The role of sex hormones in the female body
The content of the article
Puberty, the menstrual cycle, pregnancy, menopause or in general: health and beauty - all these processes and conditions depend on the specific level and constant fluctuations of female sex hormones. They are responsible not only for appearance, characteristic female features or reproductive abilities, but also for many other important processes occurring in the female body.
Hormones can either improve or worsen the condition of your skin and hair; positively and negatively influence overall well-being; increase or decrease libido and finally promote or hinder pregnancy and are responsible for various diseases.
For a woman's body to function effectively, it needs a stable hormonal balance. This is why it is so important to know the functions of individual female hormones, familiarize yourself with their standards, testing forms, and options for monitoring the correct concentration in the body.
Learn what names like estrogens, progesterone, androgens, and prolactin mean, and find out what these hormones do in the body.
Female sex hormones are the culprits of a long-term hormonal storm
You could say that hormones control your entire life. Although this is a simplification of the concept, it is no different from the truth. The endocrine system is complex and is responsible for a number of functions in the human body, and overall it directly influences hormonal balance. Therefore, the endocrine system is often tested first when symptoms, both physical and mental, are present.
Women who, both at puberty and throughout their adult lives, are constantly influenced by hormonal fluctuations can tell a lot about this. After all, female sex hormones are primarily to blame for emotional breakdowns, headaches and other unpleasant situations.
Hormonal fluctuations
How to identify female hormones among common hormones and distinguish them from male ones?
It’s worth starting with what sex hormones are in general.
Sex hormones, also called steroid hormones, are secreted mainly by the female and male gonads, ovaries and testes, respectively, with the participation of the pituitary gland, hypothalamus and adrenal glands.
Already at this stage, it can be noted that sex hormones are produced in both the female and male bodies. Whether we call them female or male depends primarily on their concentration in the body of both sexes and on the performance of certain roles. And it is the level of these sex hormones that determines the development of all broadly understood male and female characteristics.
Hormones influence, among other things, a woman's or man's appearance and the proper functioning of the reproductive system (male and female), as well as numerous processes occurring in the human body.
Among female sex hormones, the most important are:
- estrogens,
- progesterone,
- prolactin,
- androgens.
In addition to the above, gonadotropic hormones must also be present, that is, FSH (follicle-stimulating hormone) and LH (lutropin). It is worth adding thyroid hormones to this set, including triiodothyronine (T3), thyroxine (T4) and calcitonin (CT).
Female hormones are primarily responsible for:
- puberty and the development of specific feminine qualities, including body structure,
- adequate ovarian function and their decline during menopause,
- regulation of the menstrual cycle,
- pregnancy and its proper course,
- metabolism,
- proper blood clotting,
- well-being, which is often associated with changes in mood and a range of different emotional states, and sometimes with mental health,
- calcium deposition in the skeletal system,
- libido, that is, the feeling of sexual desire,
- proper functioning of the sebaceous glands, which also affects the quality of skin and hair,
- lipid metabolism and many other processes.
Each of the hormones performs specific functions, but they are closely related to each other, which is why it is so important to maintain hormonal balance at the desired level.
Thyroid hormones
Thyroid hormones are components that are synthesized by the thyroid gland. They take part in various physiological processes of the body. They contain an iodine component.
Thyroid hormones are:
- Free thyroxine, triiodothyronine.
- Total thyroxine, triiodothyronine.
- Thyroxine-binding globulin and thyroglobulin.
The thyroid gland also produces calcitonin and parathyroid hormone, these substances control the process of calcium metabolism.
Thyroid hormones stimulate growth and development of the body, affect the heartbeat, and help remove excess fluid from the body. They affect physical and mental work, and also stimulate metabolism.
The ovaries contain receptors that respond to thyroid hormones. Thanks to them, the growth of follicles is stimulated, the production of progesterone and estrogens is enhanced.
These substances help reduce the production of glycogen and fat deposits. A large amount of thyroid hormones slows down protein metabolism, and a low concentration of these substances promotes protein synthesis. A thyroid hormone test can determine the presence of thyroid disease.
Estrogens, or hormones of femininity, not only from the point of view of beauty and figure
It is likely that no sex hormone other than progesterone is associated with femininity as strongly as estrogens. It is estrogens that have a huge impact not only on the development of female sexual characteristics, but also on many key processes in the female body.
Estrogens are actually a group of hormones that include the following compounds:
- estrone,
- estradiol,
- estriol,
- esthetrol (produced only during pregnancy).
In women, these hormones are produced mainly in the ovaries, more precisely in the Graaffian follicles, as well as in the corpus luteum or placenta. They are produced in smaller quantities in other parts of the body, such as the adrenal glands, liver, breast glands and fat cells.
