In every person, the larynx is located at the level of the fourth and sixth cervical vertebrae. The paths of the respiratory and digestive systems converge at this point. The larynx borders the pharynx on top, the esophagus on the side, and the trachea on the bottom, forming a kind of “crossroads.”
The larynx consists of several elements:
- Hyoid bone and muscles;
- The lateral part adjacent to the thyroid gland;
- Various paired and unpaired cartilages connected by ligaments, muscles and joints;
- The mucous membrane inside the organ, it is often the target of damage for viruses and other various pathogens (bacteria, fungi);
- Lymphoid tissues that form the laryngeal tonsils.
Each breath, the amount of air necessary for the body passes through the larynx, which then enters the trachea, bronchi and lungs. In addition to participating in the respiratory process, the human voice apparatus is contained in the larynx1.
General information
A common manifestation of respiratory infection in children two to three years old is acute stenosing laryngitis , which is caused by laryngeal stenosis .
Extrathoracic airway stenosis is a narrowing of the trachea outside the chest and larynx. The most common is laryngeal stenosis, which will be the subject of today's consideration. The larynx is an expanded part of the respiratory tube, the upper part of which opens into the pharynx, and the lower part into the trachea. The epiglottis separates the larynx and pharynx. The skeleton of the larynx consists of three large cartilages and three small ones, which are connected by ligaments. The conical ligament is the largest and has clinical significance when performing an operation to dissect it (conicotomy) to ensure airway patency. It connects the cricoid and thyroid cartilage of the larynx. The laryngeal cavity resembles an hourglass and is divided into three sections. The upper, middle (region of the vocal folds) and lower are the subvocal space, which expands downwards and passes into the trachea.
The narrowing can be in any part of the larynx or trachea, it can be partial or complete, but in any case it leads to difficulty in the passage of air. Difficulty in the passage of air through the narrowed sections of the respiratory tract leads to disruption of aerodynamics in the respiratory tract and a person experiences a feeling of lack of air and a constant need to increase the depth of breathing. In children, the subglottic space has a loose submucosal layer, which favors the development of edema and narrowing in this place.
Laryngeal stenosis is most often caused by
laryngotracheitis , foreign bodies , epiglottitis (inflammation of the epiglottis), enlarged adenoids and tonsils. The inflammatory response in the upper respiratory tract most often occurs as a result of exposure to viruses and bacteria, but viruses predominate. If before the beginning of the 20th century the causes of the development of stenosis were bacterial infections ( diphtheria , typhus , scarlet fever ), today these are viral infections, as well as the condition after intubation (post-intubation stenosis).
How to prevent laryngeal stenosis in children and adults - prevention
Prevention of laryngeal stenosis consists of:
- competent and timely treatment of diseases that can cause narrowing of the airways;
- exclude neck injuries;
- timely diagnosis and treatment of upper respiratory tract infections;
- refusal of long intubation (no more than 3 days);
- strict adherence to the timing of tracheostomy;
- observation by an otolaryngologist after laryngeal surgery;
- avoiding inhalation of caustic smoke, ingestion of acids and alkalis into the respiratory tract;
- carrying out allergen-specific and immune therapy;
- avoiding contact with allergens.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Pathogenesis
In the pathogenesis of stenosis, allergic inflammation is important, which occurs with excessive production of inflammatory cytokines, accumulation of immune complexes and release of serotonin and histamine . These phenomena are triggered by the influence of viruses or bacteria. Allergic inflammation occurs with swelling of the larynx, which is accompanied by a reflex spasm - laryngeal stenosis (croup syndrome). At risk for the development of stenosis are children with atopic anomalies ( food allergies , atopic dermatitis , hay fever ), those who are often ill, who are sensitized by previous infections, as well as those who have undergone vaccination.
mucosal ischemia occurs in the pressure zone of the intubation tube. What matters is the trauma to the mucosa during intubation, the shape of the endotracheal tube, the pressure exerted by the inflatable cuff, bacterial inflammation, the duration of intubation, damage to the cricoid cartilage if a tracheostomy is performed, as well as an atypical lower tracheostomy. When the passage of air becomes difficult, oxygen deficiency occurs, which disrupts the functioning of the entire organism. The reaction of breathing to the development of stenosis is to slow down and deepen breathing. Respiratory failure leads to the development of hypoxia and acidosis . Hypoxia does not equally affect the functions of various organs; the central nervous system is primarily affected.
