Pharmacodynamics and pharmacokinetics
Pharmacodynamics
INN (International Nonproprietary Name) - piribedil . Dopaminergic receptor stimulator . Passes through the blood-brain barrier and reacts with dopaminergic receptors of neurons , demonstrating high affinity and selectivity for D2 and D3 receptor types . Shows antagonism towards α2A and α2C types of adrenergic receptors . Long-term use of piribedil leads to less severe dyskinesia than Levodopa , with comparable effectiveness in relation to temporary akinesia due to Parkinson's disease .
In healthy patients, piribedil enhances the attention and vigilance needed to perform cognitive tasks.
The effectiveness of the drug in the treatment of Parkinson's disease has been proven in the results of 3-blind double clinical placebo-controlled studies.
dopamine receptors in the vessels of the legs explains the vasodilatory effect of piribedil .
Pharmacokinetics
It is quickly and completely absorbed from the intestines and actively distributed.
The highest levels of piribedil in the blood are achieved 4-5 hours after oral administration. Reaction with plasma proteins is 20–28%. The risk of interaction when using piribedil with other drugs is low due to its weak binding to blood proteins.
A stable concentration of the active substance is maintained in the blood throughout the day. The half-life is approximately 12 hours. It is intensively transformed in the liver and is evacuated mainly in the urine in the form of metabolites.
Pharmacokinetics
Piribedil is quickly and almost completely absorbed from the gastrointestinal tract and distributed intensively.
Cmax of piribedil in blood plasma is achieved 3-6 hours after oral administration of the controlled-release dosage form. Plasma protein binding is average (the unbound fraction is 20–30%). Due to the low binding of piribedil to plasma proteins, the risk of drug interactions when used with other drugs is low.
Plasma elimination of piribedil is biphasic and consists of an initial phase and a second slower phase, leading to the maintenance of a steady-state plasma concentration of piribedil for more than 24 hours.
In a combined pharmacokinetic analysis, it was shown that T1/2 of piribedil after intravenous administration averages 12 hours and does not depend on the dose administered.
Piribedil is extensively metabolized in the liver and is excreted mainly in the urine: 75% of absorbed piribedil is excreted by the kidneys in the form of metabolites.
Indications for use
- Auxiliary symptomatic treatment for chronic cognitive impairment and neurosensory deficits that develop during the aging process (including attention and memory disorders).
- Monotherapy for Parkinson's disease (in forms mainly characterized by tremor ) or as part of multicomponent therapy with Levodopa at various stages of the disease.
- Auxiliary symptomatic treatment for intermittent claudication due to obliterating lesions of the arteries of the legs .
- Treatment of symptoms of ophthalmological diseases of ischemic origin (including weakened visual acuity, decreased visual field, decreased visual contrast).
Memory impairments and the role of Pronoran in their correction
The article discusses the causes of memory loss and the development of other cognitive impairments. It is noted that the nature of memory impairment depends on the location of the damage and the specifics of the pathological process. Treatment for cognitive impairment includes both non-drug and pharmaceutical methods. The choice of specific drugs that improve cognitive function depends on the severity of the cognitive defect. The possibility of using the dopamine receptor agonist Pronoran in the complex treatment of moderate cognitive disorders, including memory impairment, is discussed in detail.
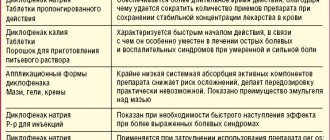
Table 1. Memory impairments
Table 2. Types of mild cognitive impairment
Table 3. Drugs used to treat cognitive impairment
Epidemiology
Complaints of memory loss regularly occur in patients of all ages. Thus, about a third of young and middle-aged people and up to 70% of older people report dissatisfaction with their memory, half of them have objective impairments [1]. The high prevalence of memory impairment is explained by a wide range of neurological, somatic and mental diseases that occur with mnestic disorders. In young people, memory impairment is usually a consequence of astheno-neurotic syndrome, which is predominantly reversible and regresses with adequate treatment. In older people, memory loss is often caused by organic brain damage, which leads to persistent progressive cognitive deficits that are difficult to treat.
According to the large Russian study PROMETHEUS-I, 83.4% of elderly patients (2677 out of 3210 examined) who came to see outpatient neurologists complained of decreased memory or mental performance. 68.2% of patients exhibit objective cognitive impairment, confirmed by neuropsychological examination, with 25% of patients having severe cognitive deficits [2].