The most important functions performed by estrogens in the female body include influencing the development of sexual characteristics already at the level of fetal development, immediately after birth and during adolescence. This means that these hormones are responsible for the typical female body structure and entire figure, the development of the genital organs, mammary glands or redistribution of fatty tissue, as well as the development of the psyche and sexual desire.
In addition, estrogens, including:
- regulate the menstrual cycle and fertility,
- have a positive effect on lipid metabolism, increasing the level of “good” cholesterol (HDL) and reducing con (LDL),
- increase calcium deposition in bones, stimulating their growth; thus preventing osteoporosis,
- accelerate metabolic processes,
- increase vaginal hydration,
- increase blood clotting,
- have a positive effect on protein absorption,
- influence the growth of adipose tissue and its metabolism,
- are responsible for the appropriate level of libido,
- affect the emotional state,
- increase the excitability of the smooth muscles of the uterus and fallopian tubes,
- responsible for converting carbohydrates
- stimulate the functioning of the mammary gland,
- regulate body temperature,
- influence the proper permeability of cell membranes,
- increase skin elasticity and reduce sebum secretion.
The physiological role of estrogens is especially important in certain phases of the menstrual cycle. They are responsible for the growth of the lining of the uterus (endometrium), its proper blood supply and nutrition, thereby preparing it for implantation of a fertilized egg.
This is directly related to fluctuations in estrogen levels during certain periods of the menstrual cycle. The lowest value is observed during menstrual bleeding followed by a gradual increase until it reaches a peak during ovulation. Without this process it would be impossible to get pregnant or maintain a pregnancy.
Estrogens also play an important role in the production of luteinizing hormone (LH), which is involved in ovulation and is responsible for the formation of the corpus luteum.
These hormones make it easier to obtain a fertilized egg and then help the fetus grow and develop. But during pregnancy itself, estrogens also affect:
- development of milk ducts in the mammary glands,
- breast enlargement and figure rounding,
- improvement of skin and hair condition,
- awakening the maternal instinct.
Breast enlargement
During pregnancy, estrogen levels gradually increase. After childbirth, it drops sharply, which may be associated with a significant decrease in the mood of the young mother (the so-called blues, which may be associated with postpartum depression).
A decrease in estrogen is also directly related to menopause. During this period, the hormonal activity of the ovaries ceases, which leads to a significant decrease in estrogen production. As a result, typical menopause symptoms appear and the risk of osteoporosis and heart disease increases.
Male gonad: testicle
The male reproductive gland - the testicle - is a paired organ that produces male reproductive cells - sperm - and male sex hormones - androgens. During the prenatal period, the testicle develops in the abdominal cavity, and towards birth it moves into the scrotum, passing through the inguinal canal - a gap in the lower part of the anterior wall of the abdomen. The scrotum is a kind of skin pocket, the temperature inside of which is slightly lower than body temperature (this is necessary for the formation of sperm).
During the descent of the testicle, deviations may occur, as a result of which one or both testicles may stop in the abdominal cavity or inguinal canal. This delayed descent of the testicles is called cryptorchidism (from the Greek kryptos - hidden - and orchis - testicle). The descent of the testicles should be completed before the age of 7 years, since it is at this age that the seminiferous tubules form in them. Until the testicle is in favorable conditions - in the scrotum, sperm are not formed in it, but sex hormones can be produced.
The testicle is oval in shape, flattened laterally; its length is about 4 cm, width 3 cm, weight 25–30 g. The outside of the testicle is covered by a dense membrane, which is thickened at the posterior edge. From it, septa extend into the testicle, dividing the testicle into lobules, the number of which reaches 300. Each lobule consists of convoluted seminiferous tubules. It is in them that sperm are formed. Then, through a network of other tubules, the sperm are sent to the epididymal duct, where they finally mature. The total length of all testicular tubules reaches 300–400 m.
Spermatogenesis The process of sperm formation - spermatogenesis - lasts about 64 days in humans. The formation of sperm begins when the body reaches puberty. During puberty, a lumen appears in the convoluted seminiferous tubules and the spermatogenic epithelium begins to function. Sperm are produced continuously throughout the period of sexual activity. As a man ages, the production of germ cells in the convoluted seminiferous tubules decreases, and the tubules themselves become empty. However, high sexual activity slows down this process.
In a healthy adult man, 1 ml of semen contains about 100 million sperm, and during one ejaculation, 300–400 million are released. If the number of sperm in 1 ml of semen decreases to 20 million, infertility is usually observed. Although the testicles produce such a huge number of sperm, only one of them fertilizes the egg.
