative agents of purulent-septic infections in humans and animals. Along with representatives of the Enterobacteriaceae family, they occupy a leading place in the etiology of purulent diseases. The genus Staphylococcus includes 35 different species. Depending on their ability to produce coagulase, the enzyme that causes coagulation of blood plasma, they are divided into two groups: coagulase-positive and coagulase-negative. The habitat of staphylococci is humans and warm-blooded animals, the external environment. Localization in humans: skin and mucous membranes, large intestine. The source of staphylococcal infections is a sick person or a healthy carrier. Routes of transmission: airborne droplets, airborne dust, contact, food. Susceptibility to infection depends on the general condition of the body and age. Children, especially newborns and infants, are most susceptible. Normally, the ability of staphylococcus to invade and the resistance of the host are well balanced, so the infection does not develop until a situation arises when a highly virulent microorganism or a macroorganism with reduced resistance is encountered.
The most famous representative of coagulase-positive staphylococci is S. aureus (Staphylococcus aureus). It occurs in the anterior nasal passages in 20–40% of healthy adults. In approximately 1/3 of the population, it is constantly discharged from the nose, 1/3 has a transient carriage, and 1/3 is free from carriage. S.aureus is most often isolated in purulent pathology and causes a number of diseases: folliculitis, boils and carbuncles, hidradenitis, mastitis, wound infections, bacteremia and endocarditis, meningitis, pericarditis, pulmonary infections, osteomyelitis and arthritis, purulent myositis, food poisoning, syndrome toxic shock. The mentioned diseases are caused by pathogenicity factors: capsular polysaccharides, peptidoglycans and teichoic acids, protein A, enzymes, hemolysins, toxins (exfoliative, enterotoxins from A to E, H and I), superantigen, which belongs to the enterotoxin (TSST-1), causing toxic shock syndrome.
All other coagulase-positive staphylococci are isolated mainly from animals and rarely from humans, but in some cases they can cause purulent-inflammatory diseases in humans.
Among coagulase-negative staphylococci, the most significant in human pathology are S.epidermidis and S.saprophyticus. They can cause urinary tract infections, osteomyelitis, bacteremia, infections in newborns in intensive care units, eye diseases, skin infections, affect heart valves, cause purulent inflammation during operations to replace heart valves with artificial ones, during organ bypass surgery, the use of intravenous catheters, catheters for hemodialysis, as well as for angioplasty.
Currently, microorganisms of the genus Staphylococcus play a leading role among pathogens of nosocomial infections. Until a certain time, penicillin was the main drug of choice in the treatment of severe purulent infections caused by S.aureus. Then strains resistant to this antibiotic began to appear. It turned out that resistance to penicillin was due to the production of the enzyme β-lactamase, which destroys the β-lactam ring in the penicillin molecule. Currently, about 80% of isolated S. aureus strains synthesize β-lactamase. Instead of penicillin, in the case of isolation of penicillin-resistant strains, semi-synthetic penicillins resistant to β-lactamase are used. But since the 80s, strains of S.aureus resistant to this group of antibiotics, in particular oxacillin and methicillin, have begun to emerge. The resistance of such strains is associated with the production of penicillin binding protein (PBP 2a), the synthesis of which in turn is associated with the acquisition of the mecA chromosomal gene by staphylococci. S.aureus strains possessing this gene exhibit resistance to all β-lactam antibiotics, including cephalosporins. S. aureus with the mentioned resistance mechanism are assigned the term methicillin-resistant strains. In some cases, resistance to semisynthetic penicillins may be due to overproduction of β-lactamases. In this case, resistance to semisynthetic penicillins, when determined in laboratory conditions, is characterized as moderate. Methicillin-resistant strains of S. aureus often exhibit resistance to other antibiotics, particularly erythromycin and clindamycin. Due to their spread in a number of foreign countries, vancomycin and teicoplanin are beginning to be used as antibiotics of choice. But already in 1996, the first reports appeared on the isolation of S. aureus strains with moderate resistance to vancomycin (MIC = 8 μg/ml.), and since 2002, strains with high resistance (MIC> 32 μg/ml.). Methicillin-resistant strains are also detected among S.epidermidis, and vancomycetes-resistant strains among S.haemolyticus.
