Dermographism is a greatly increased sensitivity of the skin to external irritants. From the slightest touch or too much pressure on the skin, pronounced traces of impact remain on its surface, which can appear in the form of red or white stripes. The type of dermatological disease is determined by their color, and the patient is subsequently diagnosed with red or white dermographism. The exact cause of the disease is still not known. It is believed that this is a type of urticaria, the appearance of which may be associated with external or internal irritants of the body.
Varieties of dermographism
There are 4 types of dermographism:
- Urticarial dermographism , which is also called edematous, is characterized by the appearance of a blistering rash, similar to the features of urticaria. However, the rashes are not accompanied by itching and burning, so they can be ignored by a person for a long time.
- Red dermographism , characterized by the appearance of pink or red stripes on the surface of the skin after a blunt object is passed over them. Sometimes hyperemic areas of the epidermis may have white outlines. The stripes do not last long - only 2-3 hours, then they disappear on their own.
- White dermographism , in which white stripes appear on the body. They are stored for several minutes.
- Reflex dermographism , which occurs after passing a sharp object across the skin. The stripes are bright red and vary in length.
If a person’s health condition is normal, then doctors allow the development of red dermographism of the skin. The most severe (in terms of treatment) is the urticarial type of disease.
Types of dermographism
Depending on the clinical picture, several types of disease are distinguished:
- White dermographism. In the corresponding zone of skin irritation, whitish stripes appear within 3-5 seconds after a small impact on it, which disappear in a few minutes.
- Edema dermographism. At the site of physical irritation, oblong edematous ridges 5–15 mm wide and 1–2 mm high appear. The swelling increases gradually, sometimes over several hours, and disappears very slowly.
- Red dermographism. Characteristic signs are the formation of red hyperthermic stripes in the area of direct skin irritation. They appear 15 minutes after mechanical impact. In the chronic course of the disease, traces remain for an hour or two. The acute stage is characterized by an increase in the time of manifestation of the disease to 1–3 days.
- Urticarial dermographism. It is the most common type of dermographism, accounting for 15% of all skin diseases. With urticarial dermographism, in addition to stripes and spots, an itchy rash appears on the irritated skin.
Which doctors should you visit?
All forms of dermographism are treated by a dermatologist.
- Gastroenterologist - to exclude gastritis, dysbacteriosis, colitis. If the patient has constipation, you need to find out the cause.
- Parasitologist. It is necessary to exclude infection with worms, protozoa, lamblia, and opisthorchiasis.
- Endocrinologist. Rule out diabetes (donate blood for sugar), check the functioning of the thyroid gland (blood for hormones).
- Immunologist - to determine the general condition of the immune system. If necessary, take a course of immunomodulators.
Additional research by specialists in different fields of medicine will help differentiate the causes of red dermographism and pathologies of other internal organs.
Causes of dermographism
Persistent red dermographism, accompanied by skin hyperemia, as in atopic dermatitis, is not dangerous to humans. Redness of the epidermis that occurs in response to mechanical damage is an absolutely normal phenomenon, unless it is accompanied by itching, burning and peeling.
The reasons for this deviation lie in the abnormal activity of the parasympathetic division of the ANS, and may be associated with a disturbance in the metabolic process caused, for example, by thyrotoxicosis.
The causes of white dermographism are vasospasm. This type of reaction can occur in any person, but people suffering from hypertonicity of the sympathetic division of the ANS are most susceptible to it.
Edematous dermographism develops against the background of allergic reactions, when tissue swelling occurs when allergens penetrate through the membranes of mast skin cells.
Factors predisposing to the development of white, edematous, reflex and red dermographism are:
- nervous tension, stress;
- chronic diseases of the nervous system;
- alcoholism;
- long-term exposure to chemical elements on the body;
- frequent cases of hypothermia.
Red dermographism may not be an independent disease, but one of the signs of pathologies of the nervous system, and even meningitis. For this reason, the diagnosis and treatment of the disease should be carried out exclusively by a doctor.
Etiology
Red dermographism is nothing more than a reaction of the skin to thermal, mechanical and other external influences, against the background of which red marks appear on the skin that persist for quite a long period of time.
The reasons for the development of pathology remain not fully understood, however, among the predisposing factors are:
- prolonged exposure to low or high temperatures;
- friction of the skin against tight clothing;
- shocks and other impacts;
- exposure to stress and nervous strain;
- genetic predisposition;
- the course of allergic processes.