A human sperm has a head, neck and tail. The head of the sperm is ovoid; it contains a nucleus with half the set of chromosomes (23 chromosomes), like the egg. At the top of the head, a special formation contains enzymes that, during fertilization, dissolve the membrane of the egg and facilitate the penetration of sperm into it. Mitochondria are concentrated in the neck, providing the sperm with energy for movement. The movements of the tail allow the sperm to move at a speed of 2–3 mm per minute (however, when moving sperm in the female genital tract, their active motility is not critical).
Testosterone synthesis In addition to the seminiferous tubules, the testicle contains interstitial cells (Leydig cells). It is believed that they synthesize the male sex hormone (androgen) testosterone, which is carried throughout the body in the blood and acts on various cells sensitive to it, stimulating their growth and functional activity. The target cells for testosterone are the cells of the prostate gland (prostate), seminal vesicles, glands of the foreskin, kidneys, skin, etc. Under the influence of androgens, as already indicated, puberty occurs, secondary sexual characteristics arise, and sexual behavior is formed. A low concentration of androgens activates spermatogenesis, while a high concentration inhibits it. A small amount of female sex hormones – estrogens – is also synthesized in the testicles. Androgens and estrogens are involved in the regulation of growth and development of the musculoskeletal system.
Removal of both testicles (castration) entails not only the loss of the ability to bear children, but also significant changes in the body: metabolic disorders, changes in the timbre of the voice, cessation of beard and mustache growth, and a delay in overall growth (if it has not been completed).
Prostate gland Let's trace the path of sperm after they leave the testicle.
Along the posterior edge of the testicle is the epididymis, inside which sperm pass through a highly convoluted duct (up to 4–6 m in length) and enter the vas deferens.
The latter leaves the scrotum, rises through the inguinal canal into the abdominal cavity and goes to the bottom of the bladder and the prostate gland located here. Having pierced its wall, it opens into the urethra. The prostate gland covers the initial section of the urethra, into which the ducts of the gland itself and the ejaculatory ducts open.
As it moves forward, secretions from various glands are mixed with the sperm, which together form the liquid part of the sperm. About 70% of seminal fluid is the secretion of the seminal vesicles, 30% is the secretion of the prostate gland. Substances produced by them and the bulbourethral (Cooper) glands liquefy sperm, increase sperm viability and activate them.
Contraction of the muscle fibers of the prostate gland prevents urine from entering the urethra during ejaculation. Enlargement of the middle part of the prostate gland can make it difficult to urinate and lead to sexual dysfunction.
There is a constant interaction between the prostate gland and the testicles: an increase in the secretory activity of the testicles stimulates its development and function. During periods of sexual abstinence, the secretion of the prostate gland enters the blood in large quantities and this inhibits the function of the testicles. On the contrary, with great sexual activity, there is little prostate secretion in the blood and this stimulates the activity of the testicles.
Male urethra The male urethra begins with an internal opening in the wall of the bottom of the bladder and ends with an external opening on the head of the penis. The urethra serves to remove both urine and semen from the body. Its longest part is located in the corpus spongiosum of the penis. During sexual intercourse, sperm enter the woman's vagina through the urethra.
What should be the correct estrogen concentration?
It all depends on the phase of the menstrual cycle, as well as the stage of development, age and health of the woman. In different periods, estrogen levels are different.
Estradiol values:
- follicular phase: 30–120 ng/l (110–440 pmol/l),
- ovulation: 130–370 ng/L (477–1358 pmol/L),
- luteal phase: 70-250 ng/l (257-917 pmol/l),
- postmenopausal period: <10 ng/l.
Estrone:
- in the reproductive period 17-200 ng/l,
- during the postmenopausal period 7–40 ng/l.
Estriol: less than 80 ng/l.
Estrogen concentrations are checked in a diagnostic laboratory. A blood sample is analyzed. You must come for the examination in the morning on an empty stomach. It should also be remembered that the values in the test results should be directly compared with the standards indicated on them, and the correct interpretation should be left to the discretion of the doctor.
What to do if your estrogen levels are too low or too high?
Both excess and deficiency of these essential hormones can have negative consequences.
Excess estrogen most often occurs in women who are obese, have diabetes, have hypertension, and have certain types of cancer, such as ovarian cancer. This is also associated with taking inadequate doses of estrogen-based drugs.
The effects of excess estrogen include:
- menstrual irregularities,
- headaches, seizures, including migraines,
- nausea and vomiting
- excessive growth of the endometrium, which can lead to cancerous changes,
- increased risk of blood clots and embolisms,
- swelling,
- breast enlargement,
- weight gain,
- general malaise,
- mood swings.
Estrogen deficiency is physiological in women during menopause, but pathological in women of reproductive age.
