Pharmacodynamics and pharmacokinetics
According to the instructions, Prazosin has the following effects on the body:
- blocking postsynaptic α1-adrenergic receptors;
- reducing the vasoconstrictor effect of catecholamines;
- decrease in total peripheral vascular resistance and decrease in blood pressure;
- expansion of peripheral veins;
- reduction of afterload on the heart;
- decreased pressure in the pulmonary circulation;
- improvement of intracardiac and systemic hemodynamics in chronic heart failure;
- decreased myocardial oxygen demand and increased stroke volume during exercise;
- decreased renal vascular resistance;
- reducing pressure and resistance in the urethra and reducing the severity of symptoms of urinary tract dysfunction.
Taking the drug may be accompanied by the development of moderate reflex tachycardia. With long-term use, a decrease in the concentration of atherogenic lipids in the blood is observed.
After taking a single dose, the maximum hypotensive effect develops within 1–4 hours. The duration of action of the drug is up to 10 hours. During treatment, early (after 3–5 days) or late (by 12 months) tolerance may develop, so the doctor may decide to increase the dose.
The drug is quickly absorbed from the gastrointestinal tract (food intake does not affect absorption). The maximum concentration in the blood is achieved within 1–3 hours. The bioavailability of Prazosin ranges from 50 to 85%, binding to plasma proteins exceeds 95%. The drug is metabolized in the liver.
The half-life of Prazosin is from 2 to 4 hours. The drug is excreted primarily in bile. In patients with chronic renal failure and elderly patients, the half-life is prolonged.
Pharmacological properties of the drug Prazosin
Selective blocker of postsynaptic α1-adrenergic receptors. Reduces blood pressure, reduces peripheral vascular resistance. IOC, systolic volume and heart rate remain unchanged. Blocks postsynaptic α1-adrenergic receptors of arteries and veins, reducing pre- and afterload on the heart, improves systemic and intracardiac hemodynamics, and reduces pressure in the pulmonary circulation. With long-term use, it reduces the concentration of atherogenic lipid fractions in the blood. Rapidly absorbed when taken orally. The maximum concentration in the blood plasma is reached after 1–3 hours, the half-life is 2.5–4 hours. Approximately 90% of the substance is excreted in the bile, 10% in the urine.
Instructions for use of Prazosin: method and dosage
The tablets should be taken orally. Eating does not affect the effectiveness of the drug.
At the beginning of treatment of arterial hypertension, 0.5 mg is prescribed at bedtime. The dose is gradually increased, first to 1 mg 3-4 times a day, and then until a stable reduction in blood pressure is achieved (usually this takes from 4 to 8 weeks). The optimal daily dose for each patient can vary between 3-20 mg, most often 6-15 mg. The total daily dose is divided into 3-4 doses.
When prescribing Prazosin as a single drug, it is necessary to take into account the possibility of developing tolerance. It is possible at the beginning of treatment (on days 3-5) or after a few months. This phenomenon requires an increase in the dose of prazosin or additional administration of diuretics.
If the hypotensive effect develops slowly or is insufficient, other antihypertensive drugs or diuretics are additionally prescribed. In this case, the dose of Prazosin is reduced to 1-2 mg 3 times a day, a second drug is added, and then the dose is gradually increased again, selecting the most appropriate treatment regimen.
The duration of use of the drug is not limited.
For congestive heart failure, 3-20 mg/day is prescribed in 3-4 doses.
The maximum permissible daily dose for adults is 20 mg.
Alpha blockers: selection for selectivity
Created for patients with cardiovascular disease, alpha blockers have become the most commonly prescribed drugs for urological patients, mainly men with benign prostatic hyperplasia (BPH) and lower urinary tract symptoms (LUTS).
A correspondent for the Urology Today newspaper spoke with Russian and foreign urologists about “evolution and natural selection,” achieving maximum selectivity and the prospects for alpha blockers.