In addition, it is generally accepted that the development of such a disease is influenced by the state of the gastrointestinal tract, which is why the sources of the disease can be considered:
- chronic constipation;
- dysbacteriosis;
- gastritis of any nature;
- pathological influence of helminths, lamblia and other protozoa;
- disruption of the functioning of the thyroid gland, which often happens when it is partially removed;
- Gluten intolerance.
Prevalence
Collecting information about how much humanity suffers from this condition is complicated by the fact that not everyone notices something unusual in the reaction of their skin, and even fewer people consider it necessary to contact doctors if abnormalities are detected. In this regard, data on how common red dermographism is is difficult to call sufficiently accurate. Researchers talk about 2-5%, but in reality the percentage is most likely higher.
Red dermographism in children occurs quite often at an early age. It can be quite intense and diffuse, but is mainly due to the fact that their skin is more delicate and sensitive and at the same time prone to irritation. However, children are more often diagnosed with other skin diseases (for example, urticaria or dermatitis), rather than red dermographism.
Diagnostics
Diagnosing dermographism is much easier than any other skin disease. To record the fact of a sharp reaction of the epidermis to mechanical stress, it is enough for the doctor to run a medical spatula over it.
If small vesicles have formed on the surface of the skin, the dermatologist can additionally scrape their tissues for serological testing. This is a differential diagnostic method, which is carried out in order to distinguish dermographism from other diseases accompanied by the formation of watery blisters.
Diet therapy
The selection of nutrition for each patient is individual and should be carried out by a nutritionist. Although there are general rules, for example, you should avoid eating spicy and fatty foods, smoked and salty foods, and do not abuse spices, alcohol and carbonated drinks. To enrich your diet, you should include more greens, vegetables, and fresh fruits.
Folk remedies are also suitable for eliminating the causes and treating red dermographism (see photo below). The most effective were: raw potatoes, nettles and raspberry roots; olive oil; sage and string; valerian and celandine; St. John's wort and chamomile. Decoctions are prepared from herbs, roots and leaves, which are taken orally or used as lotions (especially potatoes).
Treatment with folk remedies
To treat red dermographism, especially its mild form, you do not need to use specific techniques. It will be enough to use traditional medicine products, in this case they can provide significant help. Below are recommendations from healers for combating dermographic urticaria.
Morning tea and coffee for patients with urticarial dermographism should be replaced with a decoction of the series. The herb is brewed like regular tea. You can drink the decoction throughout the day, and not just in the morning. In addition to the series, teas brewed with black currant and garden raspberry leaves, rose hips, mint and yarrow are suitable for such patients.
Fresh celery juice will help get rid of the symptoms of dermographic urticaria. You can prepare it using a juicer, or simply grate the root on a fine grater and squeeze through cheesecloth. To achieve maximum effect, you should drink at least 1/3 glass of this juice per day. You can also make vegetable cocktails by adding carrot, cucumber or beet juice to celery.
Features of the treatment of dermographism
Treatment of a disease such as dermographism should be carried out under the supervision of a physician. But the therapy used will not help to completely cure the pathology if its causes have not been established. And since this is exactly what happens in the vast majority of cases, the attending physician can prescribe medications that will only temporarily remove the unpleasant symptoms.
Drug treatment involves the use of:
- antibiotics (rare);
- antiseptics;
- antiallergic (antihistamine) drugs;
- hypertonic or hypotonic drugs.
Only a doctor should treat dermographism with pharmaceutical medications, since it is almost impossible to choose a suitable remedy on your own. More precisely, this should not be done so as not to cause a more aggressive reaction of the body.
Oral administration of medications (except antihistamines) in the fight against dermographism is inappropriate. In this situation, only topical products (ointments, creams, gels) can help.
Treatment
Treatment of dermographism is carried out only in case of severe manifestations, accompanied by itching. Drug therapy is aimed at eliminating local symptoms and treating the underlying disease.
Prescribed:
- antiallergic drugs (to reduce skin irritation);
- tranquilizers and antidepressants (Diazepam, Phenazepam, Doxepin, Paxil);
- drugs with a sedative effect, including vitamin B;
- ascorbic acid, flavonoids (vitamin P, Rutin) (to reduce the permeability of vascular walls);
- vasoconstrictors (for red and vasodilators for white dermographism);
- antipruritic ointments;
- Ketotifen (in the presence of urticarial dermographism);
- choleretic drugs;
- lactobacilli and bifidobacteria;
- external antiseptics based on camphor and salicylic acid.