This may contribute to the following disorders:
- irregular menstrual cycles or their absence,
- infertility,
- disappearance of 2- and 3-row sexual characteristics,
- vaginal dryness,
- urinary tract infections,
- urinary incontinence,
- hot flashes and profuse sweating,
- sleep disorders,
- decreased sexual desire,
- mood instability and depression,
- loss of breast firmness,
- deterioration of the quality of the skin,
- calcium disorders and osteoporosis,
- heart disease as a result of high cholesterol.
Progesterone is a hormone necessary for basic tasks, ovulation and pregnancy.
Progesterone, mentioned in connection with estrogens, is an equally important female hormone.
Progesterone
Progesterone, once called lutein, is secreted by the ovaries, more specifically the corpus luteum in the luteal and early stages of pregnancy, and the placenta in later stages of pregnancy. To a lesser extent, it is produced in the adrenal cortex and central nervous system.
What is this extremely important female sex hormone responsible for? The main tasks of progesterone:
- control and regulation of the menstrual cycle,
- influence on the onset of ovulation,
- preparing the uterine mucosa for the arrival and implantation of a fertilized egg,
- maintaining pregnancy throughout its entire duration,
- relaxation of the enlarging uterus in the second half of pregnancy and inhibition of its contractions,
- maintaining the correct structure and function of the cervix during pregnancy,
- suppression of excessive growth of the endometrium under the influence of estrogens,
- in combination with estradiol, stimulates the mammary gland and prepares it for lactation.
The effect of progesterone on a woman’s body depends primarily on the phase of the menstrual cycle.
During the follicular phase, progesterone levels are low and the ovaries primarily produce estrogen. Its level increases at the beginning of ovulation, which is a sign of ovulation itself. The highest level of progesterone is reached when the egg develops into the corpus luteum.
If the embryo is not fertilized and implanted, the concentration of progesterone decreases and the so-called luteolysis of the corpus luteum occurs. Under physiological conditions, a sharp decrease in progesterone levels will lead to menstrual bleeding.
It is easy to notice that progesterone levels fluctuate constantly. Progesterone levels at individual stages of the cycle are as follows:
- in the follicular phase: 0.28–0.72 ng/ml,
- in the perovulatory phase: 0.64–1.63 ng/ml,
- in the luteal phase: 4.71–18.0 ng/ml.
The concentration of progesterone during pregnancy varies and is:
- in the first trimester: 11.0-44.3 ng/ml,
- in the second trimester: 25.4-83.3 ng/ml,
- in the third trimester: 58.7–214 ng/ml.
During menopause, low progesterone levels (according to tests).
Both too low and too high levels of progesterone can impair basic body functions. Progesterone deficiency is one of the most common causes of fertility problems.
When it's not enough:
- menstruation becomes irregular, more abundant;
- there may be severe pain in the lower abdomen, uterine cramps, spotting or vaginal bleeding;
- there is a problem with pregnancy;
- problems with excessively dry skin and excessive hair loss are visible;
- possible increased symptoms of premenstrual syndrome (PMS);
- pregnancy may end in miscarriage.
The cause of too low progesterone levels may be a deficiency of the corpus luteum or problems with the placenta, dysfunction of the pituitary gland or hypothalamus, or poisoning during pregnancy. If excess progesterone is not associated with physiological changes such as pregnancy or the luteal phase, it may indicate a number of problems, including:
- liver failure,
- polycystic ovary syndrome,
- adrenal-genital syndrome,
- ovarian or adrenal cancer.
Polycystic ovarian syndrome
Too much progesterone may indicate swelling caused by water retention in the body or varicose veins.
Pancreas
The pancreas is located in the abdominal cavity and is not only an endocrine gland, but also an organ of the digestive system. But its hormones play a particularly large role in the regulation of protein, fat and especially carbohydrate metabolism. These include:
- Glucagon is a peptide hormone responsible for increasing blood sugar levels due to the entry of glucose into the blood as a result of the breakdown of glycogen. It also stimulates insulin production and increases blood pressure, heart rate and strength. In high doses, it provokes intestinal relaxation. But the hormone is most important for ensuring the ability to mobilize the body in stressful situations by providing cells with a source of energy - glucose.
- Insulin is responsible for reducing blood glucose levels, which makes it one of the most important hormones in regulating the metabolism of carbohydrates, as well as proteins and lipids. With a deficiency of insulin or impaired cell sensitivity to it, diabetes mellitus develops.
Prolactin, an extremely important female hormone during pregnancy and lactation
A hormone that is associated with reproductive function in both women and men is prolactin (PRL).
It is a peptide hormone, also known as luteotropic hormone (LTH), that is produced primarily in the anterior pituitary gland and to a lesser extent in the uterus and breasts in women, the prostate in men, and the skin or fat tissue.
Over the years, scientists have assigned this hormone more than 300 different tasks, which can be divided into:
- reproductive,
- metabolic,
- regulatory - in the field of fluids (osmoregulation), the immune system or behavioral functions.
