The vaginal part of the cervix is covered with flat (cell-shaped) epithelium, which, when examined in a mirror, looks uniform, pale pink. The cells lining the cervical canal (canal of the cervix) are completely different in shape - cylindrical, protruding above the surface, when viewed they look red, and when viewed under magnification they look like grapes. During a gynecological examination, these two types of epithelium are clearly distinguishable. Normally, only squamous epithelial cells are detected on the surface of the cervix; columnar epithelium is not visible, because it is located inside the cervical canal.
There are several different concepts that need to be distinguished.
Erosion
(true erosion) is a disease of the cervix in which there is a defect in the mucous layer covering the vaginal part of the cervix, bright red, irregular in shape, with relatively clear boundaries, easily injured and bleeding. The cause is most often inflammation or injury. Erosive lesions resemble shallow ulcers. Because mucosal cells regenerate (recover) well; erosion usually heals in 5-7 days. Non-healing true erosion is rare and requires observation and treatment. True erosion occurs in approximately 1% of women.
Ectopia
(pseudo-erosion) is a disease of the cervix in which there is a shift in the boundaries between the squamous epithelium located on the surface of the cervix and the columnar epithelium lining the cervical canal to the vaginal part of the cervix. Ectopia occurs in approximately 40% of women and is not a pathology.
And most often it is cervical ectopia that women incorrectly call “erosion.” Let's be correct, etc. Most often, ectopia is detected in women, then we will talk further about this condition.
Due to the occurrence of ectopia, it can be: congenital (the influence of high levels of hormones of the maternal body) and acquired. Acquired ectopia may be associated with:
- infectious factors (early onset of sexual activity, a large number of sexual partners, a history of inflammatory processes in the genital organs);
- traumatic factors (cervical injuries during childbirth and abortion, the use of barrier methods of contraception);
- hormonal imbalance (early onset of menstruation, irregularities in the menstrual cycle and reproductive function);
- changes in immune status (presence of chronic diseases, occupational hazards).
According to the clinical course: uncomplicated form and complicated form (combination with inflammatory diseases of the cervix and vagina).
Prices for services
Initial appointment with a gynecologist + ultrasound (assessment of complaints, medical history, examination in a gynecological chair, pelvic ultrasound, consultation)
Primary appointment – visiting a doctor of a specific specialty for the first time. Make an appointment
1800 ₽
Repeated appointment with the gynecologist
With the exception of repeated appointments with doctors: Blatsios N.D., Dzhashiashvili M.D. Make an appointment
1200 ₽
Ultrasound of the pelvis in women (uterine cavity, ovaries)
Make an appointment
1500 ₽
Types of diagnostics
The doctor can see the pathology visually using a gynecological speculum during an examination on a chair. Ectopia is a red spot of various sizes, with uneven edges. Sometimes the defect may bleed. If squamous epithelium is visible in the area, then the erosion is in the healing stage.
Since ectopia can increase in size and lead to malignant neoplasms, a woman with such a diagnosis must undergo a series of studies.
Types of disease
The disease is:
- congenital – not considered an anomaly;
- acquired – diagnosed for progress
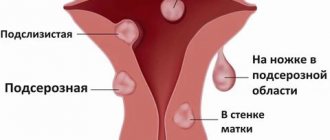
Based on the characteristics of the proliferation of columnar epithelium, the disease is classified into:
- glandular ectopia – characterized by an abundance of glandular structures;
- papillary (papillary) - the cylindrical epithelium is distinguished by the presence of a papule, with a vascular loop at the end;
- epithelizing (healing) - similar to the glandular one, however, the formation has healthy zones of normal flatness. No therapy is prescribed - the normal state is self-healing when the mature squamous epithelium completely replaces the columnar epithelium.
The appearance of cervical ectopia of the cervix makes it possible to establish the characteristics of the epithelial abnormality.
How it manifests itself
Most often, changes in the cervix do not manifest themselves in any way and are detected only during examination, which is why it is so important to undergo regular examinations by a gynecologist. But sometimes there may be:
- Pain and bleeding during sexual intercourse.
- Bloody discharge between periods.
- Bloody discharge during or after examination.
- Nagging pain in the lower abdomen.
- Discharge with a strong unpleasant odor
Such manifestations arise due to the fact that the epithelium of the cervical canal is more susceptible to irritants and is more easily injured.