Classification
With the flow:
- Fulminant stenosis (caused by foreign bodies or acute trauma).
- Acute (against the background of burns, laryngeal sore throat , allergic edema ).
- Subacute (with perichondritis and diphtheria ).
- Chronic (occurs with tumors , scar changes, granulomatosis ).
By etiological factor:
- Post-intubation.
- Post-traumatic.
- Paralytic.
By localization:
- Larynx (stenosis of the plica, vestibular, anterior commissural, subglottic, posterocommissural).
- Trachea (at the level of the tracheostomy, above its level and below the tracheostomy).
- Combined (larynx and trachea).
According to the degree of stenosis:
- I degree - the lumen is narrowed to 50%;
- II degree - up to 70%;
- III degree - up to 99%;
- IV degree – there is no lumen in the larynx.
By stages:
- Compensation stage.
- Subcompensations.
- Decompensation.
- Asphyxia.
Acute laryngeal stenosis is accompanied by a sudden suffocation syndrome. Its severity depends on the stage, and with decompensation, delay in providing assistance often leads to death. Acute stenosis is associated with the entry of foreign bodies into the airways, allergic edema , hematoma , post-traumatic edema , immobility of laryngeal structures due to paralysis of the recurrent nerve, as well as external compression of the larynx. Dysphonia is characteristic of laryngeal pathology, but it is not characteristic of tracheal pathology. With tracheal stenosis, the larynx remains motionless, and with laryngeal stenosis, it moves up and down during breathing.
Chronic laryngeal stenosis most often has a post-traumatic origin. One option is a violation of the innervation of the larynx and the associated disorder of the function of its muscles. Most often, this condition develops when the recurrent nerve is damaged during surgery on the thyroid gland. Persistent paralysis of the larynx occurs in 15% of cases after operations and in 30% if repeated interventions were performed. Complete transection of the nerve, as well as its pinching by scars or hematoma, leads to paralysis. Paralytic stenoses also develop with neoplasms of the esophagus. Breathing disorders in chronic stenosis increase slowly, as compensatory mechanisms are gradually activated. Thanks to this, compensation is observed for a long time. Chronic stenosis of the larynx most often occurs in patients who have undergone tracheostomy and also after prolonged artificial ventilation. In this regard, the causes of chronic stenosis are identified:
- Trauma (external, during intubation, fibrobronchoscopy, surgery).
- Outcome of chondroperichondritis (extended intubation, presence of a tracheostomy cannula, burns, infectious diseases).
- Ankylosis of the laryngeal joints.
- Granulomas.
- Neoplasms.
- Compression (internal and external).
- Central and peripheral paralytic stenoses.
- Congenital stenoses.
Causes and course of the disease
The causes of acute laryngeal stenosis can be both general and local in nature, and they are very diverse and numerous.
These include: Local inflammatory diseases - false croup, acute catarrhal laryngitis, acute phlegmonous laryngitis, laryngeal tonsillitis, laryngeal abscess, laryngeal diphtheria;
Non-inflammatory processes in the larynx - foreign bodies of the hypopharynx, congenital defects in the development of the larynx, gunshot wounds of the larynx, as well as mechanical injuries to the larynx, thermal and chemical injuries to the larynx received both at home and at work;
- Infectious diseases of an acute nature - scarlet fever, diphtheria, typhoid, measles, etc.;
- General diseases - pneumonia, heart and kidney disease, syphilis, tuberculosis, allergies to medications, etc.;
- Laryngeal nerve palsy;
- Retropharyngeal abscess and pathological processes in nearby areas;
- Neoplasms in the esophagus and mediastinum;
- Hypertrophic changes in the thyroid gland, which is sometimes called a goiter.
