Pancreatic cancer is a malignant tumor that is aggressive and prone to rapid growth into neighboring tissues. As the formation spreads, structural and functional disorders occur in the pancreas. Pancreatic cancer occupies a leading position among oncological diseases of the digestive organs. The number of diagnosed cases increases every year. Men suffer from the disease more often than women. Oncologists at the Yusupov Hospital diagnose pancreatic cancer using modern instrumental and laboratory research methods. They use equipment from leading Japanese, European and American manufacturers.
Doctors at the Oncology Clinic take an individual approach to choosing management tactics for each patient. Surgeons are fluent in the technique of radical and palliative surgical interventions. The use of the latest anticancer drugs can improve the quality and increase the life expectancy of patients. Medical staff provides professional care for patients.
Diagnostics
Diagnosis of pancreatic cancer at the Oncology Center is carried out in a complex that includes physical, laboratory and instrumental research methods:
- Palpation (palpation) of the abdominal organs. An examination of the patient by a doctor can detect an increase in the size of the abdominal organs, which may indicate the development of the disease.
- Ultrasound. The method makes it possible to see the location of the tumor, but is not very effective in the early stages of the disease.
- Endosonography is an ultrasound examination using an endoscope inserted through the mouth. Allows you to study the area under study from the closest possible distance and gives an accurate picture of the location of the tumor.
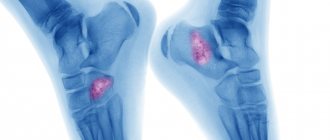
- X-ray research methods. Using radiographic methods, you can examine the size and location of the tumor, and examine internal organs for the presence of metastases.
- Blood chemistry. Pancreatic cancer changes the biochemical composition of the blood: enzymes and bile acids increase, protein levels decrease.
- CT scan of the abdomen with contrast. Allows you to clearly assess the extent of the tumor, its connection with the great vessels, and provides information about the possibility of radical surgery.
- MRI. Indicated for acid forms of tumor, for mucinous neoplasm of the pancreatic duct.
Pancreatic cancer is a malignant tumor that arises from the cells of the pancreas. Initially, it is asymptomatic and makes itself felt already in the later stages, when the disease is difficult to treat.
Synonyms Russian
Pancreatic adenocarcinoma, pancreatic carcinoma, pancreatic cancer.
English synonyms
Pancreatic Cancer, Cancer of the pancreas.
Symptoms
- Pain in the upper abdomen, radiating to the back.
- Yellowing of the skin and whites of the eyes.
- Diabetes.
- Loss of appetite.
- Weight loss.
- Depression.
- Blood clots.
Symptoms of cancer in 90% of cases begin to appear when the disease is already actively progressing: the tumor reaches a fairly large size, lymph nodes are affected, and metastases appear in the liver or lungs.
general information
Even when diagnosed early, pancreatic cancer has a poor prognosis. It is usually rarely diagnosed in time and develops quickly. Symptoms usually appear when surgery is no longer worthwhile.
The pancreas is a long, flat organ located in the upper abdomen behind the stomach. It produces enzymes that help the digestion process and hormones that regulate blood sugar levels.
The exact causes of pancreatic cancer have not yet been established.
After the gland cells degenerate into cancerous ones, they begin to multiply uncontrollably, forming a cancerous tumor when they accumulate.
Types of Pancreatic Cancer
- Pancreatic duct cancer. The cells lining the pancreatic ducts are affected. These cells produce enzymes that help with digestion. Most often, cancer is of this type. Tumors formed from these cells are called exocrine (adenocarcinomas).
- Cancer of the hormone-producing cells of the pancreas. This type of cancer is very rare and is called endocrine cancer.
Stages of development of pancreatic cancer:
1) the cancerous tumor is located within the pancreas;
2) cancer spreads beyond the pancreas to nearby tissues and organs, and can affect the lymph nodes;
3) cancer affects large blood vessels and lymph nodes outside the pancreas;
4) cancer affects the liver, lungs and peritoneum (the membrane that covers the inside of the abdominal cavity and organs).
Pancreatic cancer can lead to the following complications.
- Jaundice is due to a tumor blocking the extrahepatic bile ducts.
- Pain – when a growing tumor affects the nerves located in the abdominal cavity.