Alpha blockers: maximum uroselectivity
| Alexander Viktorovich Govorov Candidate of Medical Sciences, Associate Professor, Department of Urology, Moscow State Medical University named after. A.I. Evdokimova [email protected] |
Adrenergic receptors are no longer “ghost molecules”, but detailed cellular targets, by blocking which one can delay prostate resection or avoid surgery altogether. And if half a century ago scientists doubted the reality of receptors, now even “subtypes of subtypes” of adrenergic receptors have already been identified and studied, which means it is possible to specifically influence the desired target organs.
Nobel for receptors
“I would be presumptuous if I admitted that alpha and beta adrenergic receptors do exist [...] it seems to be simply an abstract concept to describe the observed effects through molecules of different structures” (Raymond Ahlquist, Perspect Biol Med 1973;17:119 –122).
In the 1940s, while studying the reactions of various organs and tissues to the administration of adrenaline and its analogues, scientists discovered that for these substances, at least 2 types of receptors must be present in the cell, one of which relaxes the smooth muscles of blood vessels, the second stimulates the heartbeat. These ghostly cellular structures were conventionally called alpha and beta adrenergic receptors by Raymond Ahlquist.
In the 1970s, Raymond Ahlquist was close to despair - decades of work did not bring tangible results.
Over more than half a century of research, scientists almost intuitively obtained the first beta-adrenergic receptor blocker and found that the characteristic effects of adrenaline appear even in paralyzed animals - that is, it is not the nervous system that is responsible for adrenaline. All.
True, it is worth noting that it was at this time that “ghost receptors” began to appear “molecular outlines”. Robert Lefkowitz labeled the adrenaline molecule with radioactive iodine atoms and in this way “calculated” the adrenergic receptor in a variety of cellular structures. Using radioactive tracers with beta-blockers and other substances, Lefkowitz's team unequivocally proved that alpha and beta adrenergic receptors really exist, and the intermediate link between the receptor and the executive systems of the cell are G-proteins.
Robert Lefkowitz and Brian Kobilka received the 2012 Nobel Prize in Chemistry for their discovery of G protein-coupled receptors. “About half of all medications […] act through G protein-coupled receptors,” the Nobel Committee noted the importance of work on the study of a huge family of receptors, including alpha-adrenergic receptors.
Alpha blockade
Alpha blockers are substances that interfere with the stimulation of alpha adrenergic receptors by adrenaline-like hormones. In 1975, Marco Caine first used the non-selective alpha-blocker phenoxybenzamine in clinical practice. Just 2 years later, scientists analyzed the results of a randomized placebo-controlled trial and confirmed the therapeutic effect and side effects of the first alpha-blocker in urology.
The advent of alpha blockers has radically changed the management of patients with BPH: clinicians have realized that conservative treatment can indeed be effective. Of course, there were skeptics who were confident that drug treatment could not replace transurethral resection of the prostate, however, many considered alpha blockers a panacea for the treatment of LUTS.
Over time, the enthusiasm subsided, including due to the appearance of undesirable effects on the part of other organs, mainly the cardiovascular system. It was also found that alpha blockers improve LUTS, but do not stop the progression of BPH. It turned out that they do not affect the size of the prostate gland at all, and treatment-related relief of LUTS does not always correlate with the degree of obstruction. In other words, it has become obvious that not only the mechanical component is involved in the pathological mechanisms of LUTS formation in BPH.
“Until the 90s, most experts, including myself, believed that LUTS develop due to an enlarged prostate gland, which leads to a narrowing of the lumen of the prostatic part of the urethra and, accordingly, to impaired urinary passage,” admits Herbert Lepore (Herbert Lepor), who discovered alpha1 and alpha2 adrenergic receptors in the prostate gland.
It is now known that BPH is accompanied by progressive hypertrophy of the bladder wall and changes in the urothelium; There is evidence of changes in the regulation of the urination reflex by the central nervous system. It is now generally accepted that LUTS in BPH are associated both with an increase in the mass of the prostate gland and with changes in the tone of the smooth muscles of the prostate stroma, urethra and bladder neck - the so-called dynamic component.