The early stages of development of acute laryngeal stenosis are characterized by the occurrence of hypoxia (acute oxygen starvation) and hypercapnia (carbon dioxide poisoning). Excessive levels of carbon dioxide in the human body leads to excitation in the respiratory and vasomotor centers. Then this causes excessive activity of the inhibitory fibers of the vagus nerve, a drop in pressure and a decrease in heart rate.
Friends! Timely and correct treatment will ensure you a speedy recovery!
Causes
Laryngeal stenosis in children is most often observed with:
- Respiratory infections caused by rhinoviruses, picornaviruses, enteroviruses, coronaviruses, parainfluenza viruses. In children, types 1 and 2 of parainfluenza viruses cause laryngitis with edema and the development of 1-3 degree stenosis (false croup). Adults do not develop croup. The influenza virus multiplies in the upper respiratory tract and the disease occurs in the form of tracheitis .
- Diphtheria . Currently, sporadic cases of diphtheria occur. In Russia in 2015, 2 cases were registered.
- Laryngeal abscess.
- Ingress of foreign bodies. Foreign bodies of the larynx in children pose a great danger to the development of acute stenosis.
- Trauma.
- Allergic reactions. In children with allergic rhinitis, 10% develop recurrent laryngeal stenosis. The tissue under the vocal cords is most vulnerable.
- Acute epiglottitis (laryngeal sore throat). This is a bacterial inflammation of the lymphatic tissue located in the epiglottis area. The epiglottis swells and enlarges, and there are often foci of abscess formation under the mucosa. Sometimes it occupies the entire lumen and a tracheostomy will be required.
- Congenital pathologies (macroglossia - large tongue, micrognathia - underdeveloped jaw).
- Inhalation of vapors of caustic substances.
Laryngeal stenosis in adults is caused by:
- Combined neck injury (gunshot and stab).
- Vagus nerve palsy. In 75-95% of cases, the causes of stenosis in adults are damage to the vagus nerve during operations on the neck organs. Bilateral laryngeal paralysis occurs after strumectomy.
- Long-term artificial ventilation.
- Granulomatous vasculitis (Wegener's granulomatosis). With this disease, necrotizing granulomatous inflammation develops and a subglottic granuloma of the larynx is formed. In the first year of the disease, it occurs in 17% of patients, and with subsequent relapses in a much larger number of patients. In the initial stages, the disease is asymptomatic, but then hoarseness, shortness of breath and constriction are observed.
- Crohn's disease , in which narrowing of the larynx is a typical pulmonary manifestation of the disease.
- Compression by malignant formations.
- Combined treatment of malignant neoplasms of the larynx using chemoradiotherapy. Aggressive treatment destroys tumor cells and adversely affects tissue and cartilage, causing inflammation.
- Laryngeal papillomatosis (benign neoplasm caused by HPV.
Tracheal stenosis is certainly associated with tracheal trauma and nasotracheal intubation. During intubation, standard tubes are used, which do not always correspond to the structural features of each patient. Therefore, there is always a risk of injury to the larynx when passing the tube through the glottis. Excessive pressure in the cuff that secures the endotracheal tube causes mucosal ischemia and increases the risk of tracheal rupture. If a patient undergoes mechanical ventilation for 2-3 days, erosive and ulcerative lesions of the tracheal mucosa occur. When on mechanical ventilation for 4-6 days, laryngitis develops with grade I-II stenosis and ulcerative tracheitis. When the duration of mechanical ventilation is 7 days, combined post-intubation injuries of the trachea are noted. Tracheal intubation through a tracheostomy prevents damage to the larynx. When planning mechanical ventilation for 7 days or more, it is necessary to perform a tracheostomy and it should be performed no later than 3-4 days.