For the treatment of purulent-septic infections caused by staphylococci, therapeutic bacteriophages are currently widely used, both monophages and combined ones, containing races of phages that lyse cells of several types of pathogens. Unlike antibiotics, they do not suppress the growth of normal human symbiotic microflora and do not lead to dysbiosis. However, it must be borne in mind that phages also cause the development of resistance in staphylococci, therefore, before their use, as well as before using antibiotics, it is necessary to check the sensitivity to them in isolated strains of staphylococci.
Indications for examination.
Signs of purulent-septic infection, examination of medical personnel for carriage.
Material for research.
Blood, CSF, pus, wound discharge, breast milk, nasal swabs; washouts from medical equipment and supplies.
Etiological laboratory diagnosis includes
isolation of the pathogen on nutrient media, identification of its DNA.
Comparative characteristics of laboratory diagnostic methods, indications for the use of various laboratory tests.
The technique for isolating the pathogen is now well established.
Microorganisms are quite resistant to environmental factors, so if the selected biological material cannot be immediately used for research, you can use special containers and transport media. The technique for collecting and transporting biological material to the clinical diagnostic laboratory is described in more detail in the preanalytical stages of the study section. As a rule, 3–4 days are enough to isolate the pathogen. An exception is the isolation of staphylococci from the blood. In this case, the success of the technique will largely depend on the correct timing for blood sampling and the presence of antibacterial drugs in the patient’s blood. Identification of a specific DNA fragment of S.aureus, S.epidermidis, S.haemolyticus, S.saprophyticus by PCR is carried out when studying various biological materials.
The results of DNA detection using the PCR method have a qualitative and quantitative format. It is possible to simultaneously detect and quantify the DNA of methicillin-resistant S.aureus and methicillin-resistant coagulase-negative staphylococci. This study is simple and reproducible, which allows optimizing epidemiological surveillance of the spread of methicillin-resistant strains, significantly reducing the time and labor intensity of the study. However, detection of a specific DNA fragment of S.aureus, S.epidermidis, S.haemolyticus, S.saprophyticus by PCR does not allow identifying viable microorganisms, nor determining their sensitivity to antibiotics. Features of interpretation of laboratory research results.
When examining sterile biological material (blood, CSF), the detection of S. aureus in any concentration is of clinical significance. In non-sterile biological material, only high concentrations of S. aureus are of clinical significance, indicating its leading role in the inflammatory process.
Normal vaginal microflora
The composition of the vaginal microflora varies depending on:
- day of the cycle;
- influence of external factors;
- physiological state of the woman (pregnancy, lactation, menopause);
- general health.
It is noteworthy that when submitting a smear for analysis, material is collected from three places: the urethra, cervix and vagina. When conducting a laboratory test, microorganisms that cause inflammation or any disease are identified. The smear rate is average, since the indicators cannot be the same for women of different age groups:
| Microorganisms | Number of colony forming units in 1 ml (CFU/ml) |
| Candida | 104 |
| Ureplasma | 103 |
| Veillonella | 103 maximum |
| Mycoplasmas | 103 maximum |
| Lactobacilli | 107-109 |
| Bifidobacteria | 103-107 |
| Clostridia | 104 |
| Fusobacteria | 103 |
| Propionibacteria | 104 |
| Mobiluncus | 104 |
| Porphyromonas | 103 |
| Staphylococcus | 103-104 |
| Streptococci | 104-105 |
Laboratory staff do not completely write the name of the area from which the biomaterial was taken, but use letter designations: U - urethra, V - vagina, C - cervical canal (cervical area).
Diagnostics
At the slightest suspicion of staphylococcus, diagnostic measures are carried out. Differential diagnosis of staphylococcal infection should be carried out in parallel with streptococcal infection. Now serological methods are used for this.
For example, latex agglutination and a standard coagulase test in a test tube (lasts at least four hours, and if the result is negative, it can be extended for a day). To clarify the diagnosis, the PCR method can be used to identify hidden STIs.
General urine and blood tests are mandatory. Because they make it possible to determine the content and number of leukocytes and cocci in biological fluids. But to determine the pathogen and determine the degree of its resistance and sensitivity to antibiotics, biological material is inoculated on nutrient media.
A urogenital smear is taken by a gynecologist in a healthcare facility. On the eve of the procedure, you should refrain from taking anti-inflammatory drugs and antibiotics.
Patient preparation rules
urogenital smear (female)
Standard preparation conditions (unless otherwise determined by the doctor):
Abstain from sexual intercourse for 2 days.