- Intestinal obstruction – the tumor puts pressure on the small intestine, blocking the flow of digested food from the stomach to the intestines.
- Weight loss. Due to the fact that there are fewer normally working pancreatic cells, it does not produce enough enzymes that help digestion. Nausea, vomiting and digestive problems can cause weight loss.
Who is at risk?
- Older people, especially after 60 years.
- People who are overweight or obese.
- Patients with pancreatitis (inflammation of the pancreas).
- Patients with diabetes.
- Patients who have already been diagnosed with pancreatic cancer.
- Those who have relatives who have survived pancreatic cancer.
- Smokers.
Diagnostics
Unfortunately, there are no tests that can detect pancreatic cancer in the early stages. Diagnosis is usually made in advanced stages using radiography, tomography and confirmed by biopsy.
Laboratory diagnostics:
- tumor marker CA 242,
- tumor marker CA 19-9,
- cancer embryonic antigen (CEA),
- total amylase in serum (amylase is secreted by the pancreas and is responsible for the digestion of carbohydrates; in pancreatic cancer, its level may increase),
- alkaline phosphatase and bilirubin (their increase may indicate blockage of the bile ducts by the tumor or the spread of the tumor into the liver tissue).
Analyzes for CA 242 and CA 19-9 have fairly high sensitivity and specificity, especially when high values are detected. However, their levels can also increase in other tumors of the gastrointestinal tract, and even in a healthy body. Therefore, the test for tumor markers is used as an auxiliary method for diagnosing cancer, as well as to detect relapses of cancer and to evaluate the effectiveness of its treatment.
Other diagnostic methods:
- ultrasound diagnostics,
- spiral computed tomography (CT) and magnetic resonance imaging (MRI),
- endoscopic retrograde cholangiopancreatography (ERCP),
- biopsy.
Treatment
The choice of cancer treatment strategy depends on the stage of the disease, the age of the patient, and the general state of his health.
First of all, if possible, it is necessary to eliminate the cancerous tumor.
If this is not possible, therapy is used to slow the progression of cancer and relieve its symptoms.
Treatment may include:
- surgical operation - in accordance with the location of the tumor, part of the pancreas, gall bladder, part of the duodenum, part of the bile duct, and spleen can be removed;
- radiation therapy - this uses radiation aimed at destroying cancer cells; it can be used before and after surgery;
- chemotherapy is the use of drugs that destroy cancer cells; chemotherapy can be combined with radiation therapy (chemoradiotherapy); Typically, chemoradiotherapy is used to treat cancer that has spread beyond the pancreas to nearby organs, and after surgery to reduce the risk of cancer recurrence.
- the appointment of enzymes to stimulate the digestion process - the function of the pancreas is inhibited, and it does not produce enough enzymes to help digestion.
Prevention
There are currently no known ways to prevent pancreatic cancer. However, you can reduce your risk of cancer by:
- quitting smoking;
- maintaining normal weight,
- physical activity (exercise at least 30 minutes daily),
- healthy diet (plenty of fruits, vegetables and whole grains).
Recommended tests
- CA 19-9
- CA 242
- Carcinoembryonic antigen (CEA)
- Serum total amylase
- Alkaline phosphatasase
- Bilirubin
Treatment
Treatment of pancreatic cancer is a complex task that requires prompt and coordinated actions between doctors and the patient.
In Oncology, the choice of technique depends on the stage of the disease and the presence of metastases. An integrated approach is used , combining chemotherapy and surgery (if the tumor is detected in the early stages). The operation involves partial or complete removal of the pancreas, as a result of which the patient is forced to take digestive enzymes and insulin for the rest of his life. The peculiarity of performing these operations in our oncology center is, on the one hand, maximum radicality (no-touch mobilization), on the other hand, minimal disability. A number of operations for pancreatic cancer are performed through punctures.
Read more about surgical treatment of pancreatic cancer.