Performing a tracheostomy is also associated with the development of complications, especially when performed on an emergency basis. It is produced quickly and under extreme conditions, which increases the risk of tissue trauma. Fractures of the tracheal half-rings and trauma to the cartilage of the larynx are possible. The installation of a tracheostomy cannula that does not correspond to the size of the trachea, as well as its pressure on the tissue, causes the development of granulation tissue, chondroperichondritis and purulent complications, which themselves cause cicatricial deformities of the larynx and trachea. It is important to note that with tracheal stenosis, the patient’s voice does not change.
Symptoms of laryngeal stenosis
Symptoms of laryngeal stenosis in children include difficulty breathing with a characteristic noise, slow inhalation and exhalation. In acute stenosis, the picture of the disease is pronounced, but in chronic stenosis it is erased and “blurred”, which is associated with the body’s adaptation to hypoxia . In children, this condition develops against the background of a viral infection. The disease develops over several days: against the background of temperature, hoarseness, dry cough are added to the picture of ARVI, and manifestations of stenosis gradually increase: inspiratory shortness of breath (inhalation is difficult and it lengthens), retraction of the intercostal spaces , semi-sitting position, acrocyanosis .
If stenosis develops with the flu, fever and intoxication are characteristic, then a barking cough appears, from which the child wakes up at night, he cannot take a full breath due to severe swelling of the ligaments. With abscessing acute laryngitis, the first symptom is a sore throat, impaired swallowing, and increasing signs of laryngeal stenosis. Signs depend on the stage of stenosis. With compensation, difficulty breathing appears in the child during physical activity, but stenosis does not appear at rest. Breathing also slows down and deepens, and the pause between inhalation and exhalation becomes shorter. Blood pressure may increase and heart palpitations .
In the subcompensation stage, inspiratory dyspnea appears at rest, and breathing becomes stridorous (noisy). When breathing, auxiliary muscles take part: the patient’s wings of the nose “swell,” the subclavian and supraclavicular fossae, as well as the intercostal spaces, are retracted. This is due to an increase in negative pressure in the chest cavity. Patients develop acrocyanosis (blueness of the nose, hands, nasolabial triangle) and tachycardia . The patient is excited, takes a forced position - sits, leaning on the bed and throws his head back.
In the stage of decompensation, cold sweat appears, cyanosis , hands, lips and nose become cold. Breathing is shallow and rapid. There is pronounced stridor breathing, which can be heard at a distance, increased movements of the larynx during inhalation and exhalation, and auxiliary muscles also take a maximum part in breathing. Excitement increases, there is a feeling of fear and confusion periodically appears. The patient's speech is in the form of individual words. The pressure decreases, the pulse has weak filling. Acidosis increases .
The terminal stage is manifested by impaired consciousness, drowsiness and apathy . Breathing becomes very frequent and shallow, and stridor . Periodic breathing is characteristic - breathing alternates with apnea (stopping breathing). Pathological Cheyne-Stokes breathing and gasping breathing (single and rare sighs) develop, which are characteristic of the final stage of asphyxia ( agonal breathing ). The pressure decreases, the pulse is threadlike, arrhythmic, the pupils dilate and death occurs.
In adults, the cause of narrowing of the larynx is its paralysis. Breathing disorders occur with both unilateral and bilateral paralysis. Signs of stenosis appear if the size of the glottis does not correspond to the person’s height, if there is increased weight and a small size of the larynx, as well as deformation in the cervical spine. The severity of the clinic depends on the degree of narrowing and stages.
Manifestations of post-intubation stenosis (stridor breathing and shortness of breath) appear 2-3 weeks after extubation. Symptoms for stenosis of the larynx and trachea are somewhat different.
Differences in shortness of breath. When the trachea is narrowed, exhalation is difficult (expiratory dyspnea), and when the larynx is narrowed, inhalation is difficult (inspiratory shortness of breath). When the larynx is narrowed, the patient throws his head back, and when there is tracheal narrowing, he leans forward and sits, resting against the edge of the bed.
With laryngeal narrowing, the larynx moves up and down during breathing; with narrowing of the trachea, it is motionless.