Risk factors for cognitive impairment
The problem of the growing number of patients with cognitive dysfunction is becoming increasingly important every year, which is primarily due to the increase in the population of elderly and senile people (65 years and older). In 2010 in Russia, this age group accounted for 12.9%, and by 2030, according to the official demographic forecast, the share of the elderly population will increase to 18–19.4% [3].
Age is considered the most significant risk factor for cognitive impairment. Even with normal aging, the brain undergoes a number of involutive changes (brain volume, the number of neurons and glial cells, the number of dendrites, synapses and receptors, the content of mediators, the level of metabolism and brain perfusion decrease). As a result, working memory and concentration weaken, reaction speed and mental activity slow down. With successful aging, these changes are expressed insignificantly and do not interfere with a person’s life and daily functions at work and at home. However, the aging process is inevitably accompanied by the emergence of chronic somatic pathology and neurological diseases, which lead to more pronounced cognitive dysfunction. Family history also plays a role, especially in diseases such as Huntington's disease and Alzheimer's disease. Vascular risk factors play a major role in the development of memory disorders and other cognitive functions: hypertensive and coronary heart disease, rhythm disturbances, hyperlipidemia, obesity, diabetes mellitus, etc. This unfavorable background provokes the development of acute and chronic cerebral ischemia, and also stimulates neurodegenerative processes.
Memory disorders
Memory is one of the basic cognitive functions (along with attention, language, praxis, gnosis and intelligence). This is the ability of the central nervous system to assimilate new information, store it and use it in the process of life. Conventionally, there are three components of memory:
1) registration (memorization);
2) storage (retention);
3) reproduction (extraction) of information.
Most often, registration and reproduction suffer; selectivity of reproduction may be impaired and confabulations (false memories) may occur [4].
Based on the duration of storage of material, it is customary to distinguish ultra-short-term (immediate), short-term and long-term memory [5].
Ultra-short-term memory.
Contains information directly coming from the senses, without transformation. The volume of direct memory is unlimited - sensory analyzers record all incoming information, but the duration of such memory is a fraction of a second - the time during which the impact on the analyzer continues. An example is writing from dictation, repeating words or rewriting text. Immediate memory suffers relatively rarely, for example, in the advanced stage of Alzheimer's disease, when the neurodegenerative process takes over most of the cerebral cortex (modality-nonspecific memory impairment). Problems with immediate memory can also arise with local lesions of the cerebral cortex (for example, tumors), when, depending on the location of the lesion, the memorization of visual, auditory-verbal, tactile or motor information worsens in isolation (modality-specific memory impairment).
Short-term memory.
It is characterized by a small volume and duration of information storage (seconds - minutes), during which time repetition, recoding and selection of a memorization method occur. Then the process of transferring information into long-term memory occurs; it is designated by the term “consolidation of the memory trace” and lasts up to 24 hours. It is believed that the number of structural units that can be stored in short-term memory is 7 ± 2. For example, out of 10 words heard, a person can immediately repeat 7 ± 2 words. This rule applies not only to auditory, but also to visual and any other modality. Short-term memory impairments are closely related to decreased attention and primarily occur with subcortical lesions (subcortical dementia, cerebrovascular lesions, etc.).
Long-term memory.
Has unlimited volume and storage time. It can be divided into episodic (event-based), which stores information about all events in a person’s life, and semantic (symbolic), which contains knowledge about verbal and non-verbal designations for all phenomena, that is, knowledge of language. Problems with episodic memory are very common (the patient forgets what happened to him, what he did, ate, read). Such disorders are characteristic of any type of dementia, Korsakoff's syndrome, local brain lesions (structures of the hippocampal circle, frontal lobes, etc.). Semantic memory always suffers along with other cognitive functions, and it is extremely difficult to assess its condition in isolation. Most often they resort to a test for naming words belonging to the same semantic category (animals, plants). Semantic memory may decline in advanced stages of Alzheimer's disease.
Long-term memory is divided into a declarative component (information about any facts and objects) and a procedural component (skills, habits, and ways of behavior learned from life experience). For procedural memory, learning ability and the ability to more successfully complete a task when presented repeatedly are important. Procedural memory usually suffers when connections between the frontal lobes and subcortical structures are damaged, for example in subcortical dementias.
Voluntary and involuntary memory.