Causes of pancreatic tumors
As with any other malignant diseases, pancreatic cancer is the result of a mutation in its epithelial cells. What exactly causes such mutations is still unclear. However, there are a number of factors that increase the risk of developing a tumor:
- various pathologies of the pancreas: chronic pancreatitis (its inflammation), diabetes mellitus, cysts, adenoma (benign tumor), etc.;
- smoking, which impairs blood supply to the pancreas;
- excess body weight associated with hormonal imbalance affecting gland cells;
- liver diseases, primarily cirrhotic lesions;
- peptic ulcer of the stomach and duodenum;
- nonspecific ulcerative colitis, Crohn's disease and other autoimmune diseases of the digestive system;
- improper diet with excessive consumption of sausages, fatty and fried foods, smoked meats, coffee, carbonated drinks, simple carbohydrates (sweets);
- low physical activity;
- various allergic pathologies, such as eczema, atopic dermatitis, etc.;
- oral diseases;
- chronic intoxications associated with poor environmental conditions or occupational hazards;
- tumor diseases of other organs and systems;
- age over 60 years;
- belonging to the Negroid race and male gender;
- some hereditary mutations (for example, in the BRCA2 or PKD1 gene);
- the presence of cancer pathologies in close relatives.
Risks of occurrence
Scientists have not yet established the exact cause of pancreatic cancer. The growth of a malignant neoplasm can begin under the influence of the following provoking factors:
- Excessive smoking – causes ischemia (oxygen starvation) of organ tissue;
- Excess of easily digestible carbohydrates in the diet creates additional stress on the gland;
- Chronic pancreatitis - the development of atypical cells occurs against the background of an uncontrolled inflammatory process in the pancreas;
- Excess body weight - fat deposits affect internal organs, including the pancreas, and additional load increases the risk of developing tumors;
- Chronic intoxication – long-term toxic effects negatively affect the structure and functions of the pancreas;
- Oral diseases - caries, periodontitis, periodontal disease, which significantly increase the risk of the formation of tumor foci in the pancreas.
The highest incidence of pancreatic cancer is typical for economically developed countries, which are characterized by urbanization and high socio-economic indicators. Malignant neoplasms develop with a burdened heredity.
Tumor cells from other organs affected by the tumor process metastasize to the pancreas. More than 75% of patients with pancreatic cancer have reached 70 years of age. However, the pathology also affects younger people.
Expert opinion
Author:
Alexey Andreevich Moiseev
Oncologist, chemotherapist
Pancreatic cancer is a malignant tumor that develops in the glandular tissue or ducts of the organ. The tumor very quickly destroys tissue and grows into neighboring organs, so it is important to know the main symptoms of the disease in order to consult a doctor in a timely manner.
According to doctors, the main cause of the tumor is a genetic failure at the cellular level. As a result, the affected cells cannot perform basic functions, but multiply intensively, which leads to the formation of a tumor. Medicine is unable to find the root cause of oncology and answer the question of what gives impetus to the degeneration of healthy cells into cancerous ones. Research has been conducted for many years, but no clear cause of the pathology has been found.
Provoking factors are considered to be smoking, excessive alcohol consumption, diabetes mellitus, surgical interventions on the gastrointestinal tract, and poor environmental conditions.
Not a single doctor will answer you how long a patient will live or whether a patient will live at one or another stage of pancreatic cancer. It all depends on the severity of the pathology, the extent of the damage, and the state of the patient’s body. Doctors at the Yusupov Hospital practice an integrated approach to diagnosing and treating pancreatic cancer in a hospital setting.
Make an appointment
Types of pancreatic cancer
Pancreatic tumors are classified according to the types of cells from which they develop. The following types of tumors are distinguished:
- ductal, which is the most common;
- glandular-squamous;
- squamous;
- giant cell;
- mucinous;
- acinar.
In some cases, the histological origin of the neoplasm cannot be established, and then the tumor is classified as undifferentiated. Loss of differentiation (“specialization” of cells) is a poor prognostic sign. Such neoplasms develop very aggressively and begin to metastasize early.
Classification
The classification of pancreatic cancer depends on the histological structure of the tumor and the location of the tumor. According to histological structure, malignant neoplasms of the pancreas are divided into:
- Squamous;
- Adenocarcinoma;
- Cystadenocarcinoma;
- Glandular-squamous;
- Unspecified cancer;
- Ductal adenocarcinoma.
The most common form of pancreatic cancer is adenocarcinoma. The tumor is formed from the epithelial cells of the ducts. It is accompanied by an intense fibrotic reaction. Cystadenocarcinoma has a generally favorable prognosis. Acinar cancer is observed in 5% of patients. Pancreatic sarcoma is a rare disease that is usually diagnosed in childhood.