Hoarseness is present with narrowing of the larynx, but is absent with tracheal narrowing. The voice with narrowing of the larynx does not change with muscle paralysis.
When to see a doctor
If symptoms of laryngeal stenosis are observed in a child, then before taking first aid measures yourself, you must call emergency medical help. Such services are offered by JSC “Medicine” (clinic of academician Roitblerg), located in the center of Moscow. Competent doctors work here. All studies are carried out in the shortest possible time using modern equipment.
First aid from parents in this case may include only non-specific actions. If possible, it is necessary to calm the child (if he is conscious), pick him up or help him take a position in which he is most comfortable breathing. It is important not to panic, so that the child feels supported and confident from adults that everything will end soon and everything will be fine. Under no circumstances should you delay contacting a doctor, otherwise the consequences may be irreversible.
Also, an undoubted advantage of contacting “Medicine” is the presence of highly qualified doctors and experienced medical staff who have many years of experience and always apply an individual approach.
Tests and diagnostics
All patients undergo:
- Clinical blood test.
- Throat swabs for diphtheria.
- For sore throat, throat culture to test the sensitivity of the flora to antibiotics.
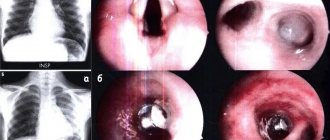
- Laryngoscopy . It evaluates the structure of the larynx, the mucous membrane, the width of the glottis and the mobility of the vocal folds.
- Fibrolaryngotracheoscopy . Examination of the larynx and trachea, which determines the level of narrowing and its degree. Tracheobronchoscopy using an operating microscope reveals cicatricial stenosis. But with degree II–III stenosis, asphyxia may develop when inserting an endoscope if the patient does not have a tracheostomy.
- X-ray tomography . Does not always determine the level and degree of narrowing of the trachea.
- CT scan. A gentle research method is used in patients with difficulty breathing. Research time is 5 seconds. This method became widely used when the use of spiral CT became possible. It identifies tumor, traumatic and inflammatory changes and provides accurate information about the degree of narrowing, its length, diameter above and below the narrowing, detects thickening and compaction of the walls, as well as changes in paratracheal tissue. Cartilage, blood vessels and lymph nodes are examined in more detail. The examination of the larynx is carried out in three modes: with a slight inhalation, pronouncing the sound “and” and performing the Valsalva maneuver. When inhaling, an image of the folds is obtained in the state of their greatest divergence, therefore the width of the glottis is judged. When pronouncing “and,” the vocal folds are brought as close as possible.
- Study of external respiration function.
In children
Acute obstructive conditions in children are common and severe. The most common is stenosing laryngotracheitis, which is often defined by the term “croup”. It is caused by inflammation of the mucous membrane of the trachea and larynx and involvement of the subglottic space. This condition most often occurs between 6 months and 6 years of age. This is a clinical syndrome characterized by a hoarse voice, a rough “barking” cough and difficulty breathing (called stenotic) and increasing respiratory failure.
The development of stenosis in children is associated with structural features of the respiratory tract. First of all, this is hyperplasia of glandular tissue in the pharynx, narrowness of the respiratory tract, secretion of viscous sputum, small volume of muscles in this area, soft cartilage, loose epiglottis. The smaller the baby, the greater the volume of loose connective tissue in the subglottic space, and this increases the swelling of the mucous membrane.
The degrees of croup have been described above and do not differ in adults and children. Croup of grades I-II is treated conservatively in children; grade III requires urgent intubation. Corticosteroids are most effective in the treatment of stenosing laryngotracheitis. Treatment begins with intramuscular administration of dexamethasone , which stops the progression of the process. Subsequently, the child is transferred to inhaled steroids ( Pulmicort ) and inhaled bronchodilators. Nebulizer delivery of medications is optimal for young children. Delivery of the required dose of the drug in a short time (5-7 minutes) provides a quick effect. In young children, a mask is used for the procedure, and from 3 years of age it is recommended to use a mouthpiece, since when using a mask, most of the drug settles in the nasopharynx.