These symptoms can also occur with other, more serious conditions. Therefore, when they appear, you should definitely contact a gynecologist for an examination, even if nothing else worries you.
Methods of treating the disease
Treatment methods for ectopia are selected according to the characteristics of the disease. Both conservative and surgical treatment methods are used.
If there are no complications, and in case of a congenital anomaly, dynamic monitoring is carried out with annual examinations by a gynecologist, collection of an oncocytological smear and colposcopy.
In case of complications, therapy is developed taking into account the type of epithelial transformation and its causes. To treat an illness caused by an infection, antibacterial therapy is prescribed. For the treatment of hormonal disorders, the gynecologist will select appropriate medications.
Surgical treatments include:
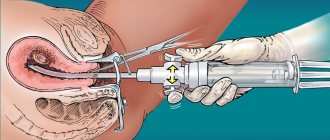
- Diathermocoagulation (cauterization) – destruction of abnormal zones with special electrodes. Afterwards a crust remains, underneath it there is healthy epithelium. When the scab falls off, a scar remains. The procedure is suitable for women who do not plan to give birth;
- Laser coagulation - the laser destroys the columnar epithelium, leaving a thin film of tissue;
- Cryodestruction - abnormal columnar epithelium is removed with liquid nitrogen. A scab remains in place. Healthy tissues are minimally damaged;
- radio wave surgery – preserves tissue elasticity and does not leave scars.
The optimal method for destroying foci of the disease will be determined by the doctor.
What are Nabothian cysts (Ovula Nabothii)?
In the transformation zone, the flat epithelium gradually “creeps” onto the columnar epithelium, “closing” the ectopia. However, the excretory ducts of the glands may become closed, and the mucus they produce accumulates in the form of small cysts. These cysts can be multiple and range in size from 1 mm to 2 cm. Small cysts do not require any treatment. Only large (severely deforming the cervix) and continuing to grow cysts may require opening and evacuation of the contents. But this happens extremely rarely.
Diseases of the cervix include the following:
- Inflammation of the cervical canal (endocervicitis).
- Cicatricial post-traumatic (postpartum or postoperative) deformity.
- Human papillomavirus infection (HPV), including cervical condylomas.
- Cervical intraepithelial neoplasia (CIN) (Other names: dysplasia, dyskeratosis, squamous intraepithelial formation (SIL)) and cervical intraepithelial glandular neoplasia (CIGN).
- Cervical cancer: squamous cell carcinoma or adenocarcinoma.
- Endometriosis of the cervix.
- Polyps and fibroids of the cervical canal.
Read about diagnostic methods (colposcopy, targeted biopsy, cytological and histological studies) and treatment of precancerous diseases of the cervix (laser coagulation, cryodestruction, diathermoexcision, conization of the cervix) in the sections diagnostics, treatment and services.
- Inflammation of the cervical canal - endocervicitis . Most often it is caused by sexually transmitted infections (chlamydia, mycoplasma, gonococci) or nonspecific infections (streptococcus, staphylococcus, E. coli, corynebacteria, enterococcus, etc.). In the first case, infection occurs through sexual contact. The second group of microorganisms enters the cervix most often by lymphogenous (through lymphatic vessels) or contact (from the rectum) route; however, sexual intercourse is not necessary for their development, but can contribute to inflammation. Other provoking factors may be some benign diseases of the cervix (see below), cicatricial deformation of the cervix, weakening of general and local immunity. Endocervicitis is manifested by profuse mucous leucorrhoea, sometimes with an unpleasant odor. Endocervicitis can be one of the causes of miscarriage and premature birth. The disease can be suspected already during a gynecological examination: a large amount of mucus is released from the cervical canal, the transformation zone has a bright pink color. To diagnose the infection that caused the process, the following tests are taken: a smear for the degree of purity, culture for flora and sensitivity to antibiotics, testing for the presence of chlamydia, mycoplasma and ureaplasma (by PCR or culture), sometimes culture on special media to isolate trichomonas, fungus genus candida, gonococcus. Treatment for endocervicitis depends on what infection is causing it.