Alpha1-adrenergic receptors are the main component of the system for regulating tone in the urethra: alpha-blockers eliminate the hypertonicity of the prostate stroma, which occupies most of the volume of the hyperplastic prostate - in this way they neutralize the dynamic component of the occurrence of LUTS.
Receptors in detail
If half a century ago scientists doubted the reality of adrenergic receptors, now even “subtypes of subtypes” of adrenergic receptors have already been identified and studied - the systematic tree turned out to be far from dichotomous. It is now known that the prostate gland contains not only alpha1 and alpha2 adrenergic receptors, but also their subtypes. The alpha1 adrenergic receptor subtypes that play a clinically important role are alpha1A, alpha1B, and alpha1D.
Alpha1A adrenergic receptors provide contractile function of the prostate both in healthy men and in patients with BPH; a decrease in tone caused by alpha1A adrenergic receptors leads to relaxation of the smooth muscle tissue of the prostate gland. Alpha1B adrenergic receptors are present in the prostate in smaller quantities than the alpha1A subtype; They are mainly distributed in blood vessels and play an important role in maintaining blood pressure. Non-selective alpha-blockers affect all subtypes of alpha-adrenergic receptors and, consequently, the tone of blood vessels, the nervous system and smooth muscle cells of the whole body, which causes undesirable effects.
The most reliable way to avoid side effects is to act precisely. That is, do not “shoot sparrows with a cannon,” but use uroselective alpha-blockers that have maximum affinity for the receptors involved in the pathogenesis of BPH.
Selection for selectivity
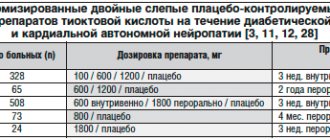
Prazosin is the first short-acting alpha1 blocker; has similar efficacy to phenoxybenzamine and better tolerability. However, side effects associated with the antihypertensive properties of the drug, due to its systemic effect on the smooth muscles of the vascular wall, were problematic. Large multicenter studies on prazosin have never been conducted due to skepticism among urologists in the early 1970s about the possibilities of conservative treatment of BPH.
Alfuzosin, terazosin, doxazosin and tamsulosin (the first alpha-blocker with pronounced selectivity) are approved by the FDA, are present on the Russian market and are recommended by the European Association of Urology (EAU) for the conservative treatment of LUTS in men.
Silodosin is a new uroselective alpha-adrenergic blocker, maximally selective for alpha1A-adrenergic receptors compared to alpha1B-adrenergic receptors (more than 100 times) and alpha1D-adrenergic receptors (more than 50 times). Due to this pronounced uroselectivity, the frequency of side effects should be minimal, and the effectiveness of action on the symptoms of BPH should be similar to widely used alpha-blockers.
Is it so? It seems so. This is evidenced by the results of laboratory and clinical studies. For example, in an experiment with dogs with oral administration of silodosin at a dosage 200 times higher than that in humans, S. Tatemishi et al. (2006) noted no effect on cardiac repolarization. And in a study with volunteers taking silodosin at a dose three times higher than the standard therapeutic dose, there was no significant change in heart rate, pulse or QRS length during electrocardiography (J. Morganroth et al., 2010). High uroselectivity is also evidenced by the results of T. Okura (2002): in rats, after intravenous administration, silodosin persists significantly longer in the tissues of the vas deferens and prostate gland than in the aorta, spleen, heart, lungs, kidneys or blood plasma. S. Murata et al. in 2000 showed that the affinity of silodosin, tamsulosin and prazosin for human prostate cells is lower than for human aortic cells by 214, 8.4 and 0.3 times, respectively.
Considerable experience has already been accumulated indicating the uroselectivity of silodosin, i.e. its high selectivity specifically for the dominant receptors in the prostate - the alpha1A subtype. And although K. Shibata et al. 2 decades ago (1995) showed that the affinity of silodosin for alpha1B adrenergic receptors is more than 500 times lower than for alpha1A adrenergic receptors, the clinical effectiveness of a superselective alpha blocker is still being studied.