The processes of involuntary memorization and reproduction are not realized by the subject. Problems with involuntary memory arise with lesions of the right hemisphere of the brain, various subcortical cognitive disorders, and in advanced stages of Alzheimer's disease. It is believed that involuntary memory is not affected in the early stages of Alzheimer's disease and Korsakoff's syndrome [6]. Thus, the nature of memory impairment depends on the location of the damage and the specifics of the pathological process (Table 1).
Specific areas of the brain involved in memory processes are the hippocampus, amygdala, striatum, and mamillary bodies. It is assumed that the hippocampus provides the function of declarative learning, and the amygdala provides emotional memory. However, damage to many other structures also leads to impairments in attention, and therefore memory and learning. Depending on the location of the lesion, memory impairment can occur in isolation or be combined with other cognitive disorders.
Isolated memory impairment syndrome is quite rare; an example is Korsakov's syndrome. Korsakov's syndrome is characterized by a combination of fixation and retrograde amnesia with confabulations. It develops with damage to the mamillary bodies, hippocampus and its connections. Causes include alcoholism, thiamine deficiency due to fasting or malabsorption, tumors, trauma, or circulatory disorders involving the hippocampal circuit structures. Patients instantly forget the content of the words just spoken; after a couple of minutes they do not remember who addressed them or what they did. Events that immediately preceded the disease (perhaps weeks, months and even years) may completely disappear from the patient’s memory. In severe disorders, disorientation occurs; patients are unable to name the current date or even the year, and cannot find their bed or the way to the toilet. The prognosis for this condition is often disappointing; it requires emergency measures aimed primarily at eliminating the cause of the disease.
Most often, memory impairments are combined with other cognitive disorders and accompany any neurological or psychiatric disease.
Mild cognitive impairment
Depending on the severity of cognitive decline, mild, moderate cognitive impairment and dementia are distinguished. Typically, chronic cerebrovascular diseases and neurodegenerative processes have a pre-dementia stage.
The term “moderate cognitive impairment” denotes a deterioration in cognitive abilities that exceeds the expected deterioration of cognitive functions for a given age, but does not reach the level of dementia and does not lead to social and everyday maladjustment [7]. The nosology “moderate cognitive impairment” is included in the latest revision of the International Classification of Diseases (ICD-10) and has its own diagnostic criteria:
- complaints of memory impairment or increased fatigue during mental work;
- objective evidence of decline in memory, attention, or learning ability;
- the level of impairment is insufficient to diagnose dementia;
- cognitive impairments are organic in nature.
Depending on the presence or absence of memory impairment, several main types of mild cognitive impairment are distinguished (Table 2).
Approximately 50–70% of patients with mild cognitive impairment develop dementia within four to five years, but 20% of patients show improvement in cognitive function at follow-up [3]. Thus, moderate cognitive impairment is a very heterogeneous condition in its course and clinical manifestations. Early diagnosis makes it possible to timely identify the potential cause and risk factors for the development of cognitive impairment, begin adequate therapy and thereby prolong the patient’s active life, delay, and sometimes prevent the development of dementia.
Dementia
Dementia is a multiple disorder of cognitive functions, which, unlike mild cognitive impairment, leads to social maladjustment. In most cases, the decline in cognitive function at the stage of dementia is irreversible. Memory impairment is considered a key sign of dementia and is included in the diagnostic criteria according to ICD-10:
- memory impairment (impaired ability to memorize new material, difficulty in reproducing previously learned information);
- impairment of other cognitive functions (impaired ability to judge, think (plan, organize) and process information);
- clinical significance of detected disorders;
- impairment of cognitive functions is determined against the background of preserved consciousness;
- emotional and motivational disorders – at least one of the following signs: emotional lability, irritability, apathy, antisocial behavior;
- the duration of symptoms is at least six months.
However, it must be borne in mind that some neurodegenerative diseases (for example, frontotemporal degeneration), especially in the initial stages, may occur with minor mental disorders or without them at all. In such cases, dementia will be diagnosed based on a decrease in any two cognitive functions leading to maladjustment.
The causes of the development of mild cognitive impairment and dementia are the same, they are very diverse:
- neurodegenerative diseases (Alzheimer's disease, dementia with Lewy bodies, frontotemporal degeneration, Parkinson's disease, etc.);
- vascular diseases of the brain;
- mixed vascular degenerative dementias;
- dismetabolic and toxic encephalopathies;
- neuroinfections;
- demyelinating diseases;
- post-traumatic encephalopathy;
- tumors;
- normal pressure hydrocephalus;
- other rarer diseases.