Sometimes exposure to ultraviolet light has a positive effect.
With the help of timely identification of the causes that provoke dermographism and their elimination, it is possible to achieve stable remission, and in some cases, completely get rid of such manifestations.
Therapy
In mild cases (90%), there is no need to treat such a disorder. Marks on the skin disappear on their own after some time and do not leave scars. To relieve symptoms, take sedative antihistamines of the 1st generation: suprastin, diphenhydramine.
But in severe chronic forms, non-sedating antihistamines of the 2nd generation (loratadine) or 3rd generation (cetirizine) are prescribed. They are taken once when manifestations occur or regularly for persistent relapses. For prevention, ketotifen is prescribed; it prevents histamine from entering the tissue.
Prevention measures
To avoid the development of dermographism, it is necessary:
- wear comfortable clothes made from natural fabrics;
- try to rub your skin with a washcloth as little as possible while taking a shower or bath;
- use hypoallergenic hygiene products;
- do not overcool and do not overheat;
- keep your skin clean;
- walk outdoors more often.
To restore the skin after an illness, it is necessary to enrich the menu with products containing vitamins. In particular, the body needs vitamin C, which activates the immune system, giving it the strength to fight pathological processes.
Drinking fluids (adults - 2 liters per day, preschool children - 1 liter) restores the structure of skin tissue and moisturizes the epidermis.
Proper skin care significantly reduces the risk of developing dermographism and other dermatological diseases. That is why the rules of child hygiene must be taught from early childhood.
There are no similar articles.
Did you like the article?
Prevention and prognosis
To avoid symptoms, you need to follow a few simple rules:
- avoid contact with allergens;
- avoid stress;
- reduce the effect of cold and hot temperatures on the skin;
- normalize the rest and wakefulness regime;
- stop wearing tight clothes;
- regularly perform hygiene procedures;
- undergo a full clinical examination several times a year to identify pathologies of the gastrointestinal tract or endocrine system that can cause such a disease.
The prognosis for red dermographism is favorable in most cases - complete recovery can be achieved.
What is urticaria?
This is a dermatological disease caused by a certain irritant, which is accompanied by the following symptoms: the skin turns red and swells, blisters 0.1-1.0 cm in size appear on it. The lesions resemble nettle burns, they bother the patient: they hurt, burn, itch.
Urticaria is a common disease. In children it is more often acute, while adults suffer from a chronic form.
There are 2 ways of developing pathology:
- Immune. Ordinary substances upon first contact with the body, due to improper functioning of the immune system, are perceived by it as hostile - it begins to produce antibodies. Upon repeated contact, the antibodies begin to fight the irritant, causing harm to the person himself - characteristic allergy symptoms appear.
- Non-immune. Antigens (for example, antibiotics) in this case do not require repeated contact, they will immediately provoke antibodies to attach to mast cells and release histamine.
Types of pathology
There are several types depending on the factor that provokes the reaction. Types of urticaria
| View | Provocateur of reaction |
| cold | low temperatures |
| solar | ultraviolet radiation: sun, solarium |
| thermal | heated object |
| cholinergic | overheating of the body, heavy physical activity, stress |
| aquagenic | water |
| contact | natural fabrics, wool and particles of animal epidermis, some plants, cosmetics, topical medications |
| medicinal | medications, in particular antidepressants, non-steroidal anti-inflammatory drugs, acetylsalicylic acid, antibiotics |
| food | products |
| dermographic | mechanical effect on the skin |
| idiopathic | unknown origin: the irritant can be cold, heat, stress, medications, foods |
General notes on therapy
Treatment Goals
- regression of rashes;
- no relapses.
Diet.
- In case of a proven food allergy, it is recommended to avoid eating foods that provoke the development of the disease. Eliminating identified allergens from the diet leads to an improvement in the condition of the skin after 24-48 hours.
- In patients with daily or almost daily urticaria, it is recommended that a hypoallergenic diet be included in the extensive evaluation plan. In the case of a pseudo-allergic reaction, improvement with a hypoallergenic diet occurs after 3 weeks.
Pharmacological drugs
.