Why is prolactin called the female hormone? Mainly because it is responsible for many important functions during pregnancy and lactation. First of all, the appropriate concentration of this hormone supports the functioning of the corpus luteum, which is responsible for the production of progesterone, another essential hormone. to maintain pregnancy.
It is also worth knowing that the name prolactin itself comes from a direct connection with lactation, that is, with the function of stimulating milk production, which occurs in response to breastfeeding. Prolactin stimulates the growth of mammary glands during pregnancy and causes lactation.
Moreover, in lactating women, it suppresses the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), thereby blocking ovulation and menstruation, especially in the first months of the postpartum period.
The regulation of prolactin levels is influenced by dopamine (a hormone secreted by the hypothalamus) and estrogens.
What are the normal prolactin levels? The concentration should be between 5-25 ng/ml, but should be assessed based on the standards provided by the specific test results. Another thing is that prolactin does not always remain the same. It is quite natural, for example, to increase prolactin during pregnancy and breastfeeding.
Fluctuations in this hormone are also observed during the menstrual cycle. At first it increases slightly, and in the second half it gradually decreases. Thus, we can distinguish different prolactin norms for women. It should be:
- in the follicular phase below 23 μg/l,
- in the luteal phase below 40 μg/l,
- and in the third trimester of pregnancy up to 400 mcg/l.
It is also worth mentioning that prolactin values can be expressed in different units. Mainly in ml/ml and in hives/ml. They are recalculated using the formula 1 ng/ml = 20 mIU/l.
Moreover, prolactin concentration is also related to the circadian cycle. In the second half of the night, hormone levels rise, reach a peak in the early morning, and then gradually decrease.
Changes in the level of this hormone are also influenced by stress, sexual intercourse, rich food or exercise.
Any abnormalities require a prolactin level test. The examination involves analyzing a blood sample taken in the morning on an empty stomach, preferably between 8 and 12 o'clock.
What does excess prolactin mean? Everything depends, of course, on the conditions described above. However, even if a woman is not pregnant, elevated prolactin levels may mean:
- more than 25 ng/ml – the occurrence of irregular periods and non-ovulatory cycles,
- more than 50 ng/ml – complete cessation of menstruation,
- more than 100 ng/ml – risk of pituitary tumor.
Too high prolactin levels can manifest as:
- menstrual irregularities, including scanty bleeding with a tendency to stop completely,
- breast pain and tenderness,
- galactorrhea, that is, leakage of milk from the nipples, even outside of pregnancy or breastfeeding,
- decreased libido,
- Vaginal dryness, which can lead to pain during intercourse.
Decreased libido
It is worth knowing that excess prolactin in women can lead to problems with pregnancy. Hyperprolactinemia, the so-called increase in the level of the hormone prolactin, may have the above physiological background:
- during pregnancy or breastfeeding, during sleep or exercise,
- for pathological conditions caused by various diseases, including pituitary adenoma, renal or liver failure, hypothyroidism or taking certain medications.
Hypoprolactinemia, that is, a decrease in prolactin concentration below normal, is diagnosed much less frequently. This mainly occurs in people suffering from hypopituitarism.
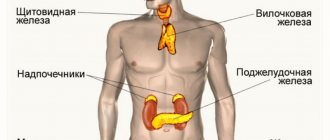
Endocrine system and hormones: what is it?
The endocrine system is a whole complex of interconnected organs and endocrine glands that synthesize hormones. They, under the guidance of the nervous system, regulate the course of a huge number of biochemical transformations occurring in the body and the functioning of internal organs through the same hormones.
Hormones are biologically active substances that are synthesized by the body in small quantities and are responsible for transmitting information to other organs without changing their nature and without directly entering into various biochemical transformations.
Elements of the endocrine system are both the endocrine glands themselves (pancreas, thyroid, parathyroid glands), and individual organs, as well as parts of the brain, including the pituitary gland, hypothalamus, pineal gland, thymus, adrenal glands, gonads (testes in men and ovaries in women) . Even adipose tissue is a hormone-producing organ. In addition, endocrine cells are found in a number of other organs, including the heart, kidneys, etc.
Each of them is responsible for the production of a specific hormone, which is released into the blood and delivered directly to the target organs and tissues, starting or stopping the course of a particular process. Thanks to this, it not only ensures the fulfillment of processes important for life, but also the body’s ability to sensitively adapt to changes in the conditions of the internal and external environment, to grow and develop.
The interaction of hormones with tissues occurs mainly according to the feedback principle. That is, the hormone synthesized by the endocrine gland is delivered to target cells, triggers a certain process, which leads to the production of another hormone by another gland, which affects the source of production of the first, letting us know that the desired process has been completed and thereby inhibiting its synthesis. Thus, all hormones and, accordingly, endocrine organs are closely interconnected and are sensitive to changes in each other’s work. Therefore, when disturbances occur in one of the organs of the endocrine system, the entire body inevitably suffers.