Refrain from urinating. bile Standard preparation conditions (unless otherwise determined by the doctor):
2 weeks in advance Stop taking antibacterial drugs.
Stop taking any local medications and procedures in the area of biomaterial collection. tonsil smear Standard preparation conditions (unless otherwise determined by the doctor):
Stop taking antibacterial and antimycotic drugs.
2 hours before Do not use on an empty stomach or 2 hours after meals. breast milk Standard preparation conditions (unless otherwise determined by the doctor):
24 hours in advance Stop taking topical antibacterial and antiseptic drugs.
Notes:
Before collecting biomaterial, treat the skin of the nipple and areola with 70% ethyl alcohol.
Express a medium portion of BM from the affected mammary gland into a sterile container, soak the Amis female tampon in it, and place it in the Amis transport medium. It is important to achieve maximum impregnation of the tampon by contacting the BM for 10-15 seconds. Transport in a test tube with Amis medium to the laboratory within 72 hours at a temperature of 20-25 °C. nasal swab Standard preparation conditions (unless otherwise determined by the doctor):
5 hours in advance Stop taking any nasal drops and sprays.
ejaculate Standard preparation conditions (unless otherwise determined by the doctor):
Immediately before the examination, toilet the external genitalia.
Notes:
By masturbation, collect the ejaculate in a sterile container at home, or in ML DILA by appointment: Podvysotskogo, 6A;
Obolonsky Ave., 49; Gagarina, 9. Place the Amis female tampon in the ejaculate until maximum saturation (contact with the BM for 10-15 seconds), place the soaked tampon in the Amis female gel medium. Transport to the laboratory within 72 hours at a temperature of 20-25 °C. tongue swab Standard preparation conditions (unless otherwise determined by the doctor):
do not brush your teeth with toothpaste, do not chew chewing gum.
Do not consume food or drinks. prostate secretion Standard preparation conditions (unless otherwise determined by the doctor):
toilet the external genitalia.
urine Notes:
After thoroughly toileting the external genitalia, collect the middle portion of the first morning urine in a sterile container.
Transfer urine from a sterile container in accordance with the instructions into a transport tube with boric acid preservative (Vacuette Bac tube). Deliver to the laboratory at a temperature of 20-25 °C within 24 hours, in a sterile container within 2 hours. sputum Notes:
Before collecting sputum, brush your teeth, rinse your oropharynx with boiled water, and spit out the saliva. Collect the morning portion of sputum released during coughing into a sterile container from the kit, then according to the instructions, moisten the sterile Amis female tampon in BM for 10-15 seconds and place it in a test tube with Amis female medium. It is important to achieve maximum impregnation of the tampon by contacting it with the BM for 10-15 seconds. Transport in a test tube with Amis medium to the laboratory within 72 hours at a temperature of 20-25 °C.
You can add this study to your cart on this page
Treatment options
If during the diagnosis it is revealed that the permissible number of staphylococci is exceeded, then the optimal treatment regimen is selected for the patient. It is individual for each clinical case and depends on the nature and characteristics of the course of the disease.
Therapeutic measures are not always carried out, because not only the total number of cocci is taken into account, but also their percentage ratio to other strains. At the initial stage, broad-spectrum drugs are prescribed (Lincomycin, Erythromycin, Fuzidin, Novobiocin). But before this, the patient’s allergy history is carefully studied.
The average treatment plan looks like this:
- The use of antibacterial drugs to destroy the main strain of microorganisms and eliminate the manifestations of infection. Without an integrated approach, therapy will not be effective. This means taking pills, douching, using vaginal suppositories (Terzhinan, Vokadin, Pimafucin). Antiseptic solutions can be used to sanitize the vagina: Miramistin, Streptomycin, Chlorophyllipt.
- Search and elimination of pathologies that contribute to the proliferation of staphylococcus. The factors contributing to this are different: starting with non-compliance with basic hygiene rules, and ending with the exacerbation of chronic diseases.
- Restoration of vaginal microflora, for which preparations containing lactobacilli are used.
If the degree of staphylococcal damage is severe, then the patient may be prescribed the following drugs: Vancomycin, Oxacillin, Ampicillin. The course consists of a certain number of days and cannot be shortened or extended on your own initiative.
Treatment for intestinal infection in the uterus
The goals of therapy are:
- elimination of E. coli;
- prevention of chronic inflammation;
- restoration of the menstrual cycle;
- preservation of a woman's reproductive function.
