Causes of pathology
Fibrillation and ventricular flutter occur due to the pathology of impulse transmission through the myocardium.
These rhythm disturbances are successive stages of the development of one process. In ICD-10 (International Classification of Diseases, 10th revision) they are classified under one heading. Dysfunction of the cardiac pathways can occur as a result of:
- large scar (consequence of myocardial infarction);
- focal post-infarction cardiosclerosis;
- coronary heart disease;
- acute myocardial infarction;
- cardiomyopathy with severe hypertrophy of cardiomyocytes;
- dilatation (stretching of the walls) of the heart chambers;
- arrhythmogenic cardiomyopathy;
- myocarditis (inflammation of the heart muscle);
- valve defects;
- severe intoxication (including alcoholism).
Symptoms and signs of ventricular fibrillation
VF is a life-threatening condition. It develops suddenly, and the victim very quickly develops a picture of clinical death. However, if it is preceded by ventricular flutter (contraction of muscle fibers with a frequency of more than 200 times per minute), the patient may have time to complain about:
- chest pain;
- sensation of accelerated heartbeat (2-3 times per second or more);
- dizziness, loss of orientation in space;
- nausea, which may progress to vomiting;
- increased sweating;
- disturbed rhythm and difficulty breathing;
- general weakness.
These symptoms may last no more than 15-20 seconds. When VF develops, the patient loses the ability to speak coherently. During inspection, you need to pay attention to:
- unconscious state;
- pallor of the skin with acrocyanosis (bluish color of the earlobes, tip of the nose);
- convulsive muscle contractions (occur 35-45 seconds after the onset of the attack, may be accompanied by involuntary urination or defecation);
- a state of clinical death that will occur 2 minutes after the onset of VF if help is not provided: dilation of the pupils (normally they narrow if a person raises their eyelids in a bright room, but here opening the eyes does not cause a physiological reaction);
- it will be impossible to feel the pulse (both on the radial artery (peripheral, runs at the wrist) and on the main ones (large: carotid, femoral);
- breathing movements will stop.
However, to confirm the diagnosis, it is necessary to conduct an instrumental study - electrocardiography.
Ventricular fibrillation - Treatment in Switzerland
Sudden cardiac arrest is characterized by a sudden cessation of cardiac activity. The cause of this in almost all cases is ventricular fibrillation of the heart. At the same time, the heart rate increases sharply to more than 300 beats per minute. This leads to the stopping of the pumping function of the heart. The supply of oxygen to the body suddenly stops. The brain reacts to this by losing consciousness within a few seconds.
Only prompt action and immediate first aid can save lives in such a situation. Ventricular fibrillation should be stopped as quickly as possible using a defibrillator. If a defibrillator is located nearby, non-specialists should also be able to use it. It is easy to use and each defibrillator comes with illustrated instructions for use. If there is no defibrillator nearby, the patient must be given first aid in the form of cardiac massage and, if necessary, artificial respiration before the ambulance arrives. At the same time, cardiac massage, according to recent studies, is much more important than artificial respiration. Therefore, the new instructions recommend that persons providing first aid themselves limit themselves to cardiac massage and not perform artificial respiration. Cardiac massage, however, should be performed without cautious expectancy, pressing forcefully with both hands on the chest 5-6 cm from the chest bone with a frequency of 100 to 120 times per minute. Don't be afraid to hurt the patient. As a result of cardiac massage, blood circulation in the body is restored, and this is extremely important for the survival of the victim. Possible injuries received during cardiac massage will not play a significant role. Cardiac massage should continue until the doctor arrives.
After successful resuscitation, a search for the causes of ventricular fibrillation begins, after which appropriate treatment is prescribed. Often the actual cause of ventricular fibrillation is coronary heart disease with circulatory disorders. To prevent further cases of ventricular fibrillation, portable defibrillators can be implanted that sense the heart rhythms characteristic of ventricular fibrillation and then respond immediately. For more details, see Chapter “Surgical treatment of cardiac arrhythmias.”
How does the disease manifest itself on an electrocardiogram?
Ventricular fibrillation on an ECG (electrocardiogram) has several stages of development:
- Ventricular flutter. Lasts several seconds, myocardial contractions are still coordinated. On the ECG it appears in the form of high-amplitude (with a large distance between the upper and lower bending points) rhythmic waves (there can be 250-300 such complexes per minute).