The most common cause of cognitive impairment in old age (40–50% of all dementias) is Alzheimer's disease. This degenerative brain disease is accompanied by the formation of neurofibrillary tangles and amyloid plaques in the brain and is clinically manifested by progressive dementia. Memory problems are considered the main and for a long time may remain the only symptom of Alzheimer's disease. The patient begins to forget emotionally unimportant events, new names, the content of recent TV shows and books, while memory for distant events remains relatively intact for a long time. In the advanced stages of Alzheimer's disease, memory impairments are combined: fixation, anterograde and retrograde amnesia and confabulations are observed, which generally resembles Korsakoff's syndrome. However, unlike the latter, the clinical picture of Alzheimer's disease also includes other cognitive disorders: apraxia, agnosia, and speech disorders.
In approximately 15–20% of cases, Alzheimer's disease is accompanied by vascular damage to the brain. This “mixed” pathology is considered the second most common cause of cognitive impairment in old age, followed by vascular dementia (10–15%), dementia with Lewy bodies (5–15%) and rarer forms [8].
Treatment of memory impairment and other cognitive disorders
Treatment of cognitive disorders, including memory impairment, is currently quite limited, predominantly symptomatic, and consists of the following areas:
- correction of somatic disorders and dysmetabolic disorders;
- eliminating or minimizing doses of drugs that impair cognitive function;
- treatment of emotional and behavioral disorders;
- neuropsychological rehabilitation and other non-pharmacological approaches;
- prescribing medications that improve cognitive function.
Pathogenetic therapy is possible for so-called reversible cognitive disorders. These include dysmetabolic and endocrine disorders, diseases accompanied by cardiac and respiratory failure, infectious diseases, in some cases, brain tumors and other disorders, the timely elimination of which makes it possible to prevent organic damage to the brain and restore its normal functioning. Therefore, the doctor’s primary task is to diagnose and make the most complete correction of concomitant somatic and neurological diseases.
Elderly patients usually take a large number of medications, some of which can worsen or even cause cognitive impairment. Such drugs include drugs with an anticholinergic effect, tricyclic antidepressants, benzodiazepines, barbiturates, and antipsychotics. The use of these drugs in elderly and senile patients should be limited as much as possible.
On the one hand, emotional disorders often accompany cognitive disorders, since they are a consequence of the same organic brain damage. On the other hand, anxiety-depressive disorders can themselves cause a decrease in memory, attention, fatigue, causing a kind of cognitive defect “pseudo-dementia”. In any case, emotional instability requires separate specific therapy, against the background of which partial regression of cognitive disorders is possible. Most often, with organic diseases of the brain, depressive symptoms develop, requiring the use of antidepressants. The choice of an antidepressant is made taking into account its effect on cognitive and somatic functions. Preference is given to drugs with a selective mechanism of action.
Non-drug methods of combating cognitive disorders are effective mainly at the stage of mild and moderate cognitive impairment, and are also certainly useful for preventive purposes. Neuropsychological rehabilitation, in other words, the creation of a cognitive reserve - mental activity, memory and attention training, social contacts, emotional life, is necessary for older people. Moderate physical activity, physical therapy, and adherence to a Mediterranean diet are recommended.
Currently, a fairly wide range of drugs that improve cognitive function is offered. The main groups are presented in table. 3. The choice of therapy primarily depends on the severity of the cognitive defect, since various management tactics are recommended for mild cognitive impairment and dementia.
Acetylcholinesterase inhibitors
The acetylcholinergic system is of great importance for the processes of concentration and memory. The role of cholinergic deficiency is shown in the main forms of dementia: Alzheimer's disease, vascular, mixed, etc. The severity of cholinergic disorders correlates with the severity of dementia, neuron death, the number of senile plaques and neurofibrillary tangles. It has been experimentally proven that a deficiency of central cholinergic systems leads to the deposition of beta-amyloid in the brain, forming senile plaques, and, on the contrary, an increase in the concentration of acetylcholine in the brain activates the growth of neurons and promotes an increase in the number of synapses, that is, it has a neuroplastic effect [9]. In this regard, the fight against memory impairment and the development of dementia is largely based on the action of acetylcholine.
