Atrial flutter - this is another form of atrial fibrillation in which very frequent, from 200 to 400 times per minute, contraction of the atria occurs, and the rhythm of contractions is not disturbed. In their symptoms, atrial fibrillation and atrial flutter are very similar to each other, however, they have different characteristics. Thus, atrial flutter is characterized by greater resistance to any antiarrhythmic drugs and stronger persistence of paroxysms. There are several forms of atrial flutter: The correct form is when on the ECG the P waves are inverted in the aVF, II and III holes, and in the aVF lead they are directed upward. Irregular shape is when on the ECG the P waves have an unusual shape, in the aVF, II and III holes are directed upward, and the VR lead is inverted. And left atrial flutter, when P-waves are recorded in leads aVF, II and III as a negative wave and in aVR, V1 as a positive one.
Causes of atrial flutter.
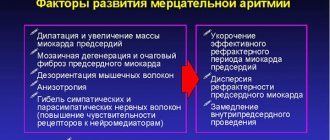
The most common cause is various types of disorders of the impulse conduction system due to the following diseases: - rheumatism (especially in the presence of mitral stenosis ( - coronary heart disease, - acute myocardial infarction, - arterial hypertension, - acute or chronic cor pulmonale, - idiopathic cardiomyopathies, - hyperthyroidism, - pericarditis, - myocarditis, - nonspecific chronic pulmonary diseases, - obstructive chronic pulmonary diseases, - atrial septal defect in adults, - WPW - syndrome (ventricular pre-excitation syndrome) - SSSU (sinus node dysfunction) or also called tachy syndrome - brady, - pathological (atypical) desympathy of the atria, - idiopathic variants. Pathogenetic significance of atrial flutter. The main pathological factor is the excessively high frequency of atrial contractions and all the resulting symptoms. Against the background of developing tachysystole, contractile diastolic dysfunction of the myocardium appears in the region of the left ventricle, which subsequently develops into contractile systolic dysfunction. Ultimately, this picture can develop into dilated cardiomyopathy and result in heart failure.
Symptoms of atrial flutter.
There are two forms of the disease: paroxysmal, that is, paroxysmal and constant. From here, two clinical pictures are distinguished:
Paroxysmal form of atrial flutter. With this form of the disease, the frequency of paroxysms, that is, attacks, ranges from one per year to several per day. The peculiarity of paroxysmal atrial flutter is that there is no age or gender category. Attacks can occur in both men and women of any age. But of course most often in people with myocardial disease. Paroxysms can occur against the background of physical or emotional stress, overeating, drinking alcohol, with a sharp drop in external temperature (immersion in cold water, going outside in winter, and so on) and even when drinking large amounts of water or stomach upsets. The patient often describes an attack of atrial flutter as a feeling of strong and rapid heartbeat that appears after some event or action. In more severe cases, dizziness, weakness, loss of consciousness and even short-term cardiac arrest are observed during an episode of atrial flutter with high-frequency conduction in the AV node (1:1). Persistent form of atrial flutter. This is a very dangerous form, since in the first stages of the development of the disease it is usually asymptomatic and manifests itself with the accumulation of consequences of a decrease in systemic blood output and arterial systemic pressure, which ultimately leads to a decrease in coronary blood flow. Typically, patients come to the doctor with already severe symptoms of heart failure.
Symptoms of arrhythmia
- Feeling of interruptions and sinking heart.
- Palpitations, “fluttering” in the fingertips.
- Pain in the heart area.
- Dyspnea.
- Edema.
- Increased fatigue.
- Fear.
- Presyncope and fainting.
- Sleep disorders.
Children may have a delay in the rate of psychomotor development, tearfulness, and chest deformation.
Children experience vomiting, anxiety, shortness of breath, refusal to eat, and cold sweat. In some cases, arrhythmias are signs of life-threatening conditions:
- arrhythmic collapse or shock;
- heart failure;
- myocardial ischemia (acute coronary syndrome);
- sudden cardiac death.
Diagnosis of atrial flutter.
— An ECG is performed to determine arrhythmia. — Holter monitoring allows you to determine paroxysmal atrial flutter, the causes of the attack, track the work of the heart during sleep and determine the strength of paroxysms. — Ultrasound examination of the heart (EchoCG) allows you to determine the condition of the valves, the contractile activity of the myocardium and the size of the heart chambers. — A blood test will help identify the cause of atrial flutter. For example, with potassium deficiency, thyroid dysfunction, and so on. — In some cases, it is necessary to conduct an EPI (electrophysiological study) of the heart. Treatment and secondary prevention of atrial flutter, in fact, like primary prevention, is practically no different from the treatment of atrial fibrillation. Complex therapy is always carried out, which is based on eliminating the root cause of the development of atrial flutter and situations leading to paroxysms. A diet excluding salty, smoked, spicy and fatty foods must be prescribed. You will have to give up alcohol and cigarettes forever and generally switch to a healthy lifestyle. Drug treatment is prescribed exclusively by a doctor. You should be especially careful when stopping paroxysms and use only those medications prescribed by your doctor. Forecast. The prognosis for treatment is generally similar to that for atrial fibrillation.