- Convulsive stage. The high-amplitude waves remain, but now their frequency is on the order of six hundred per minute. This is a manifestation of chaotic uncoordinated contraction of individual sections of the myocardium lasting 55-65 seconds.
- Ventricular fibrillation. Deterioration of contractility leads to dissociated contraction of individual groups of cardiomyocytes. The ECG records small (low-amplitude) waves with a frequency exceeding 100 per minute.
- Atonic stage. The energy reserve of the myocardium is almost completely exhausted. There are damped contractions of individual sections of the heart muscle. The waves become even lower and smaller, now their frequency does not exceed 400 per minute.
Photos and examples of film with VF
Let's look at examples of electrocardiographic films and descriptions of them.
- Ventricular flutter
- Stages: convulsive;
- ventricular fibrillation;
- atonic.
Publications in the media
Ventricular fibrillation (VF) is a form of cardiac arrhythmia characterized by complete asynchrony of contraction of individual fibers of the ventricular myocardium, causing loss of effective systole and cardiac output. VF means circulatory arrest and is equivalent to death if cardiac resuscitation is not performed.
More than 90% of cardiac arrests are caused by VF , so chest compressions, electrical defibrillation, mechanical ventilation and drug therapy are started immediately before ECG confirmation.
Classification • By frequency - flicker and flutter • • Ventricular fibrillation - irregular waves with a frequency of up to 400-600 per minute of various amplitudes and shapes ••• Small-wave VF - wave amplitude less than 5 mm ••• Large-wave VF - amplitude exceeds 5 mm • • Ventricular flutter is a regular, sinusoidal waveform with a frequency of up to 300 per minute. The main symptom is the absence of an isoelectric line. VF usually begins after an attack of paroxysmal ventricular tachycardia or early extrasystole (with ischemic heart disease) • By the presence of concomitant pathology •• Primary VF (usually due to acute coronary insufficiency) - 50% of all deaths from ischemic heart disease. In 30% of patients brought out of this state using electrical defibrillation (high efficiency), relapse of VF occurs within a year •• Secondary VF is usually manifested by small-wave ventricular fibrillation and occurs in patients with severe damage to the heart and blood vessels (extensive MI, dilated cardiomyopathy, decompensated heart disease, stroke), with chronic pulmonary heart failure, cancer. The effectiveness of defibrillation is low.
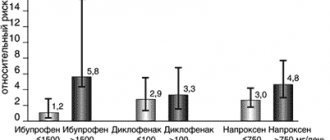
Etiology • Myocardial infarction or ischemia • Ventricular paroxysmal tachycardia • Intoxication with cardiac glycosides • Electrolyte disturbances • Electrical shock Hypothermia • Coronary angiography • strophanthin K), sympathomimetics (epinephrine, orciprenaline, salbutamol), barbiturates, anesthetics ( cyclopropane, chloroform), narcotic analgesics, TAD, phenothiazine derivatives (chlorpromazine, levomepromazine), amiodarone, sotalol, class I antiarrhythmic drugs.
Clinical manifestations - see Cardiac arrest.
TREATMENT - see also Cardiac arrest • Defibrillation is the main method of treating VF (first shock - 200 J, second - 300 J, third - 360 J) • Epinephrine 1 mg IV (if there is no effect, the injection is repeated every 5 minutes) • Repeated a series of defibrillation (3 times 360 J) - 1 minute after the administration of epinephrine • Lidocaine 50-100 mg IV bolus, if there is no effect after 5 minutes, the dose should be repeated.
Reduction . VF - ventricular fibrillation.
ICD-10 • I49 . 0 Ventricular fibrillation and flutter
Treatment and algorithm for helping with VF
Since VF is a condition that poses an immediate threat to the patient’s life, there is a documented protocol for action when such a paroxysm occurs. Since the patient is often treated after the transition to a state of clinical death, it all begins with resuscitation.
If a person is found during a convulsive period of VF, then all that needs to be done is to gently restrain the head from hitting the underlying surface. You can add folded clothing to mitigate their effects. It is forbidden to open the victim’s mouth, take out his tongue or hold his limbs.
Urgent actions
Algorithm of actions in order of priority:
- Check the patient’s consciousness: call by voice; if he does not respond, lightly shake his shoulders (so that the head does not come off the surface on which it lies and does not fidget on it; the direction of movement is from top to bottom).
- Assess for the presence of a pulse. To do this, it is recommended to clasp the central part of the neck (trachea) in the upper half with the fingers of one hand.