Thus, the balance of hormones is very important for the body, but it can be disrupted due to the action of various factors, including:
- stressful situations;
- chronic lack of sleep;
- weakened immunity;
- smoking and alcohol abuse;
- irrational use of medicines;
- infection with helminths and other parasites;
- some diseases.
Unfortunately, every person can encounter such factors, since it is almost impossible to avoid them in modern life. Therefore, hormonal imbalances are extremely common today, which leads to unfavorable chain changes in the functioning of the body, disruption of many metabolic processes and the development of a wide variety of diseases, the complications of which can even lead to fatal consequences. Therefore, any changes in hormonal levels require medication correction.
However, the male body is more stable in terms of maintaining normal hormonal levels. In women, it can fluctuate due to physiological changes, in particular during pregnancy, during breastfeeding and during menopause. In addition, female hormonal levels regularly change during each menstrual cycle, which explains the fact that it is necessary to take tests for female sex hormones strictly on certain days of the cycle. Otherwise, the data obtained may not be informative.
In order to avoid the development of various diseases caused by changes in hormonal levels, it is important to correct them in a timely manner, including during physiological changes caused by menopause, since estrogen deficiency increases the risk of developing not only diseases of the genital organs, but also oncology.
Today, more than 60 different hormones are known, including sex hormones. Female sex hormones are called estrogens, male hormones are called androgens. However, this gradation is rather arbitrary, since both estrogens and androgens are synthesized in the female body, just like in the male body. Moreover, androgens act as the basis for the synthesis of estrogens in women and play an important role in maintaining homeostasis. Let's take a closer look at the organs of the endocrine system and their main hormones.
Gonadotropins, that is, hormones necessary for proper childbirth
The very name of gonadotropic hormones suggests their key role in the human body. They are responsible for stimulating the activity of the human gonads, that is, the female ovaries and male testes. They are secreted by the anterior pituitary gland.
Gonadotropins primarily include:
- follicle-stimulating hormone (FSH), that is, follicle-stimulating hormone,
- luteinizing hormone (LH), called lutropin.
This group of hormones also includes human chorionic gonadotropin (hCG), released during pregnancy.
The FSH hormone in women is intended to stimulate the growth of ovarian follicles, control their development and regulate the functions of the corpus luteum. Stimulates the secretion of estrogens by granular cells of ovarian follicles.
Levels of stimulation of blood follicles depend on the woman’s age and the phase of the menstrual cycle. FSH norms in women are:
- in the follicular phase – below 12 IU/l,
- in the ovulation phase – from 20 to 90 IU/l,
- in the luteal phase – below 10 IU/l,
- during menopause – from 40 to 250 IU/l (after menopause, FSH concentration increases),
- during pregnancy – trace concentrations.
Insufficient FSH levels are usually associated with pituitary and/or hypothalamic failure. An excess, in turn, may indicate primary or acquired ovarian failure or inhibition of ovulation stimulation.
The LH hormone in women is primarily responsible for ovulation, and its main task is to regulate and control the secretion of progesterone. After the egg enters the fallopian tube, lutropin converts granulosa cells into lutein cells (which produce progesterone), and the cells of the inner layer in the follicle shell into paralutein cells (which produce estrogens).
The role of luteinizing hormone is also to support the production of progesterone and estrogen by the corpus luteum.
As with FSH, the concentration of lutropin depends on the time of the cycle and the age of the woman. LH norms for women:
- in the follicular phase – up to 5-30 IU/l,
- during ovulation – from 75 to 150 IU/l,
- in the luteal phase – from 3 to 40 IU/l,
- after menopause – 30-300 IU/l.
Too low levels of lutropin may indicate damage to the pituitary gland or hypothalamus.
On the other hand, excess LH hormone may indicate insufficient ovarian activity or neoplastic changes in the pituitary gland.
Androgens, or male hormones in the female body
The group of steroid sex hormones also includes androgens, that is, androgenic hormones.
They are associated primarily with masculine attributes, but are found in both sexes, and their role is primarily to control the proper development of sexual characteristics in both men and women. In women, androgenic hormones are primarily produced by the adrenal glands and to some extent by the ovaries.
These include:
- popular testosterone,
- androstenedione,
- dehydroepiandrostenedione (DHEA),
- dihydrotestosterone (DHT).
Androstenedione and dihydrotestosterone play an important role in the female body because they act as precursors of female sex hormones, that is, estrogens. They are primarily responsible for triggering and controlling the maturation process in girls, as well as libido levels, mood, bone metabolism and fertility in more mature women.