Centrally acting acetylcholinesterase inhibitors block the breakdown of acetylcholine in the synaptic cleft, thereby enhancing neurotransmission. With the use of acetylcholinesterase inhibitors, stabilization of the condition and some regression of the severity of cognitive and behavioral disorders are noted, especially in the initial stages of dementia. Currently, four drugs from the group of acetylcholinesterase inhibitors are used: donepezil, galantamine hydrobromide, rivastigmine and ipidacrine. In therapeutic dosages they have comparable effectiveness (50–70%). During therapy with acetylcholinesterase inhibitors, memory and other cognitive functions improve, and the ability to self-care increases. If there is no effect, it is recommended to replace one acetylcholinesterase inhibitor with another. If acetylcholinesterase inhibitors are intolerant or insufficiently effective, therapy with non-acetylcholinergic drugs is prescribed.
Memantine
Efficacy in dementia has been proven for the NMDA receptor antagonist memantine glutamate.
The glutamatergic system is directly involved in the development of cognitive deficits. In Alzheimer's disease, vascular and other types of dementia, excessive activity is observed, a large amount of glutamate is released and the phenomenon of excitotoxicity occurs (cell destruction as a result of excess glutamate and overstimulation). The antagonist of NMDA receptors for glutamate, memantine, normalizes glutamatergic transmission, thereby providing a neuroprotective and symptomatic positive effect.
Both monotherapy for dementia and combined use of acetylcholinesterase inhibitors and memantine are possible. If there is a clinical effect, treatment is carried out for life. The effectiveness of acetylcholinesterase inhibitors and memantine in Alzheimer's disease and some other dementias has been shown in large multicenter placebo-controlled studies and is beyond doubt. However, in moderate cognitive impairment, the advisability of using acetylcholinesterase inhibitors and memantine has not been proven and remains a subject of debate [9]. In addition, acetylcholinesterase inhibitors have a fairly wide range of side effects. Therefore, their prescription for cognitive impairment not reaching the level of dementia should be considered on an individual basis in patients with mild cognitive impairment of the Alzheimer's type.
Piribedil
Drugs that affect the dopaminergic and adrenergic systems are considered promising for the correction of moderate cognitive impairment. Both of these mediators are necessary for cognitive functions. The noradrenergic system is involved in maintaining active wakefulness, an adequate level of attention and memory processes. Activation of dopaminergic transmission is also necessary for switching attention; its insufficiency leads to increased inertia, that is, slowness of cognitive processes (bradyphrenia), in particular, decreased speech fluency and perseverations. It has been shown that even minor dopamine deficiency, characteristic of older people, plays a significant role in age-related decline in memory and other cognitive functions.
Age-related changes in the brain are accompanied by loss of neurons and slowing of metabolism. This is especially true for dopaminergic formations of the frontal and subcortical regions. With age, the bioavailability of dopamine D2 receptors in the basal ganglia and their density decrease, which negatively affects the performance of cognitive tests. A decrease in markers of the dopaminergic system correlates with impaired function of the frontal cortex, deterioration of memory, attention, and weakened metabolism in the prefrontal and anterior cingulate cortex [10]. Naturally, in neurodegenerative and cerebrovascular diseases, neuronal death and neurotransmitter dysfunction only increase, so replenishment of dopaminergic deficiency is useful in mild cognitive disorders of any nature [11].
A drug that combines dopaminergic and adrenergic properties is piribedil (Pronoran), a D2/D3 receptor agonist and presynaptic alpha-2 adrenergic receptor antagonist. The combined effect enhances the nootropic effect and distinguishes Pronoran from other drugs of the group of dopamine receptor agonists. Its effect on cognitive functions is due to the following mechanisms:
- stimulation of dopaminergic transmission through activation of D2/D3 dopamine receptors in the limbic system and frontal cortex;
- increased noradrenergic transmission in these sections due to blockade of presynaptic alpha-2 adrenergic receptors;
- increased release of acetylcholine in the frontal cortex and dorsal hippocampus associated with blockade of alpha-2 adrenergic receptors [12].
Pronoran is considered a first-line drug for mild cognitive impairment, which has been confirmed in 14 clinical studies involving more than 7,000 patients. During treatment, an improvement in cognitive functions was observed (the condition was assessed using the Mini-Mental State Assessment Scale) [13, 14], a significant difference was noted in memory, attention, thinking (comprehension, reasoning, development of strategies and problem solving) [15], bioelectrical brain activity [16].