- If there is no pulse, call an ambulance (or have someone do it).
- Check for breathing. You need to lean your cheek towards the victim’s mouth and nose, observing the amplitude of movements of the chest and at the same time feeling the air movement (if present) with the skin. If necessary, clear the airway.
- Perform indirect cardiac massage (in this situation this is the most important) and artificial respiration.
When the emergency medical team arrives, they:
- continue to carry out resuscitation measures;
- connect a cardiac monitor and defibrillator (in modern models these two devices are combined);
- after recording an electrocardiogram and confirming the presence of VF, defibrillation is performed (discharges are delivered with increasing intensity every 2 minutes, against the background of chest compressions, until the rhythm normalizes);
In the absence of a defibrillator, it was previously recommended to perform a precordial blow (with a fist on the lower third of the sternum), but due to injuries and complex technique, it is now not recommended for use.
- if necessary, the following medications are administered: adrenaline;
- amiodarone;
- lidocaine.
What treatment should a patient with ventricular fibrillation receive?
Emergency care for ventricular fibrillation must include defibrillation. Waves of depolarization roll chaotically through the myocardium, and therefore performing chest compressions or using medications will most likely be ineffective.
When the patient is restored to sinus (normal) rhythm through the efforts of the ambulance team, there remains a risk of relapse. To reduce the risk of a recurrent attack, the following medications are prescribed:
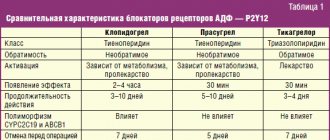
| Group of drugs | Representatives | Destination purpose |
| Antiarrhythmic | Lidocaine Amiodarone | Prevention of recurrence of ventricular fibrillation immediately after an attack |
| Bisoprolol Nebivolol | Maintaining an adequate heart rate in the long term | |
| Oral anticoagulants | Warfarin Rivaroxaban | Preventing the formation of blood clots and embolism (blockage) of blood vessels |
| Infusion therapy | Stereofundin Ringer's Lactate Trisol Chlosol Sodium Bicarbonate | Restoring the body’s water-electrolyte balance (it ensures adequate processes of excitation and contraction in the heart cells) |
Are there surgical techniques?
- Implantation of a cardioverter-defibrillator. This device is attached near the left collarbone, and electrodes from it are guided to the heart. It monitors the regularity of your heart rate. When VF paroxysm occurs, this device delivers a shock.
- Coronary angioplasty (stenting of coronary arteries). If VF occurs against the background of coronary heart disease, this surgical operation will remove the very cause of the paroxysm and prevent relapse.
- Coronary artery bypass grafting (bypass routes to restore blood flow in the basin of one of the coronary arteries). It makes sense if the onset of VF was preceded by an ischemic attack.
Prehospital cardiopulmonary resuscitation
What are the most common causes of sudden death? What can be done in cases of respiratory and circulatory arrest at the prehospital stage? Why is the intracardiac route of drug administration the “path of despair”?
Cardiopulmonary resuscitation is a set of measures aimed at reviving the body in the event of circulatory and/or respiratory arrest. Timely (within the first minutes) initiation of resuscitation measures can prevent irreversible brain damage and, possibly, the onset of biological death.
Most cases of sudden death have a cardiac cause.
The main signs of circulatory arrest are loss of consciousness, cessation of breathing and absence of a pulse (the presence of a pulse in the carotid arteries should be assessed).
Cardiopulmonary resuscitation (CPR) has two main parts.
- Basic resuscitation measures (BR) or non-specific resuscitation. It is carried out regardless of the cause of circulatory arrest and includes maintaining blood circulation (external cardiac massage with a frequency of 80-100 compressions per minute should be performed by placing the patient on a hard surface), as well as ensuring airway patency and a sufficient level of ventilation of the lungs (artificial ventilation - 12 breaths per minute using mouth-to-mouth, mouth-to-nose methods or using a breathing bag). Resuscitation should begin with inhalation, and then, if resuscitation is carried out by one person, perform 12-15 compressions per 2 breaths, and if there are two people - 5 compressions per breath. The probability of saving the patient's life in the event of circulatory arrest is inversely proportional to the time elapsed before the start of resuscitation measures.
The algorithm of actions when conducting ORM is presented in Fig. 1.
- Specialized resuscitation measures - the use of drugs and resuscitation equipment, depending on the reasons that caused circulatory arrest. These activities do not exclude, but complement the ORM.