For inhalation, Beclomethasone , Pulmicort , Budenit Steri-Neb , Flixotide , Beclazon Eco and Alvesco . From 6 months it is allowed for inhalation through a nebulizer Budenit Steri-Neb , from one year - Flixotode , which is inhaled through a spacer (device for inhalation), Beclazon Eco is allowed from 4 years, and Alvesco can be used from 6 years. The daily dose of Pulmicort depends on age and is 0.25-1 mg. The drug is prescribed once a day, but at the height of an attack, inhalations are effective 2 times a day every 12 hours. Hormonal drugs are prescribed 15 minutes after inhalation of the bronchodilator, but simultaneous use of two drugs in one chamber of the device is allowed. The duration of treatment with inhaled corticosteroids for croup is 2-3 days. If the stenosis is caused by epiglottitis , an antibiotic ( Zinnat , Zinacef , Ceftriaxone Akos ) must be prescribed.
Other causes of stenosis in children include:
- Congenital synechiae of the larynx is a fairly rare pathology in which there are membranes in the larynx that narrow its lumen. The first symptom of this anomaly is a change in voice - this may be hoarseness or “cock crow”. Small membranes that narrow the lumen by 1/3 do not require surgical intervention. Large synechiae cause stenosis, which requires surgical treatment.
- Connective tissue dysplasia syndrome . In this case, chronic pathology of the musculoskeletal system, as well as internal organs, including the respiratory system, is formed. Children with connective tissue dysplasia very often develop stenosing laryngotracheitis .
- Acquired paralysis associated with injury to the recurrent nerve during surgery. With unilateral paralysis there is only hoarseness without respiratory stenosis, and with bilateral paralysis there are signs of stenosis that require surgical intervention.
- Recurrent respiratory papillomatosis is a common benign tumor at this age. The first symptom is progressive hoarseness, and then stenosis occurs.
- Acquired cicatricial stenosis, which, when completely obstructed, significantly impairs breathing. The main reason for its formation is prolonged nasotracheal intubation, which is performed during operations and extreme situations. Also, scar narrowing can form after a sports and transport injury. Scars are localized in various parts of the respiratory tube, but in 70% of children it is noted in the subvocal part of the larynx.
List of sources
- Ryabova M. A., Ermakov V. N. Acute laryngeal stenoses / A manual for medical students and doctors // St. Petersburg. Publishing house of St. Petersburg State Medical University. — 2008.— 20 p.
- Pogorelova E. I., Pochivalov A. V., Panina O. A., Savenko I. L. / Acute laryngitis in young children against the background of connective tissue dysplasia syndrome // Scientific bulletins of Belgorod State University. Series: Medicine. Pharmacy. 2014. No. 24–1 (195). pp. 71–72.
- Vozgoment O.V. Laryngeal stenosis as a complication of tracheostomy // Difficult patient No. 5, T O M 16, 2021.— p. 54-58.
- Banar I.M. Microsurgery for the elimination of paralytic stenoses of the larynx: Abstracts of reports at the IX Congress of Otorhinolaryngologists of the USSR. November 15–17, 1988, Chisinau. pp. 314–315.
- Bystrenin A.V. Surgical tactics for chronic stenosis of the larynx and trachea // Abstract of thesis. Dr. Honey. Nauk – M., 2003 – 34 p.
Treatment
Patients with acute laryngeal stenosis need emergency treatment and are urgently sent to an ENT hospital. If laryngeal stenosis is in the stage of compensation, then conservative treatment is possible. However, constant monitoring of the patient’s ENT condition is necessary, since surgical intervention—tracheotomy—may be required at any time. Initially, patients are prescribed distraction and degritation (removal of excess fluid) measures. Foot baths, intravenous administration of desensitizing (decongestant) drugs and glucose solution, warm drinks in small portions, and magnesium are indicated. Bromides, antihistamines and corticosteroids that have a sedative effect are prescribed.