Russian scientists have carried out several large studies that examined the effectiveness of Pronoran in moderate cognitive disorders of vascular origin. In the PROMETHEUS study, which was already mentioned above, patients with dyscirculatory encephalopathy and moderate cognitive impairment were treated with Pronoran 50 mg/day. After 12 weeks of treatment, significant or moderate improvement in cognitive scores was observed in 67% of patients [17].
Improving cerebral and peripheral blood supply with the use of Pronoran is important for patients with cognitive impairment and cerebrovascular diseases [18]. Thanks to this property, Pronoran is also successfully used in the treatment of patients with peripheral circulatory disorders of the arteries of the lower extremities, ischemic circulatory disorders of the eyes and neurosensory deficits.
For the treatment of moderate cognitive impairment, high doses of the drug are not required. A dose of 50 mg/day, that is, one tablet, is considered sufficient, effective and safe, and is well tolerated by patients. After three months of treatment with Pronoran 50 mg/day, patients’ memory significantly improved, their level of wakefulness increased [19], and visual and auditory disorders and dizziness were less frequently recorded (in 41, 71 and 84% of patients, respectively) [20, 21]. Patients complained less of headaches, fatigue, forgetfulness, and noise in the head. There was a regression of depressive and anxiety symptoms [22–24].
In the multicenter study FUETE, a comparative assessment of the effectiveness of Pronoran and drugs with vasotropic and neurometabolic effects (piracetam, ginkgo biloba extract, vinpocetine) was carried out in patients with moderate cognitive impairment due to arterial hypertension and cerebral atherosclerosis. After two months of therapy, regression of subjective complaints and objectively detected cognitive disorders was noted in all compared therapeutic groups, but the improvement was significantly more pronounced in the Pronoran group [25].
Conclusion
Pronoran is considered a first-line drug for the treatment of mild cognitive impairment. The effectiveness and safety of its use (at the recommended dose of 50 mg/day) have been proven in a series of large multicenter placebo-controlled studies. Pronoran improves cognitive functions, including memory, in most patients, reduces astheno-depressive complaints and has a good effect on the condition of elderly people with neurosensory deficits.
It is recommended to start using this drug as early as possible, since Pronoran therapy is effective in pre-dementia stages of cognitive impairment.
In addition to the dopamine receptor agonist Pronoran, a number of drugs with neurotrophic, neurometabolic and vasoactive effects are widely used in the complex treatment of moderate cognitive disorders. The combination of Pronoran with other nootropic drugs is well tolerated and can provide additional positive effects.
Side effects
Adverse reactions are moderate in nature, develop mainly at the beginning of treatment and disappear after discontinuation of Pronoran.
- Digestive reactions: nausea, flatulence , vomiting.
- Reactions from nervous activity: agitation, confusion, hallucinations, dizziness, drowsiness, sudden falling asleep.
- Circulatory reactions: orthostatic hypotension, arterial hypotension , blood pressure lability.
- Allergic reactions: there is a risk of an allergy to the crimson dye included in the medicine.
- Behavioral disorders: addiction to gambling, compulsive overeating, increased libido, obsessive desire to make purchases, hypersexuality.
Instructions for use of Pronoran (Method and dosage)
It is recommended to take the tablets orally, after eating, without chewing and with 100 ml of water.
Pronoran, instructions for use
For monotherapy of Parkinson's disease, 150-250 mg of the drug per day is prescribed, divided into 3 doses. If you need to take 250 mg of Pronoran, it is recommended to divide the dose as follows: 100 mg is taken in the morning, another 100 mg is taken at lunch and 50 mg of the drug is taken in the evening.
For all other indications (excluding Parkinson's disease), the medicine is prescribed to take 50 mg once a day. If necessary, the dosage can be increased to 100 mg per day, divided into 2 doses in the morning and evening.
When used in combination with levodopa drugs, the daily dose is 150 mg, divided into 3 doses.
When selecting an upward dose, you need to titrate the dose, slowly increasing it by 50 mg every 14 days.
Release form
Controlled-release film-coated tablets, 50 mg.
15 tablets per blister (PVC/Al). 2 blisters with instructions for medical use per cardboard pack.
30 tablets each in a blister (PVC/Al). 1 blister with instructions for use is included in a cardboard box.