- Deformation of the cervix occurs due to traumatic childbirth or surgical interventions on the cervix. During labor, the cervix shortens, flattens, and then dilates to a diameter of 10 cm, allowing the fetal head to pass through the mother's birth canal. Sometimes, during the passage of the head, the cervix ruptures. This is facilitated by the following factors: rapid and rapid labor, weakness of labor with early ineffective pushing, inappropriate behavior of the woman in labor during pushing, which is often observed against the background of fatigue and painful contractions, the application of “high” obstetric forceps, a large fetus (weighing more than 4000 grams). ), previous operations on the cervix, including cervical excision, diathermocoagulation of ectopia, etc., ruptures in previous births. Most often, ruptures occur on the sides of the neck (at 3 and 9 o'clock). They can be of several degrees in depth. At the most severe degree, the ruptures reach the vaginal fornix and spread to the body of the uterus. After childbirth, the obstetrician examines the cervix “in the speculum” and, if ruptures are detected, closes them with absorbable sutures. Unfortunately, not all ruptures are diagnosed and carefully sutured. In such cases, the cervix after childbirth is formed defective - the cervical canal often remains gaping, and the cervix itself can take on the most bizarre shapes. If a woman is not planning a pregnancy, then nothing may bother her, and she will only find out about the presence of scars and deformities during the next gynecological examination. However, problems may arise during the next pregnancy - most often, spontaneous abortions (miscarriages) and premature births. There are extremely many reasons for spontaneous abortions, and cervical pathology is not the most common of them. However, cervical insufficiency can be suspected if the miscarriage occurs more than 16 weeks, begins with rupture of amniotic fluid, and there is a history of traumatic birth or cervical surgery. Diagnosis includes a visual examination in a gynecological chair, and, if necessary, cervicohysterography (X-ray examination with the introduction of a contrast agent into the lumen of the cervical canal and the uterine cavity). Treatment is required if a woman suffers from miscarriage due to severe deformation of the cervix. In such cases, surgical treatment is performed - cervical plastic surgery (tracheloplasty). If a cervical deformity is detected during pregnancy in the presence of signs of a threatening miscarriage, a special circular suture is placed on the cervix in order to preserve the pregnancy, designed to compensate for the lost mechanical function of the cervix. This suture usually remains until full term pregnancy. It is removed either on the eve of the expected birth, or in the event of the onset of labor.
- Papillomavirus infection (HPV) , including exophytic condylomas of the cervix.
 In short, you should know that: 1) the development of exophytic condylomas on the surface of the cervix, most often caused by papillomavirus type 6, leads to changes in the mucosa, which can be characterized as a mild degree of dysplasia (see point 4). 2) They themselves do not lead to the development of cancer and precancerous conditions of the cervix. 3) Small condylomas often undergo spontaneous regression (disappear on their own). 4) Oncogenic serotypes of HPV viruses (16, 18, 35, 39, 45) significantly increase the risk of developing severe dysplasia and cervical cancer. Moreover, they are the main cause of the development of these diseases. 5) Oncogenic types of viruses do not cause the development of exophytic condylomas. They are integrated into the genome of epithelial cells and change their genetic properties, promoting gradual cancerous degeneration. 6) Exophytic condylomas of large sizes, as a rule, must be removed (for example, using electrocoagulation, laser, podophyllotoxin preparations, etc.). 7) To date, there are no systemic medications that can reliably cure the papilloma virus. Detection of long-term persistence (preservation in the body) of oncogenic type papilloma viruses is the main risk factor for the development of severe degrees of dysplasia and cervical cancer, therefore, in this case, a particularly thorough and frequent examination of the cervix is required in order to detect the disease in time and adequately treat it.
In short, you should know that: 1) the development of exophytic condylomas on the surface of the cervix, most often caused by papillomavirus type 6, leads to changes in the mucosa, which can be characterized as a mild degree of dysplasia (see point 4). 2) They themselves do not lead to the development of cancer and precancerous conditions of the cervix. 3) Small condylomas often undergo spontaneous regression (disappear on their own). 4) Oncogenic serotypes of HPV viruses (16, 18, 35, 39, 45) significantly increase the risk of developing severe dysplasia and cervical cancer. Moreover, they are the main cause of the development of these diseases. 5) Oncogenic types of viruses do not cause the development of exophytic condylomas. They are integrated into the genome of epithelial cells and change their genetic properties, promoting gradual cancerous degeneration. 6) Exophytic condylomas of large sizes, as a rule, must be removed (for example, using electrocoagulation, laser, podophyllotoxin preparations, etc.). 7) To date, there are no systemic medications that can reliably cure the papilloma virus. Detection of long-term persistence (preservation in the body) of oncogenic type papilloma viruses is the main risk factor for the development of severe degrees of dysplasia and cervical cancer, therefore, in this case, a particularly thorough and frequent examination of the cervix is required in order to detect the disease in time and adequately treat it. - Cervical intraepithelial neoplasia (dysplasia) . This term (CIN) is used to refer to disorders of the maturation and structure of stratified squamous epithelium. Changes are assessed by cytological examination of cell scrapings from the surface of the neck and/or by histological examination of biopsy material. This pathology is associated with impaired cellular differentiation and maturation. There are three degrees of dysplasia: CIN I, CIN II, CIN III. With mild dysplasia (CIN I), cell maturation is impaired in the lower third of the epithelial layer. The top two thirds look typical. With the second and third degrees of dysplasia (CIN II, CIN III), cell maturation is impaired, respectively, in 2/3 or throughout the entire thickness of the epithelium. The next most severe cellular and tissue changes are carcinoma in situ, which translates as cancer “in place,” that is, within the epithelial layer, without growing into the underlying tissue of the cervix.