Total daily testosterone production is about 100-400 mcg. Testosterone levels in women change along with the menstrual cycle. The lowest concentration is observed in the early follicular phase.
Testosterone levels in women are:
- free testosterone: 10.4-45.1 pmol/l,
- total testosterone: 1-2.5 nmol/l.
Testosterone levels increase in pregnant women, with the highest levels being reached in the third trimester. In turn, in the period from 20 to 45 years, the concentration of this hormone in the female body decreases by 50%.
Should women have their testosterone tested? Indications for testing the level of testosterone and other androgens in women are primarily:
- Hirsutism, that is, the presence of excessive hair in typical male areas, such as the lips and chin, forearms, thighs, chest, abdomen, back and genitals;
- Masculinization, that is, the presence of male sexual characteristics in women of the tertiary level, such as the aforementioned excessive hair growth characteristic of men, as well as enlargement of the clitoris and labia, breast reduction, decreased tone of voice, increased muscle mass, as well as the appearance of acne, seborrheic dermatitis or male pattern baldness;
- Menstrual irregularities;
- Difficulties with pregnancy.
Disorders in the adrenal cortex and ovaries, including various types of cancer or polycystic ovary syndrome, may be responsible for too high androgen levels in women.
Because the effects of androgens, including testosterone, are weaker in women, symptoms of deficiency of these hormones may be milder. You may notice, first of all: decreased sex drive, depression and mood swings, fatigue, impaired concentration and memory, or a general lack of energy.
External genitalia
1 – pubis; 2 – foreskin of the clitoris; 3 – head of the clitoris; 4 - labia minora; 5 - external opening of the urethra; 6 - hymen (is the border between the external and internal genital organs); 7 - Bartholin gland; 8 - anus; 9 — entrance to the vagina; 10 - labia majora.
Pubis
The pubis is an elevation located in front and slightly above the pubic joint, covered with hair, the upper limit of which grows horizontally (in men, hair growth extends upward along the midline).
Clitoris
The clitoris is a small (up to 1-1.5 cm), but very sensitive and important organ, consisting mainly of the corpus cavernosum. The male penis has a similar structure. The cavernous body has voids filled with circulating blood. During sexual arousal, these voids are intensely filled with blood, and the clitoris becomes enlarged and thickened—an erection. The corpus cavernosum is not capable of contracting like blood vessels, so traumatic injury to the clitoris is dangerous due to excessive bleeding.
Labia minora
The labia minora (LGB) are two folds of skin between the labia majora and the opening of the vagina. In front, connecting, they form the foreskin of the clitoris. Normally, the labia minora protrude slightly beyond the boundaries of the major lips, their color varies from pale pink to dark brown in the posterior regions. MPGs have a large number of vessels and nerve endings and are an ergenic zone; during sexual arousal, they increase in size due to blood flow.
PGMs are variable in shape and size, and are often asymmetrical. If the shape and size of the labia minora cause physical or mental discomfort, surgical correction of their size and the shape of the labia minora are performed.
sex slit
The genital fissure is the space between the labia majora and labia minora.
Labia majora
The labia majora (LGB) are two pronounced longitudinal folds of skin located on the sides of the genital slit. Anteriorly, the BPG converge into the anterior commissure, located above the clitoris. Behind, narrowing and converging one on the other, the BPG pass into the posterior commissure. The skin of the outer surface of the GPG has hair and contains sweat and sebaceous glands. The thickness of the labia majora contains blood vessels, nerves and Bartholin glands. On the inside they are covered with thin pink skin similar to a mucous membrane.
There are two openings under the labia majora and minora. One of them, with a diameter of 3 - 4 mm, located just below the clitoris, is called the external opening of the urethra (urethra), through which urine is discharged from the bladder. Directly below it there is a second hole with a diameter of 2 - 3 cm - this is the entrance to the vagina, which covers (or once covered) the hymen.
External opening of the urethra
The external opening of the urethra has a round, semi-lunar or star-shaped shape, it is located 2-3 cm below the clitoris. The urethra is 3-4 cm long, its lumen stretches to 1 cm or more. Along its entire length it is connected to the anterior wall of the vagina. On both sides of the external opening of the urethra are the excretory ducts of the paraurethral glands. These formations produce a secretion that moisturizes the mucous membrane of the external opening of the urethra.
Bartholin glands
Bartholin's glands (glands of the vestibule of the vagina) are paired, oblong-rounded formations, the size of a bean. They are located on the border of the posterior and middle third of the labia majora and produce a whitish secretion with a specific odor. The secret moisturizes the mucous membrane and has antibacterial properties.
Vaginal vestibule
The vestibule of the vagina is an anatomical formation. The “bottom” of the vaginal vestibule is the hymen or its remnants. In front, the vestibule is limited by the clitoris, behind - by the posterior commissure, on the sides - by the labia minora.