When packaging (packing) at the Russian enterprise Serdix LLC, 30 tablets are placed in a blister (PVC/Al), 1 blister with instructions for use in a cardboard pack.
Interaction
Concomitant use with antipsychotics (except Clozapine ) is contraindicated due to mutual antagonism of action.
Patients with extrapyramidal syndrome provoked by taking antipsychotics should be treated with anticholinergic drugs and it is not recommended to prescribe antiparkinsonian dopaminergic drugs .
The drug can cause or stimulate the development of psychotic disorders. If it is necessary to prescribe antipsychotics to persons with Parkinson's disease taking antiparkinsonian dopaminergic drugs, the dosage of the latter should be slowly reduced until complete withdrawal (the prohibition on abrupt withdrawal of these drugs is associated with the risk of neuroleptic malignant syndrome ).
Due to the mutual antagonism of antiparkinsonian dopaminergic drugs and Tetrabenazine , their combined use is not recommended.
Caution is recommended when using piribedil with other drugs that exhibit sedative effects.
Contraindications
increased individual sensitivity to piribedil and/or excipients included in the drug;
collapse;
acute myocardial infarction;
concomitant use with antipsychotics (except clozapine);
children under 18 years of age (due to lack of data).
With caution: due to the fact that the drug contains sucrose, patients with intolerance to fructose, glucose or galactose, as well as patients with sucrose isomaltase deficiency (a rare metabolic disorder), are not recommended to take the drug.
special instructions
In a number of patients (mainly those suffering from Parkinson's disease ), due to taking piribedil , a state of drowsiness may suddenly occur, or even suddenly fall asleep. This phenomenon is observed very rarely, but patients driving vehicles should be warned about the possibility of its development. If such reactions occur, consider reducing the dosage of piribedil or ending piribedil therapy.
Considering the age of patients receiving treatment with piribedil , the likelihood of falls caused by arterial hypotension , sudden falling asleep or confusion must be taken into account.
Patients and their caregivers should be warned about possible behavioral disorders (increased libido, gambling, compulsive overeating, hypersexuality, compulsive shopping) when using the drug. If such reactions occur, consider reducing the dosage of piribedil or ending piribedil therapy.
Analogues of Pronoran
Level 4 ATC code matches:
Pramipexole
Mirapex
Bromocriptine
The most common analogs of Pronoran are listed below: Bromocriptine-Richter, Azilect, Zymox, Duellin, Isikom, Credanil 25/250, Cognitiv Selegiline, Madopar, Benserazid, Midantan, Amantadine, Mendylex, Mirapek, Newpro, Pantogam, Nakom, Pantocalcin, Permax, PC -Merz, Parcon, Requip, Pramipexol-Teva, Modutab, Selegiline, Segan, Sinemet, Tasmar, Stalevo, Phenotropil, Eldepril, Cyclodol, Yumex.
Reviews about Pronoran
Reviews about Pronoran on forums are very few (partly because treatment with the drug is prescribed mainly to older people) and contradictory, which does not allow one to form a complete picture of the effectiveness of the drug. However, we can say that the occurrence of various kinds of side effects when taking the described drug is not a rare phenomenon. In any case, the selection and evaluation of the effectiveness of drugs, especially in the treatment of Parkinson's disease , should be carried out by an experienced specialist.
Price, where to buy
The price of Pronoran No. 30 is 510-700 rubles. In Ukraine, the cost of a standard package of the drug can reach 210 hryvnia.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
ZdravCity
- Pronoran tab. with counter.release.p.o.
50 mg n30 LLC Servier Rus 346 rub. order
Pharmacy Dialogue
- Pronoran tablets p/o 50 mg No. 30Servier
RUB 471 order
show more
Pharmacy24
- Pronoran 50 mg N30 tablets Lab.Serv e Industries, France
181 UAH order
Compound
| Controlled-release film-coated tablets | 1 table |
| active substance: | |
| piribedil | 50 mg |
| excipients: magnesium stearate - 5 mg; povidone - 20 mg; talc - 130 mg | |
| shell: carmellose sodium -0.71 mg; polysorbate 80 -0.3 mg; crimson dye Ponceau 4R - 3.87 mg; povidone - 6.31 mg; sodium bicarbonate -0.15 mg; colloidal silicon dioxide -0.27 mg; sucrose - 57.17 mg; talc - 50.37 mg; titanium dioxide - 0.78 mg; white beeswax - 0.07 mg |