Urgent consultation with a cardiologist
Treatment tactics
- Drug therapy is the prescription of special drugs to relieve attacks of arrhythmia and prevent their occurrence.
- Radiofrequency ablation is a minimally invasive surgical treatment for cardiac arrhythmias. The procedure begins with constructing an electrical model of the atrium and determining the localization of sources of pathological excitation. During the intervention, a catheter is inserted through the patient's femoral vein into the atrium cavity. Electrical isolation of the pulmonary veins is then performed using catheter radiofrequency lesions. The procedure is performed under local anesthesia and takes about two hours.
Radiofrequency ablation (RFA)
When a person has an abnormal pulse and develops arrhythmia as a result of a number of cardiovascular diseases, he needs to undergo a comprehensive examination. Doctors often recommend using the catheter ablation method, that is, RFA of the heart. They made this choice largely due to the wide list of advantages of the technique with a minimum number of disadvantages. Therefore, this heart operation is considered one of the best.
It involves neutralizing cells that cause rhythm disturbances with electric current. The latter's access to the heart is provided by a catheter. The operation is not surgical and is considered minimally invasive. It is performed under local anesthesia.
The source of arrhythmia is destroyed using high-frequency (or radio frequency) current of 400-500 kHz.
Supraventricular arrhythmia
Atrial fibrillation and atrial flutter is one of the types of supraventricular arrhythmia. The most common symptoms include rapid heartbeat, shortness of breath, and even fainting. The best results are achieved by combining pharmacological treatment with diagnostic procedures. Supraventricular cardiac rhythm disturbances are caused by electrical impulses originating in the sinus node or atrioventricular focus.
Supraventricular arrhythmia - types
Supraventricular arrhythmias include:
- additional, single stimulation,
- supraventricular tachycardia,
- pre-excitation syndromes,
- atrial tachycardia,
- atrial fibrillation,
- atrial flutter,
- sinus tachyarrhythmias.
Supraventricular arrhythmia - symptoms
Each of the arrhythmias listed above has different causes and symptoms. Each of them is treated differently. First of all, it is necessary to determine what diseases cause supraventricular arrhythmia, what symptoms accompany it, what is the patient's prognosis and how to treat it. Symptoms that are typical of supraventricular arrhythmia include:
- cardiopalmus,
- fatigue,
- dyspnea,
- fainting,
- dizziness,
- chest discomfort.
There are often no symptoms with supraventricular accessory beats.
Types of arrhythmias
There are many types of arrhythmias, as well as divisions in medicine depending on the accepted classifications. The most common forms of cardiac arrhythmia include:
- sinus tachycardia,
- bradycardia,
- atrial fibrillation,
- ventricular fibrillation,
- additional supraventricular and ventricular contractions,
- tachycardia: supraventricular and ventricular.
Each of these disorders is actually a separate disease that has different causes and also requires different treatments.
Definition
Heart flutter is a generalized colloquial definition of one of two pathological conditions.
- Flutter of the ventricles of the heart.
- Atrial flutter.
Ventricular flutter is a life-threatening condition in which the heart is unable to pump blood through its vessels. It is accompanied by loss of consciousness, rapidly increasing symptoms of tissue hypoxia, and without immediate resuscitation, it leads to death within a few minutes.
Therefore, in general practice, heart flutter is most often understood as atrial flutter.
Atrial flutter (AFL) is a cardiac arrhythmia characterized by a rate of 240–400 beats per minute, usually with some degree of atrioventricular (AV) node conduction block. In the most common form of atrial flutter (typical AFL), electrocardiography (ECG) shows a negative sawtooth pattern in leads II, III, and aVF.
Typical (or classic) AFL involves a single reentrant circuit with activation of a circle in the right atrium around the tricuspid annulus. The front of an electric wave most often propagates counterclockwise. Atypical TP occurs according to a different pattern. It may involve the right or left atrium.
TP is associated with a variety of heart diseases. In most studies, approximately 60% of patients with atrial flutter have coronary artery disease (CAD) or hypertension; 30% do not have heart disease. Unusual forms of atrial flutter were noted during long-term follow-up in 26% of patients with surgical correction of congenital heart defects.
Symptoms in patients with AFL usually reflect decreased cardiac output as a result of increased ventricular rate. The most common symptom is rapid heartbeat. Other symptoms include fatigue, shortness of breath and chest pain. An ECG is important for making a diagnosis. Transthoracic echocardiography (TTE) remains the initial imaging modality of choice for the evaluation of AFL.
In this condition, it is very important to control the ventricular response rate or return the patient to sinus rhythm. First, immediate electrical cardioversion is considered for hemodynamically unstable patients. Catheter ablation remains the most appropriate therapy for patients with typical AFL if they meet the contraindication criteria.
Atrial flutter is similar in many ways to fibrillation (underlying disease, pathological factors, complications and treatment). Some patients even experience both flutter and atrial fibrillation. However, the underlying mechanism of AFL makes this arrhythmia amenable to treatment with percutaneous catheters.