Both acute and chronic inflammatory processes in the uterus caused by an intestinal infection require antibacterial therapy. For symptomatic treatment, painkillers, restorative and immunostimulating agents, and probiotics with lactobacilli are used. Physiotherapy is used to treat damaged endometrium and restore the menstrual cycle.
ethnoscience
Traditional recipes for maintaining immunity
Traditional medicine is powerless in the fight against staphylococcal infection. All drugs prepared according to ancient recipes are considered auxiliary agents. Their use is aimed at strengthening the immune system and removing toxins from the body.
Women who have become victims of staphylococcal infection are recommended to use decoctions of medicinal herbs, consisting of: plantain, licorice root, thyme and string. But propolis tincture, which you can prepare yourself or buy ready-made at a pharmacy, has a special effect. Norm and rules of admission: 1 tsp. alcohol tincture in half a glass of water, three times a day.
Staphylococcus and pregnancy
If a staphylococcal infection is detected in a pregnant woman, a gentle treatment regimen is used. Taking antibiotics is a last resort. Moreover, some staphylococcal strains are highly resistant to antibiotics, which makes treatment with them ineffective.
Most often, pregnant women are prescribed local anti-inflammatory drugs, immunomodulating and immunostimulating drugs, and quartz treatment. Doctors select medications that do not have side effects. And the ideal “weapon” for the fight is the staphylococcus-killing virus - a bacteriophage.
During pregnancy, a woman is especially vulnerable, so staphylococcus easily enters the body, causing various complications. For example, an ascending gynecological infection can provoke peritonitis.
The possibility of infection of fetal tissue and membranes cannot be ruled out. First of all, it affects the kidneys and bladder. Staphylococcus aureus is considered especially dangerous, which often causes miscarriage. This is why pregnant women should get tested regularly.
Cutaneous staphylococcus - treatment
Scientists from the Milner Center for Evolution at the University of Bath have identified 61 genes in staphylococcal skin bacteria that can cause deadly diseases. The samples were taken from patients who had infections following hip or knee replacement surgery and fracture fixation, and were compared with skin swab samples from healthy volunteers.
Surprisingly, even more deadly forms of the bacteria were found in some of the healthy people who took part in the study. Staphylococcus epidermidis has also been found to form biofilms, which increase the body's resistance to antibiotics.
Treatment of cutaneous staphylococcus involves the use of antibiotics. Unfortunately, some antibiotics do not work against some types of cutaneous staphylococcus - the drug resistance of cutaneous staphylococcus is similar to that of Staphylococcus aureus.
For highly drug-resistant strains, vancomycin or teicoplanin are used, which are effective against staphylococci, including methicillin-resistant strains.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter
Prevention measures
- It is not recommended to take antibacterial drugs and douching without the consent of a doctor.
- When diagnosis and treatment are required, care must be taken to select a healthcare facility. Especially if it concerns the reproductive organs. After all, cases of staphylococcal infection due to the fault of doctors are now not uncommon.
- Tampons and menstrual cups are recommended to be used in case of emergency, and it is better to avoid wearing underwear made of synthetic fabrics altogether.
- Protected sexual intercourse, which involves the use of a condom, is protection against unwanted pregnancy, STDs, staphylococcus and other problems.
- It is necessary to take care of the timely treatment of gynecological diseases and neutralization of inflammatory processes.
- Intimate hygiene is an art. All movements are performed from front to back, and not vice versa.
Causes of intestinal infection in the uterus
The microorganism Escherichia coli is a normal inhabitant of the rectum. When E. coli enters the vagina and then the uterine cavity, it causes inflammation. This may happen due to:
- improper washing technique;
- insufficient genital hygiene;
- wearing tight synthetic underwear, thongs;
- combining anal and vaginal sex;
- change of sexual partner.
The penetration and reproduction of E. coli in the uterus is facilitated by low immunity, sudden temperature changes, menopause, and endocrine disorders in the body. Colonization by pathogenic microflora can be associated with douching, long-term use of antibacterial agents, and chronic infections (general and genital infections).
Prerequisites for the introduction of bacteria may include instrumental medical manipulations, curettage, hysterosalpingography, hysteroscopy, insertion of an intrauterine device, and trauma to the birth canal during childbirth.
We have prepared for you a list of studies that will help you deal with this problem:
30 working days
Gut microbiome
12000 ₽
More details