In accordance with the location, cancer of the head, body, and tail of the organ is distinguished. In 65% of cases, the tumor is localized in the head of the pancreas, in 30% in the body and tail, and in 5% only in the tail. Malignant neoplasms of the head of the pancreas penetrate the duodenum. They obstruct the passage of the bile ducts, spread into the retroperitoneal space and peritoneal cavity, and form cysts. Tumors of the body and tail of the pancreas can penetrate the splenic vein, portal vein of the liver, and metastasize to the spleen and colon. Metastases of pancreatic cancer are often found in the liver, lungs and peritoneum.
The exocrine part of the pancreas has a well-developed network of lymphatic ducts that are located along the blood vessels. Tumors localized simultaneously in the tail and body of the pancreas spread through the lymphatic ducts.
Make an appointment
Localization of pancreatic cancer
Anatomically, this organ has three parts, each of which can be affected by a tumor. Accordingly, depending on the location it happens:
- gland head cancer. This is the most common type of pancreatic cancer, accounting for approximately 3/4 of all cases of this disease. Tumors of the head of the gland are usually smaller than tumors of other parts of the organ. But, since the head is located next to the bile ducts, it quickly begins to compress them. Therefore, a common symptom of pancreatic cancer in the early stages is the appearance of a icteric tint to the sclera and skin;
- gland body cancer. Tumors of this location account for about 18% of cases. Large neoplasms in this part of the gland often lead to compression of surrounding vessels, and therefore to disruption of the blood supply to nearby organs. In addition, due to damage to glandular tissue, these tumors are characterized by symptoms of diabetes mellitus;
- tail gland cancer. This is a fairly rare pathology that occurs in approximately 7% of cases of pancreatic malignancy. A special feature of this tumor is that it is difficult to detect on ultrasound, since the tail part of the gland is covered by organs such as the stomach, colon and lower parts of the lung.
Symptoms
The insidiousness of pancreatic cancer lies in the fact that the initial stages of the disease are practically asymptomatic. There is no severe pain or obvious manifestations of any abnormalities in health or discomfort. You should be wary and immediately visit a doctor if the following symptoms appear:
- Pain in the abdominal area, radiating to the back, increasing with changes in body position;
- Yellowness of the skin;
- A sharp decrease in body weight;
- Loss of appetite;
- Nausea and vomiting, dizziness, loose stools, weakness for no apparent reason.
With malignant tumors, the pain heads are usually localized in the epigastric region. If the tumor is located in the tail of the organ, patients complain of pain in the left upper quadrant of the abdomen. Gradually the pain becomes more severe and constant, intensifying at night. It can be localized in the back (when it grows into retroperitoneal structures).
The nature of the pain changes when changing position. The patient feels relief when bending the body forward. Exacerbation may occur during attacks of acute pancreatitis. Pain in the left half of the abdomen, constipation or signs of intestinal obstruction are caused by metastasis of cancer of the body or tail of the pancreas to the colon.
Acinar carcinoma is accompanied by a syndrome of focal inflammation and subcutaneous lipoid necrosis. It is characterized by joint pain and increased levels of eosinophils in the blood, high levels of lipase in the blood serum. Similar symptoms are characteristic of recurrent pancreatitis. A non-local manifestation of pancreatic adenocarcinoma is superficial thrombophlebitis of a migratory nature. When the portal vein is blocked, esophageal varices develop. It leads to stomach bleeding.
Over time, jaundice becomes one of the main symptoms of pancreatic cancer. It is detected in 90% of patients with tumor lesions of the head of the organ. Jaundice is progressive. Tumor remission may result in less jaundice. In case of cancer of the tail and body of the pancreas, jaundice is rarely recorded. With the development of cholangitis, body temperature rises.
Upon palpation, a volumetric formation is determined in the projection area of the pancreas. When the tumor is localized in the head of the organ, an enlarged, painless gallbladder is palpable in the right hypochondrium. Infection with abdominal metastases leads to the development of ascites (accumulation of free fluid in the abdomen).
Patients in most cases seek medical help when their condition sharply worsens. As a rule, at this stage the cancerous tumor is already significant in size.
Treatment at various stages
Specialists at our Oncology Center in Moscow develop treatment regimens for pancreatic cancer on a strictly individual basis. Doctors take into account the histological type of tumor, its location, the patient’s general health, etc. But the most important parameter is the stage of development of the oncological process.