In turn, CIGN is an analogue of CIN, but refers to columnar epithelium. CIGN is judged by cellular atypia of the epithelial layer. Accordingly, adenocarcinoma in situ is distinguished as the most severe dysplasia. Cells of altered tissue (both squamous and cylindrical epithelium) look atypical, which is confirmed by cytological examination of scrapings from the surface of the cervix (Papanicolau smear). In them, the nucleus is enlarged, it has a lighter color, and the content of cytoplasm in the cell is reduced. In addition to the changes described, blood vessels also acquire a special structure: they come close to the surface, arranged in the form of loops, spirals and other elaborate shapes. This helps distinguish healthy tissue from pathological tissue during colposcopic examination of the cervix.
Cervical ectopia: treatment for nulliparous women
Based on the diagnostic results, the specialist may prescribe drug therapy or surgery.
Conservative treatment in nulliparous patients is carried out at home with the help of various drugs - antibiotics, anti-inflammatory drugs, hormonal therapy, local effects. Drugs and treatment features are individual.
To remove foci of the disease, radio wave surgery is most often prescribed, since it is as safe as possible for future pregnancy and childbirth.
Do you want to cure ectopia? Come to El.En.!
The regimen is selected individually, the gynecologist takes into account the patient’s characteristics, the nature of the changes and other factors. The only thing we can guarantee you with 100% confidence is that by contacting us, you will get an effective result and get rid of a delicate problem.
We employ high-class specialists, doctors with recognized international authority and enormous experience. We use the latest equipment from foreign manufacturers and always take a comprehensive approach to solving the problems of our patients. Therefore, if you have suspicions of ectopia, or it has already been confirmed, come to us, and we will do everything to preserve your reproductive health and restore the opportunity to lead a full intimate life.
Choose a time that suits you and sign up for a consultation by phone or online.
Prevention
There are no special methods of prevention. General recommendations:
- healthy lifestyle;
- good nutrition;
- refusal to frequently change partners;
- pregnancy planning;
- use of contraception;
- timely treatment of inflammatory and infectious diseases of the genitourinary system.
It is important to have preventive visits to the gynecologist once every six months.
Other articles by the author
- Polycystic or polycystic ovary syndrome
- Uterine cancer
- Pelvic pain syndrome
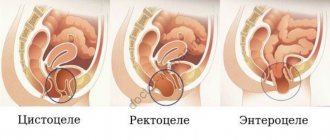
- Stress urinary incontinence
- Ectopic cervix
How to treat
True erosion goes away on its own after eliminating the cause. Therefore, in this case, you need to choose the right treatment regimen. If this is a consequence of an injury, then the erosion will heal without consequences. In case of infection, antibacterial therapy is necessary; in some cases, it is advisable to undergo a histological examination of the cervix and select therapy depending on its result.
The treatment regimen for ectopia will depend on the patient’s age, the size of the changes and the condition of the cervix, as well as on the results of the preliminary examination and the cause of the appearance. But most patients with ectopia only need to be monitored by a doctor.
Ectropion most often does not require treatment, however, with frequent inflammatory processes caused by this condition, a biopsy of the cervix and minimally invasive surgery aimed at restoring its structure makes sense.
Thus, in the vast majority of cases, changes in the cervix, which can be interpreted as erosion, are not such. Therefore, there is no need to carry out “cauterization” if the examination does not reveal indications for surgical treatment.