Symptoms and accompanying manifestations
Symptoms in patients with AFL usually reflect decreased cardiac output as a result of increased ventricular rate. At the same time, contrary to popular belief, the feeling of “heart fluttering” does not occur. A condition that some patients tend to describe as “heart fluttering” occurs with paroxysmal ventricular tachycardia.
Typical symptoms of TP include:
- dizziness;
- fatigue or poor exercise tolerance;
- slight shortness of breath;
- pre-fainting state.
Less common symptoms include angina, severe shortness of breath, or fainting resulting from poor left ventricular function. With this arrhythmia, thromboembolic phenomena are possible.
In addition, patients may have symptoms of conditions that cause AFL. They may be non-cardiac (such as hyperthyroidism or lung disease) or cardiac.
Often, arrhythmia in these conditions occurs under the influence of provoking factors - alcohol, pneumonia, acute myocardial infarction and surgical procedures. Stimulants such as ginseng, cocaine, ephedra or methamphetamine can also trigger an attack.
For AFL lasting more than 48 hours, anticoagulation with warfarin or transesophageal echocardiography is necessary to exclude left atrial thrombus before cardioversion to sinus rhythm.
The AFL rhythm itself is unstable and usually reverts to either atrial fibrillation or sinus rhythm.
Remaining stable chronic AFL is uncommon, but possible. A history of preexcitation syndrome (Wolf-Parkinson-White) puts the patient at risk for 1:1 flutter waves, which can cause ventricular fibrillation and death.
Patients who are simultaneously diagnosed with new-onset rapid atrial fibrillation or atrial flutter and decreased left ventricular ejection fraction tend to have a high incidence of left atrial appendage thrombus.
Classification and mechanism of occurrence of disorders
In humans, the most common form of atrial flutter (typical) involves a single reentrant circuit with cycle activation in the right atrium around the tricuspid annulus (most often in a counterclockwise direction) with a region of slow conduction located between the tricuspid valve, the annulus, and the coronary sinus ostium (sub-Eustachian isthmus).
Typical counterclockwise atrial flutter has caudocranial activation (counterclockwise around the tricuspid annulus when viewed on a left anterior oblique fluoroscopic image) of the interatrial septum.
A typical AFL may also have a reverse activation sequence (clockwise around the tricuspid annulus). This option is much less common. When electrical activity moves clockwise, the electrocardiogram (ECG) will show positive flutter waves in leads II, III, and aVF, and they may appear somewhat sinusoidal. This arrhythmia is still considered to be a typical isthmus-dependent flutter. It is usually called reverse typical TP.
Atypical AFL is less studied and electroanatomically characterized. It can happen:
- from the right atrium as a result of surgical scars;
- from the left atrium, in particular from the pulmonary veins (focal entry site);
- from the mitral ring.
Left atrial flutter is a common complication after linear ablation procedures (for atrial fibrillation).
How does arrhythmia occur?
To understand the mechanism of arrhythmia, it is necessary to recall basic information about the structure and function of the heart in the body. This organ consists of two atria and two ventricles, which contract and relax in a strictly defined rhythm. Thanks to these movements, blood is constantly pumped into every cell of the body, providing it with nutrients and oxygen. But what makes the heart beat so regularly? The heart is equipped with a natural "pacemaker", that is, the sinus node, located in the right atrium. It is thanks to him that the heart “beats” even when it is removed from the chest. The sinus node produces electrical impulses that move the entire muscle. The work of the heart is a series of complex bioelectrical processes that occur in each of its cells. Cardiac arrhythmias occur when abnormalities occur at some point in this complex process. The pulse source may fail or problems may arise at the conduction stage. In both cases, arrhythmia will occur.
What tests should be taken for ventricular arrhythmia?
To correctly identify ventricular arrhythmia and accurately differentiate the type of ventricular arrhythmia, it is necessary to perform an ECG. If arrhythmia occurs intermittently, perform a Holter test (24-hour ECG recording). You can also monitor your heart rate for longer, such as three days or even 2-3 weeks. In this case, it is necessary to wear an Event-Holter device, which the patient activates only when symptoms appear, such as:
- cardiopalmus,
- deterioration of health,
- dizziness.
An invasive electrophysiological study is performed when the site of ventricular arrhythmia is identified and an attempt is made to destroy the arrhythmogenic focus. The following methods are used in the treatment of ventricular arrhythmias:
- antiarrhythmic drugs,
- percutaneous high-frequency ablation,
- implantation of a cardioverter-defibrillator.
The doctor decides what treatment to take when he determines what type of ventricular arrhythmia the patient has.
Treatment of supraventricular arrhythmias
First of all, it is important to have a detailed history of not only heart disease, but also general, rheumatological, metabolic and endocrine diseases. This usually starts with non-invasive tests such as: morphology, ECG, cardiac ECHO and Holter study. If necessary, invasive and complex tests such as electrophysiological studies are performed. Supraventricular arrhythmias are usually treated with medications. When this doesn't work, you can introduce ablation, for example. These two treatments can also effectively complement each other.
The article is for informational purposes only, self-medication is not acceptable. Be sure to consult with your healthcare provider.