- Non-sedating 2nd generation H1-histamine blockers are recommended as basic first-line therapy for acute and chronic urticaria.
- The use of 1st generation H1-histamine blockers is currently limited due to their low effectiveness and the risk of side effects (sedation, anticholinergic effects, sleep disorders, etc.) and is indicated only in a number of exceptional cases.
- Treatment of acute urticaria with glucocorticosteroid drugs is not recommended. Indications for the use of systemic glucocorticosteroids are: lack of effect when treated with H1 receptor blockers, delayed urticaria due to pressure, angioedema.
- It is not recommended to use, due to very low evidence of effectiveness: H2-receptor blockers (both monotherapy and in combination with H1-histamine blockers), montelukast, zafirlukast, tranexamic acid, sodium cromoglycate, topical corticosteroids, colchicine, indomethacin, nifedipine.
Indications for hospitalization
to the dermatological hospital: widespread urticaria, accompanied by intense itching and a disturbance in the general condition, as well as lack of effect at the outpatient stage of therapy. to the intensive care unit: concomitant angioedema in the larynx, anaphylactic reactions
Requirements for treatment results
- stopping the appearance of fresh rashes;
- complete resolution of existing rashes;
- absence of subjective manifestations of the disease.
Prevention
Prevention of urticaria involves a thorough analysis of the allergy history before prescribing drug treatment. Particular attention should be paid to the manifestations of atopy in patients with urticaria. For preventive purposes, the use of 2nd generation H1-histamine blockers is recommended [8]. For patients with chronic urticaria, it is important to sanitize foci of chronic infection, treat concomitant pathologies, and also limit the effect of potential allergens.
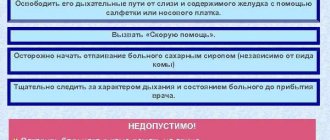
Acute urticaria
- Eliminate exposure to trigger factors.
- Carry out drug therapy aimed at relieving the symptoms of the disease:
- treatment with H1-histamine receptor blockers;
- if there is no effect, treatment with systemic glucocorticosteroid drugs;
- urgent measures to relieve angioedema.
Chronic urticaria
- Elimination of exposure to factors that cause exacerbation of the disease (if possible).
- Hypoallergenic diet with the exclusion of suspected allergens and/or obligate allergens. When eliminating a food allergen from the diet, the condition improves after 1-2 days. When the rashes disappear, a gradual introduction of excluded or new foods begins, one at a time, one every other day, until new rashes appear. The ineffectiveness of the elimination diet for 1 month indicates the absence of a connection between urticaria and food products and serves as an indication for canceling the elimination diet.
- Drug therapy aimed at reducing symptoms of the disease.
Algorithm for drug treatment of patients with chronic urticaria.
| First line of therapy: | H1-histamine blockers 2nd generation |
| Symptoms persist for 2 weeks | |
| Second line of therapy: | Increasing the dose of 2nd generation H1-histamine blockers by 4 times* |
| Symptoms persist for 1-4 weeks | |
| Third line of therapy: | Omalizumab |
| A short (maximum 10-14 days) course of glucocorticosteroid drugs can be administered at any time. Indication: severity of exacerbation | |
* it is required to justify the prescription in doses exceeding those specified in the instructions for the use of drugs, to invite the patient or his legal representative to sign an informed consent, explaining the benefits and risks of such a prescription, to approve the prescription by a medical commission.
2nd generation H1-histamine blockers are effective in 40-60% of patients with chronic spontaneous (idiopathic) urticaria. If there is no effect from treatment with them for 2 weeks, a 4-fold increase in the dose of drugs is possible. Increasing the dose of H1-histamine receptor blockers allows you to limit the use of glucocorticosteroid drugs and, thus, avoid side effects of therapy and steroid resistance.