It is interesting to note that the affinity of tamsulosin for alpha1B adrenergic receptors is only 15 times lower than that for alpha1A adrenergic receptors. That is, tamsulosin is less selective for prostate tissue than silodosin, but the effectiveness of treatment with both alpha-blockers appears to be similar. In this context, the question of additional benefits of silodosin is interesting. Due to its high uroselectivity, silodosin should have less pronounced side effects on the cardiovascular system, which is especially important for patients in the older age group, in which BPH and LUTS are most common. Regarding the issue of cardiac safety profile, we can cite an interesting experimental study by S. Kobayashi et al. (2009), who assessed intraurethral and blood pressure during therapy with silodosin and tamsulosin in dogs with prostate hyperplasia. Under anesthesia, intraurethral and blood pressure were measured. Silodosin dose-dependently reduced urethral pressure, with virtually no hypotensive effect in dogs of different ages. Tamsulosin had a similar effect on intraurethral pressure, but at the same time reduced blood pressure, much more pronounced in “old” animals than in “young” ones. There are also clinical data. For example, S. MacDiarmid et al. in 2010 showed that simultaneous use of silodosin with sildenafil or tadalafil at the maximum therapeutic dose does not lead to clinically significant changes in blood pressure, heart rate or other manifestations of hypotension.
It is also important that the incidence of orthostatic hypotension when taking silodosin concomitantly with antihypertensive drugs is similar to that when taking placebo. Thus, in a randomized phase III trial, patients simultaneously took silodosin and various antihypertensive drugs: angiotensin-converting enzyme inhibitors (24%), beta-blockers (13%), calcium antagonists (8.7%) and diuretics (7.5%). The incidence of orthostatic hypotension in patients taking silodosin alone (n = 1081) was 1.2%; in those patients who took the above antihypertensive drugs simultaneously with silodosin (n = 500), – 1.4%; in the placebo group – 1% (F. Montorsi, 2010).
Summarizing the data on the clinical and pharmacological profile of silodosin, it is important to once again note the lack of need to adjust the dosage when treating elderly men, as well as the ability to use silodosin simultaneously with phosphodiesterase type 5 inhibitors and antihypertensive drugs.
Side effect of selectivity
It was previously found that ejaculation disorders are more common when taking tamsulosin compared to other alpha blockers, which was associated with the high alpha1A selectivity of the drug. Now we can say that with increasing selectivity, the incidence of ejaculation disorders inevitably increases.
Although the mechanism of ejaculatory disorders remains unclear, young age is considered a risk factor. This side effect, as studies show, is very rarely a reason to refuse treatment.
Not the pinnacle of evolution
Recently, research has been conducted to find superselective alpha blockers. A worthy result in this direction has been achieved, and the topic has to some extent exhausted itself.
In recent decades, the understanding of the pathological mechanisms of LUTS has changed significantly and, accordingly, drugs have appeared that complement alpha-blockers. Perhaps, attempts to combine an alpha blocker with something else in one tablet, for example, with 5-alpha reductase inhibitors, remain promising and interesting. Perhaps there will be medications that combine 3 active ingredients in one (alpha blocker + phosphodiesterase type 5 inhibitor + antimuscarinic drug). It is worth noting that there are already combination drugs on the pharmaceutical market, but they are not yet available in Russia.
What will happen to non-selective alpha blockers? Most likely, they will disappear from the clinical practice of the urologist due to the presence of a large number of side effects. And given the significant duration of treatment for LUTS, patients are interested in managing “less blood” and, as a rule, are independently interested in new therapeutic options. In the future, some new receptors or molecular cascades may be discovered, and accordingly it will be possible to create even more advanced adrenergic receptor antagonists or a completely new class of drugs.