Hymen
The hymen (hymen) is the thinnest ring-shaped or semi-lunar-shaped membrane, 0.5 - 2 mm thick. With the onset of sexual activity, the hymen is torn. The hymen is the boundary between the external and internal genitalia.
Crotch
The perineum in the anatomical sense is the area between the pubis and the top of the coccyx, on the sides limited by the ischial tuberosities of the pelvic bones, in fact it is the exit from the small pelvis. In a clinical (obstetric) sense, the perineum is considered the area between the posterior commissure of the labia majora and the anus (Fig. 1). On the skin of the perineum there is a pigment line running from the posterior commissure to the anus - the perineal suture. The distance from the posterior commissure to the anus is called the perineal height and is 3-4 cm.
Rice. 1.
Anatomical landmarks of the female perineum: 1 - anterior commissure of the labia majora, 2 - posterior commissure of the labia majora, 3 - anus (anus), 4 - apex of the coccyx, 5 - ischial tubercle (on the left).
The thickness of the perineum consists of the skin, muscles, their tendons and fascia. The set of soft tissues occupying the space of exit from the small pelvis forms the pelvic floor or pelvic diaphragm. A woman's urethra, vagina, and rectum pass through the pelvic diaphragm.
The muscles and ligaments of the pelvic floor support the pelvic organs (bladder, vagina and rectum) in an anatomical position and provide a number of very important physiological functions: voluntary urination and urinary retention, defecation, retention of feces and intestinal gases, closure of the vaginal opening, are part of labor paths (Fig. 2).
Damage to these structures during childbirth leads to insufficiency of the perineal muscles and disruption of the pelvic organs - pelvic floor dysfunction, sexual dysfunction. This is written in detail in this article.
Rice. 2.
Sagittal section of the pelvic floor
Thyroid hormones – support for health and beauty or a threat to fertility?
Thyroid hormones, including mainly triiodothyronine (T3), thyroxine (T4) and calcitonin (CT), are equally important for health, including fertility and beauty.
All three are produced by the thyroid gland and perform different functions in the female body. Their beneficial effects can be felt first of all:
- in the proper functioning of calcium-phosphate metabolism, that is, bone metabolism, for which calcitonin is responsible;
- in accelerating metabolism, which promotes increased calorie burning - in this case, triiodothyronine is in the lead;
- in maintaining the proper condition of the skin and hair, which is facilitated by thyroxine.
However, endocrine disorders, including abnormal levels of thyroid hormones, can lead to irregular menstruation, anovulation and hence infertility. Moreover, even when the opportunity to become pregnant arises, problems may arise in maintaining it. Manifested by miscarriage or premature birth.
Premature birth
Thyroid hormone levels:
- T3: 2-10 mU/l,
- T4: 5-12 mcg/dl,
- CT: 8.3-22.0 pmol/l (30-80 pg/ml),
- TSH (thyroid-stimulating hormone secreted by the pituitary gland): 0.27-4.0 mU/l.
Depending on abnormalities in thyroid hormone levels, there may be an overactive or underactive thyroid gland.
Thyroid
The thyroid gland is a small endocrine gland located on the front surface of the neck and consisting of two halves connected by an isthmus. It produces the same thyroid hormones that have a close relationship with TSH.
Thyroid hormones are biologically active substances whose molecules contain iodine. These are thyroxine (T4) and triiodothyronine (T3), which regulate the processes of growth and development of the body, and are also involved in the regulation of metabolic rate. They increase the tissue's need for oxygen, and also contribute to an increase in blood pressure, frequency and strength of heart contractions.
A person’s energy, psychological energy and the speed of cognitive processes depend on thyroid hormones. They also promote the formation of glucose in the liver and its use by cells, while they suppress the accumulation of glycogen. In addition, thyroid hormones promote faster decomposition of fat and prevent the formation of new ones.
Diagnosis of female sex hormones - what tests and when to do?
Analysis of the concentration of female sex hormones is important at many stages of a woman’s life, including:
- when abnormalities are detected in the body that may indicate an excess or deficiency of one of the hormones,
- during many unsuccessful attempts to get pregnant,
- for menstrual irregularities,
- during pregnancy,
- in the perimenopausal period, to check hormone levels and the possible decision to introduce hormone replacement therapy,
- in cancer prevention.
A doctor who specializes in hormones is an endocrinologist. The specialist may order specific blood tests and indicate, among other things:
- at what point in the cycle should you go to the laboratory,
- how to prepare for the test,
- When is the best time to get your blood tested?
This all depends on the need to check the level of a specific hormone and the exact purpose of the analysis.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
If you find an error, please select a piece of text and press Ctrl+Enter