Features of the treatment of individual forms of urticaria
- Cold urticaria
. Patients should avoid sudden exposure to cold temperatures. 2nd generation antihistamines (rupatadine) can be used. Systemic glucocorticosteroid drugs are ineffective. - Delayed pressure urticaria
. Pressure on the skin should be avoided. For severe delayed urticaria from pressure, the most effective are systemic glucocorticosteroid drugs, which are prescribed for a short period of time with a gradual reduction in dose. Histamine H1 receptor blockers are usually ineffective. - Solar urticaria
. Antihistamines and ultraviolet light irradiation in gradually increasing doses are effective (tolerance induction). Adequate photoprotection (UVA+UVB) is important. - Urticarial dermographism
. No treatment is required unless the patient consistently responds to minimal trauma. 1st generation H1-histamine receptor blockers are effective. In some cases, the disease is severe and continuous therapy with 2nd generation antihistamines is required. - Cholinergic urticaria
. Patients should avoid intense physical activity. 1st and 2nd generation H1-histamine receptor blockers are used. Belladonna alkaloids/phenobarbital/ergotamine and radobelin/phenobarbital/ergotamine are indicated for the treatment of cholinergic urticaria. - Contact urticaria.
Avoid contact with provoking factors. Antihistamines are effective methods of therapy. Preventive administration of 2nd generation H1 histamine blockers is acceptable in cases of possible contact with trigger factors (for example, insect bites). Topical glucocorticosteroid drugs may be prescribed. For severe manifestations of the disease, systemic glucocorticosteroid drugs are used. - Thermal, aquagenic, vibration urticaria.
Antihistamines are not always effective. - Angioedema
. With the development of angioedema, epinephrine is administered parenterally (intravenously, intramuscularly or subcutaneously, depending on the severity and location of the lesion) and H1-histamine receptor blockers (intravenously or intramuscularly). If this therapy is ineffective and in cases of the development of severe angioedema with a violation of the general condition, systemic glucocorticosteroid drugs are used. In cases of difficulty breathing, aminophylline is used. - Adrenergic urticaria.
Avoid contact with provoking factors, oral propranolol. Nonspecific therapy, including tranquilizers and antihistamines.
Treatment regimens
1. 2nd generation H1-histamine receptor blockers
- Loratadine 10 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- desloratadine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- fexofenadine 180 mg orally 1 time per day until the rash disappears and 4 weeks after the rash disappears
- Cetirizine 10 mg orally once daily or 5 mg orally twice daily until the rash disappears and 4 weeks after the rash disappears
- Levocetirizine 5 mg orally once a day until the rash disappears and 4 weeks after the rash disappears
- ebastine 10-20 mg orally 1 time per day (depending on the severity of symptoms) until the rash disappears and 4 weeks after the rash disappears
- Rupatadine 10 mg orally once a day until the rash disappears and 4 weeks after the rash disappears.
2. First generation H1-histamine receptor blockers
- diphenhydramine 25-50 mg orally 4-6 times a day or 20-50 mg intramuscularly 1-2 times a day for 7-10 days
- clemastine 1 mg orally 2 times a day or 2 mg intramuscularly 2 times a day for 7-10 days chloropyramine 25 mg orally 1-2 times a day or 20-40 mg intramuscularly 1-3 times a day for 7-10 days
- cyproheptadine 2-4 mg orally 3-4 times a day for 7-10 days
3. Glucocorticosteroid drugs
- betamethasone 1-2 ml intramuscularly with an interval of 7-10 days, 1-2 injections
- dexamethasone 4-16 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- dexamethasone 1.5-4.5 mg per day orally until pronounced clinical improvement occurs, with a further gradual dose reduction of 0.125-0.25 mg once a week until complete withdrawal
- prednisolone 30-100 mg per day intravenously or intramuscularly until pronounced clinical improvement occurs, with further transition to oral administration (except for the treatment of angioedema)
- prednisolone 10-30 mg per day orally until pronounced clinical improvement occurs, with a further gradual reduction in dose by 2.5-5 mg once a week until complete withdrawal.
4. Adrenergic agonists
For severe urticaria and/or angioedema (laryngeal edema, exercise-induced anaphylaxis, severe cold allergy), epinephrine, a solution of 0.1% (0.1 to 0.3 ml), is administered subcutaneously or intramuscularly, if necessary, the administration is repeated after 10 -20 minutes up to 3 times.
5. Omalizumab
The drug is indicated for the treatment of chronic idiopathic urticaria, resistant to therapy with H1-histamine receptor blockers, in patients aged 12 years and older. The recommended dose of the drug for chronic idiopathic urticaria is 300 mg subcutaneously every 4 weeks. It is recommended that the attending physician periodically evaluate the need for continued treatment. The effect of omalizumab, as a rule, can be observed already in the first day, with its subsequent increase over a number of weeks. According to clinical studies and real clinical practice, the effectiveness of omalizumab reaches 90%.