Truly selective alpha blocker
| Herbert Lepore Professor, Department of Urology, New York University Medical Center, USA |
More than 80% of men over 70 years of age develop BPH; The prevalence of LUTS increases from 56% (among men aged 50–79 years) to 70% (among men aged 80 years).
Until the 1990s, transurethral resection of the prostate (TURP) was performed on most men with BPH. Despite the high effectiveness of surgical treatment, the risk-benefit ratio has long remained a problematic issue for patients with moderate manifestations of LUTS.
It is only after the widespread use of alpha blockers that TURP is primarily performed on patients who develop urinary retention or recurrent lower urinary tract infections due to BPH; as well as patients who do not respond to conservative treatment.
Prostate tissue samples, norepinephrine and phenoxybenzamine. This was the “recipe” of the experiment by which Marco Caine showed in 1975 that alpha-adrenergic receptors are involved in the contraction of prostate smooth muscle. Having contracted in response to norepinephrine, the prostate sample “relaxed” after exposure to the antidote, the alpha-blocker phenoxybenzamine. Already in 1976, Marco Kane reported that alpha blockers relax the prostate not only in vitro: the first group of patients with BPH was successfully treated with phenoxybenzamine.
In 1984, Herbert Lepor identified alpha1 and alpha2 adrenergic receptors in the prostate, and in 1988 he showed that it was alpha1 adrenergic receptors that were involved in Kane’s “tricks.” In 1992, Lepore et al published the results of the first multicenter, randomized, placebo-controlled trial on the safety and efficacy of terazosin. “Only 4% and 7% of patients assigned to the placebo and terazosin groups, respectively, were excluded from the 3-month study due to adverse effects,” the author writes. “The results of subsequent studies allowed the FDA to register terazosin as a drug for the treatment of BPH” (ed.).
Currently, alpha blockers are the first line of therapy for most men with BPH and LUTS; 5-alpha reductase inhibitors (dutasteride and finasteride) are the only effective drugs for treating patients with large prostate volume. But since men with “large prostates” also respond to treatment with alpha blockers, even in this group of patients alpha blockers are the first line of therapy.
Non-selective alpha blockers are effective in improving the condition of patients with LUTS, but their use often causes side effects. To date, the FDA has approved 5 alpha-blockers for the treatment of patients with BPH and LUTS: terazosin, doxazosin, tamsulosin, alfuzosin, and silodosin. But only subtype-selective alpha blockers, with equal or greater effectiveness, have a better safety and tolerability profile and do not require dose adjustment. Of all the alpha blockers, only silodosin can be considered a truly selective alpha1A adrenergic receptor blocker.
In in vitro experiments, tamsulosin was almost 10 times more selective for alpha1A adrenergic receptors than for the alpha1B subtype, and 2.5 times more selective for alpha1A than for alpha1D adrenergic receptors. For silodosin, these ratios are 162 and 55, respectively. Due to its uroselectivity, silodosin not only has similar efficacy to tamsulosin, but also safety advantages: adverse effects from the cardiovascular system are minimal.
The only drawback of alpha1A-blockers can be considered ejaculatory disorders, the frequency of which correlates with the effectiveness of treatment and which only in rare cases (3.9%) are the reason for refusal of therapy.
Alpha blockers: science in focus
| Francesco Montorsi Professor, Department of Urology, Vita Salute University, San Rafael Hospital, Milan, Italy |
Alpha blockers are the most effective and accessible group of drugs, mainly prescribed for the treatment of patients with BPH and LUTS. A correspondent for the Urology Today newspaper talked with prof. who needs new alpha blockers and why. F. Montorsi.
Alpha blockade according to urology
Alpha blockers were originally developed to treat patients with hypertension, but over the past 30 years they have become increasingly important in urological practice. In more than 50% of patients, alpha blockers improve the course of LUTS and, accordingly, have a positive effect on the quality of life.