The most effective method of treatment at the moment remains surgery. It is almost always supplemented with pharmacological and radiation therapy. In the early stages of the existence of a malignant neoplasm, it can be eliminated by operations of various scales:
- Whipple operation - removal of the head of the gland;
- segmental resection - removal of the body of the gland with subsequent connection of its remaining parts;
- distal resection – removal of the body and tail of the gland;
- total resection – removal of the entire gland.
These interventions will be effective on:
- stage zero (the tumor is represented by only a certain number of malignantly degenerated cells in one place);
- first stage (the tumor is entirely in the gland, without affecting either the lymph nodes or other organs):
- second stage (the tumor has spread to the tissues and lymph nodes surrounding the gland, but has not yet grown through the walls of neighboring large vessels).
Also, all nearby lymph nodes are often removed for preventive purposes. In addition, at the second stage, those parts of other organs into which the malignant process has managed to spread are also subject to excision: areas of the duodenum, stomach, gall bladder, etc.
At the third (tumor growth through the walls of large vessels) and fourth (metastases in distant organs) stages, palliative surgical interventions are mainly performed. Their goal is to improve the patient’s quality of life and eliminate the most severe symptoms of a pancreatic tumor. These can be operations on:
- removal of those parts of the tumor that put pressure on surrounding organs, disrupting their functions, or compress blood vessels and nerve pathways;
- removal of the largest metastases, often in combination with HIPEC (Hyperthermic Intra Peritoneal Chemotherapy), an innovative method of hyperthermic intraperitoneal chemotherapy for peritoneal carcinomatosis.
- elimination of obstruction of the biliary tract or intestines, including by applying stents and anastomoses;
- suturing pathological holes in the walls of adjacent hollow organs.
Conservative treatment
In the treatment of this malignant pathology, the administration of traditional cytostatic drugs is widely used. In addition, oncology today offers more effective means for the treatment of pancreatic cancer. This is, first of all, targeted therapy, in which the active substances of drugs act on specific target molecules of tumor cells, disrupting the processes of their growth and reproduction. Targeted treatment is highly selective, practically without affecting healthy tissue, and therefore produces much fewer side effects. In addition, radiation therapy also demonstrates some effectiveness for pancreatic tumors.
Before surgery, conservative therapy can be prescribed in order to slow down the growth of the tumor as much as possible and reduce its size, destroying as many malignant cells as possible. After surgery, the main point of using these methods is to combat possible metastases and relapses. And in the later stages of the development of the oncological process, when radical operations seem inappropriate, conservative therapy becomes the basis of treatment.
Prevention of pancreatic cancer
The following rules will help reduce the risk of this pathology:
- Quitting smoking and drinking alcohol.
- Reducing the amount of sweets, baked goods and fatty foods in the diet.
- Increasing the consumption of plant fiber.
- Normalization of body weight.
- Constant moderate physical activity.
- Use of personal protective equipment in hazardous industries.
- Periodic preventive examinations by a gastroenterologist for the timely detection and treatment of pathologies that are considered precancerous (pancreatitis, cysts and pancreatic adenomas).
List of sources:
- Hidalgo M. Pancreatic cancer. N Engl J Med. 2010;362(17):1605-1617.
- Li D, Xie K, Wolff R, et al. Pancreatic cancer. Lancet. 2004;363(9414):1049-57.
- National Cancer Institute. SEER stat fact sheets: pancreas cancer. NCI website. Published April 28, 2021.
- "Pancreatic Cancer Treatment (PDQ®) Patient Version." National Cancer Institute. National Institutes of Health. 17 April 2014.
- Ryan DP, Hong TS, Bardeesy N (September 2014). "Pancreatic adenocarcinoma". The New England Journal of Medicine. 371(11):1039–49.
- Bazin I.S. Basic principles of management of patients with pancreatic cancer // Effective pharmacotherapy. - 2014. - No. 47. - P. 10-17. — ISSN 2307-3586.
- Kubyshkin V. A. Pancreatic cancer. // Consilium medicum. Vol. 5, No. 8 (2003).
- Lockhart K., Rotenberg M. L. et al. Adjuvant cancer therapy. Per. from English N. D. Firsova (2017)