Treatment of angioedema (Quincke's edema)
- epinephrine, solution 0.1%: 0.1-0.5 ml intravenously or intramuscularly, or subcutaneously once;
- chloropyramine, or clemastine, or diphenhydramine 1-2 ml intravenously or intramuscularly once;
- prednisolone 60-100 mg intravenously or intramuscularly or dexamethasone 8-16 mg intravenously or intramuscularly until pronounced clinical improvement;
- aminophylline 10 ml of 2.4% solution intravenously, slowly, once.
Related treatments
In the treatment of urticaria, drugs that affect the central nervous system are used as concomitant therapy: anxiolytics (tranquilizers) and antidepressants.
1. Anxiolytics (tranquilizers) for cholinergic urticaria:
- Hydroxyzine 25 mg orally 4 times a day with meals for 7-10 days
- belladonna alkaloids/phenobarbital/ergotamine 1 tablet orally 2-3 times a day for 1 month
- radobelin/phenobarbital/ergotamine 1 tablet orally 3 times a day for at least 1 month.
2. Antidepressants as concomitant therapy for patients with urticaria in the presence of depression and anxiety.
- amitriptyline 25-50 mg orally 1 time per day for at least 1 month.
3. External therapy. To reduce itching and burning, use warm showers and baths, lotions, shaken suspensions with menthol, anesthetics that do not contain glucocorticosteroid drugs.
Open recommendations
- Some experience has been accumulated in the use of cyclosporine A in combination with 2nd generation H1 histamine blockers for chronic urticaria.
- There are few studies showing the effectiveness of plasmapheresis in chronic urticaria of autoimmune origin.
- The latest consensus documents on the treatment of urticaria also recommend leukotriene receptor blockers, 2nd generation H1 histamine blockers in combination with omalizumab, ketotifen, dapsone, sulfasalazine, oxatamide, nifedipine, warfarin, intravenous gammaglobulin, autologous plasma, montelukast. However, this therapy has low-quality evidence, with no efficacy data from high-quality randomized clinical trials (CDs) [26–29, 34–43].
Treatment of pregnant women and during lactation
When managing pregnant and lactating women, you should adhere to rules similar to those when managing children. It is important to avoid the use of any systemic drug during pregnancy, especially in the first trimester, but the most effective treatment should be ensured. There are indications of an increase in histamine levels in pregnant women, which determines the need for the use of antihistamines. Prescription of 2nd generation H1-histamine blockers during pregnancy should only be used if necessary, when the expected benefit to the mother outweighs the possible risk to the fetus. In the first trimester, medications should be avoided.
A low dose of loratadine may be used for a short time. Use of 1st generation H1-blockers immediately before birth may cause respiratory depression and other side effects in newborns.
To date, there is not a single indication in the world of congenital pathology in children born to women who took 2nd generation H1-histamine blockers (cetirizine, loratadine) during pregnancy. It is advisable to prescribe loratadine to pregnant women with urticaria; recommendations for loratadine can be extrapolated to desloratadine. Recent clinical observations have shown that the safest drugs during pregnancy are loratadine, and during lactation, loratadine and cetirizine [45].
Treatment during lactation.
It is necessary to avoid taking medications during breastfeeding. If necessary, loratadine and cetirizine can be used.
Treatment of children
In children, acute urticaria is more often recorded, which can manifest itself as an allergic reaction, for example, to food. The disease usually develops within an hour after eating food and resolves within 24 hours. Chronic urticaria is less common among children than among adults. In childhood, the most commonly reported urticaria are pressure urticaria and cold urticaria, which are often combined with dermographic or cholinergic urticaria. In most cases, the positive effect of therapy is achieved by taking antihistamines and eliminating trigger factors. For children, 1st line of therapy is recommended, similar to that for adults. It is important to consider the age restrictions and age dosages of each of the H1-histamine blockers:
- loratadine: children aged 2 to 12 years with body weight less than 30 kg - 5 mg 1 time per day, children over 12 years old, and also with body weight more than 30 kg - 10 mg 1 time per day;
- Levocetirizine: children aged 2 to 6 years - 2.5 mg per day, children over 6 years - 5 mg per day;
- Cetirizine: children over 6 years of age (weighing more than 30 kg) - 1 tablet 1 time per day.