But alpha blockers can be used not only to treat patients with BPH and LUTS. For example, we can talk about the possibility of using alpha blockers for urolithiasis. Currently, there is evidence confirming the effectiveness of alpha blockers in the lithokinetic therapy regimen: when prescribing alpha blockers, the frequency and intensity of renal colic decreases, the likelihood of stone passage increases, and the number of analgesics taken decreases. The use of alpha blockers for urolithiasis is significantly associated with an increase in the rate of stone passage. It is assumed that the observed effects are due to relaxation of the smooth muscle tissue of the ureter with subsequent expansion of its lumen.
It is interesting to note that alpha blockers are considered to have possible antitumor activity, including against prostate cancer (PCa). However, epidemiological data on the relationship between alpha blockers and high-risk PCa are contradictory. According to some published results, the use of alpha-blockers does not significantly affect the risk of developing prostate cancer, tumor progression, or the occurrence of biochemical recurrence of prostate cancer after radical prostatectomy. On the other hand, there is evidence of a higher prevalence of prostate cancer among men taking alpha blockers. However, it is worth noting that alpha blockers, apparently, are not a cause, but some indicator of a high risk of prostate cancer (men using alpha blockers already have changes in the prostate), which the authors of the studies themselves admit (editor's note). ).
Experimental data are also heterogeneous, although they are of significant scientific interest. There is a sufficient amount of data confirming the so-called antitumor activity of alpha1-adrenergic receptor blockers against malignant cells of the prostate gland, bladder, kidneys and other organs, including those not related to the genitourinary system.
In experiments using alpha blockers, scientists observed a decrease in the rate of proliferation and migration of tumor cells, a decrease in the “viability” of cells, an increase in the sensitivity of the tumor to antitumor therapy, and even apoptosis (!). Comparing selective and non-selective alpha blockers, some researchers have come to the conclusion that selective alpha blockers have greater antitumor activity (ed.).
The perfect tablet
Do urologists need new alpha-blockers and drugs for the conservative treatment of BPH and LUTS? Yes, we do! In particular, it is necessary to achieve an optimum in the ratio of effectiveness and long-term action of drugs while maintaining good tolerability and reducing the frequency and severity of side effects. The issue of searching for new alpha blockers is relevant for patients with severe symptoms or a high risk of progression of BPH. In addition, the good safety profile of new, more selective alpha-blockers allows these drugs to be used in a larger group of patients, including for the treatment of men with diseases of the cardiovascular system.
To understand what medications patients need, it is necessary to understand the mechanism of urological disorders. Thus, the development of LUTS is mainly associated with bladder obstruction. The smooth muscle tissue of the prostate gland is controlled by adrenergic nerve fibers, the stimulation of which leads to a significant increase in urethral resistance. Bladder neck obstruction results in an adaptive response of the detrusor to increased resistance to urinary flow due to bladder outlet obstruction. In addition, increased bladder smooth muscle mass also leads to detrusor instability.
Thus, bladder obstruction is an important component of LUTS, determining the severity of the disease. Since alpha-adrenergic receptors determine smooth muscle tone, their blockade has a significant effect on bladder obstruction. However, the severity of LUTS depends both on the severity of bladder obstruction and on compensatory changes in the detrusor. Therefore, we must keep in mind that not only bladder obstruction, but also other factors, such as changes in detrusor muscle fibers, are involved in the pathogenesis of LUTS and influence the severity of its manifestation.
To summarize, it can be noted that the effectiveness of treatment can be improved by addressing both components - bladder outlet obstruction and detrusor overactivity. This means that the ideal drug for patients with LUTS due to BPH should not only reduce the degree of bladder obstruction, but also affect detrusor contractility.
What other problems are relevant for patients and urologists? Since the prevalence of BPH increases with age, there is a high likelihood of concomitant use of alpha blockers and modern antihypertensive drugs. Since non-selective alpha blockers reduce the adrenergic activity of blood vessels, questions remain about the mutual influence of drugs and the manifestation of delayed side effects, which means that the most selective molecules affecting a specific target are needed.
In October 2008, silodosin, a new alpha blocker with a unique selectivity profile, was approved by the FDA for the treatment of BPH. In 2009, it was registered in Europe, and 3 years earlier (in 2006) it appeared in Japan. Due to its unique selectivity for alpha1A adrenergic receptors, the new molecule has minimal effects on blood pressure and the cardiovascular system. Thus, one of the problems - reducing the impact on the cardiovascular system and the likelihood of delayed adverse effects, including with simultaneous use of drugs - has been partially solved by increasing the selectivity of alpha blockers.
Given the complex etiology of the disease, the possibility of increasing the effectiveness of conservative therapy through a combination of molecules, such as alpha blockers and 5-alpha reductase inhibitors, is currently being considered. In addition, the combination of alpha-blockers with phosphodiesterase inhibitors has recently been proposed as a “therapeutic option for the control of BPH”5. To date, positive results have been obtained in these areas (in 2012, the FDA approved tadalafil for the treatment of BPH and LUTS (Editor’s note)), however, further research and observation are needed to verify them.
It is important that the alpha blocker affects one of the most painful symptoms of BPH - nocturia. Silodosin relieves nocturia most effectively of all existing alpha-blockers, which undoubtedly improves the quality of life of patients with BPH.
Superselectivity
Increasing the selectivity of alpha blockers is associated with an increased cardiovascular safety profile. However, there is a problem of additional undesirable effects - in particular, ejaculatory disorders, which can be considered as an unfavorable factor in the treatment of young (!) men.
Previously, it was believed that impaired ejaculatory function is associated with relaxation of the smooth muscles of the prostate gland, urethra and bladder, which, as after transurethral resection of the prostate, leads to retrograde reflux of ejaculate into the bladder. But recently, scientists have found that ejaculation disorders caused by taking highly selective alpha1A-blockers are associated with impaired seminal fluid production. Ejaculation disorders are reversible - it quickly recovers after discontinuation of the selective alpha blocker. In no more than 4% of patients, ejaculatory disorders cause discontinuation of treatment.
I believe that, given its good safety profile, silodosin can be considered as the drug of choice, especially for patients with pathology of the cardiovascular system.
5
Your rating: No Average rating: 5 (1 vote)
Side effects
- From the central and peripheral nervous system: headache, weakness, vertigo, sleep disorders, emotional disorders, hallucinations, anxiety, perception disorders, depression, fatigue, paresthesia;
- From the cardiovascular system: anginal pain, shortness of breath, tachycardia, palpitations, arterial hypotension (especially orthostatic); with long-term use – swelling of the lower extremities; rarely – orthostatic collapse (usually after taking the first dose);
- From the urinary system: frequent urination;
- From the digestive system: diarrhea or constipation, nausea, vomiting, dry mouth;
- From the senses: blurred vision, darkening of the eyes, hyperemia of the cornea and conjunctiva, tinnitus;
- Allergic reactions: skin rash, itching;
- Other: hyperthermia, nasal congestion, hyperhidrosis, arthralgia, nosebleeds, the appearance of antinuclear factors, alopecia, decreased potency, priapism.
Drug interactions
Prazosin is incompatible with nifedipine. Its effect is enhanced by sympatholytics, diuretics, and beta-blockers.
With the simultaneous use of beta-blockers, angiotensin-converting enzyme inhibitors, calcium channel blockers, the risk of severe arterial hypotension increases, especially after taking the first dose of prazosin.
The vasodilating effects of calcium channel blockers and alpha-blockers may be synergistic or additive. With simultaneous use of prazosin with verapamil, the development of severe arterial hypotension is partly due to their pharmacokinetic interaction: the maximum concentration increases and the total concentration of prazosin increases.
Indomethacin may reduce the effect of prazosin.
Prazosin promotes a rapid and significant increase in plasma digoxin levels and may alter the antihypertensive effect of clonidine.
Patients receiving propranolol are at risk of developing severe hypertension after the first dose of prazosin.