Desloratadine, fexofenadine, rupatadine are approved for use in children aged 12 years and older. In infants and children under 2 years of age, first generation H1-histamine receptor blockers can be prescribed. In rare cases, the use of systemic glucocorticosteroid drugs is allowed (for 3-5 days ) .
Possible complications
If dermographism is accompanied by severe itching, then when scratching the areas of the epidermis affected by rashes, there is a high risk of bacterial or viral infection. This could be herpes, human papillomavirus, streptococcal or staphylococcal microflora, etc.
If you do not pay attention to the manifestations of dermographism, this can lead to the development of complications. These include:
- exhaustion of the nervous system;
- damage and thinning of the dermis;
- the introduction of infection and the development of inflammatory processes in places where skin rashes and blisters occur;
- Quincke's edema, anaphylactic shock (in rare cases).
General characteristics of the disease
Direct determination of dermographism as a diagnosis is not difficult - this is easily done by pronounced characteristic manifestations on the skin during a visual examination and testing the skin for mechanical impact. However, this dermatological pathology is rarely an independent disease - most often it is one of the symptoms of the underlying disease.
Diseases that cause dermographism pose a particular danger to a child. They can lead to the development of the following negative consequences:
- damage to various internal organs;
- decreased motor ability;
- changes in hormone levels;
- metabolic disorders at the cellular level;
- change in blood formula;
- disability, asphyxia, death.
Therefore, when the first signs of dermographism appear in children, you should immediately contact your pediatrician. Self-medication is strictly forbidden. Only qualified medical care can provide quality treatment and prevent the development of complications.
The term “dermography” comes from the words derma - skin and grapho - write. Translated from Greek, it means “skin writing” or “skin writing.” In a person suffering from dermographism, the skin is indeed constantly “painted” with various symbols, similar to mysterious inscriptions. They are formed even from minor exposure to seams on clothing, folds of bed linen, or touching with a blunt object. These can be stripes of different sizes and shapes, characterized by slight swelling and redness or paleness of the skin.
With dermographic urticaria, the pressure mark is distinguished not only by a more pronounced change in color, but also by swelling of the skin with itchy rashes on it. Such symptoms persist for several hours or days.
Therefore, when the first signs of dermographism appear in children, you should immediately contact your pediatrician. Self-medication is strictly forbidden. Only qualified medical care can provide quality treatment and prevent the development of complications. Before treating dermographism, a child or adult patient first undergoes a differential examination to identify or exclude the most likely diseases:
- exhaustion, disorder or intoxication damage to the nervous system;
- psoriasis, other dermatoses;
- vegetoneurosis, vegetative-vascular dystonia;
- hyperthyroidism;
- meningitis, disorders of the central nervous system;
- disturbances of sympathetic innervation;
- parasitic infestations;
- increased swelling;
- exposure to allergens;
- hormonal imbalances;
- metabolic disorders;
- autoimmune, cardiovascular pathologies;
- infectious processes in the body;
- hereditary predisposition.
To identify the cause of dermographism, the following are prescribed:
- laboratory tests of blood and feces for the presence of parasites;
- blood test for hormone levels;
- encephalogram of the brain to establish the functionality of the central nervous system;
- immunogram to check the state of the immune system;
- allergy tests;
- Ultrasound of internal organs,
- tomography, x-ray;
- biopsy.
Based on the results of diagnostic studies, the root cause of skin hypersensitivity is determined and a course of treatment is prescribed.
Symptoms of red dermographism
Even by the name of the disease, you can determine that the main clinical symptom is red spots on the skin. When mechanically applied to the skin of a healthy person, some changes are visible. First, the skin at the site of exposure turns white, then turns red, and after some time it acquires a normal color. And there are cases when the patient experiences persistent redness or paleness of the skin. This condition is called white or persistent red dermographism. Most patients no longer report other pathological symptoms. However, in isolated cases, patients complain of severe skin itching at the site of redness; when scratching this area, minor pain, blisters, wounds and rashes of unknown etiology are added. Often, patients are not as concerned about skin manifestations as they are about psychological discomfort. They are embarrassed by the very fact that they have such a pathology. The causes of red dermographism in children, adolescents and adults are not fully understood. Rashes and redness on the skin last from several hours to several days. As a rule, they disappear on their own and without a trace, unless, of course, there is the influence of additional factors. No complications were identified with such a disease as red dermographism (photo below).