Methods of drug administration during CPR
Intravenous. With established peripheral venous access, it is possible to administer drugs into a peripheral vein, but after each bolus administration it is necessary to raise the patient's hand to speed up the delivery of the drug to the heart, accompanying the bolus with the introduction of a certain amount of fluid (to push it). In order to provide access to the central vein, it is preferable to catheterize the subclavian or internal jugular vein. The introduction of drugs into the femoral vein is associated with their slow delivery to the heart and a decrease in concentration.
Endotracheal. If tracheal intubation is performed before venous access is ensured, then atropine, adrenaline, lidocaine can be administered with a probe into the trachea. In this case, the drug is diluted in 10 ml of physiological solution, and its dose should be 2–2.5 times greater than for intravenous administration. The end of the probe should be below the end of the endotracheal tube; after administering the drug, it is necessary to perform 2-3 consecutive breaths (while stopping the indirect cardiac massage) to distribute the drug throughout the bronchial tree.
Intracardiac. The “path of despair” is used only if no other route of administration is possible. If possible, you should refrain from intracardiac injections, since when using this method, large coronary arteries are damaged in 40% of cases.
Resuscitation tactics for ventricular fibrillation and hemodynamically ineffective ventricular tachycardia
It is necessary to begin resuscitation with ORM and electrical defibrillation (EDF). Defibrillation begins with a discharge with a power of 200 J. If fibrillation persists, a discharge is used again, but at a higher power - 200-300 J, then - 360 J. Resuscitation measures should not be started immediately with a discharge of maximum power in order to avoid damaging effects on the myocardium.
If the above measures are ineffective, ORM is resumed, the trachea is intubated, venous access is established, and adrenaline is administered at a dose of 1 mg every 3-5 minutes; Increasing doses of adrenaline 1-3-5 mg every 3-5 minutes or intermediate doses of 2-5 mg every 3-5 minutes can be administered. Adrenaline can be replaced with vasopressin, which is administered in a dosage of 40 mg into a vein once.
If ventricular fibrillation continues, antiarrhythmic drugs are used to reduce the defibrillation threshold:
- lidocaine 1.5 mg/kg intravenous bolus, repeated administration after 3-5 minutes, in case of restoration of blood circulation, a continuous infusion of lidocaine is established at a rate of 2-4 mg/min;
- amiodarone 300 mg into a vein over 2-3 minutes, if there is no effect, another 150 mg into a vein can be administered; in case of restoration of blood circulation, a continuous infusion is established in the first 6 hours of 1 mg/min (360 mg), in the next 18 hours 0.5 mg/min (540 mg);
- procainamide at a dosage of 100 mg; if necessary, the administration is repeated after 5 minutes (up to a total dose of 17 mg/kg);
- magnesium sulfate 1-2 g for 5 minutes; if necessary, administration can be repeated after 5-10 minutes for pirouette tachycardia.
After administering the drug, ORM is performed for 30-60 seconds, and then EDF is repeated (during this time the antiarrhythmic reaches the target). It is recommended to alternate the administration of drugs with DF according to the following scheme: antiarrhythmic - EDF (360 kJ) - adrenaline - EDF (360 kJ) - antirhythmic - EDF (360 kJ) - adrenaline, etc. You can use not one, but three discharges of maximum power . The number of EDFs is not limited.
The algorithm of actions for ventricular fibrillation is presented in Fig. 2.
The previously widely practiced administration of sodium bicarbonate (as a means of combating acidosis) is now used much less frequently due to limited indications:
- prolonged (more than 15 minutes) resuscitation measures;
- poisoning with tricyclic antidepressants;
- severe acidosis;
- hyperkalemia.
Sodium bicarbonate is administered at a dose of 1 mEq/kg into a vein (on average 140–180 ml of a 4% solution).
Tactics for electromechanical dissociation
Electromechanical dissociation (EMD) is the absence of pulse and breathing in a patient with preserved electrical activity of the heart (the rhythm is visible on the monitor, but there is no pulse).
Unfortunately, the prognosis for this type of cardiac dysfunction is poor if the cause that caused the circulatory arrest (acidosis, hypovolemia, hypoxia, hypothermia, cardiac tamponade, tension pneumothorax) is not eliminated.
Treatment of EMD includes ORM, intravenous administration of adrenaline - 1 mg every 3-5 minutes and atropine 1 mg every 3-5 minutes, cardiac pacing, and administration of sodium bicarbonate at the 15th minute of resuscitation. It is necessary to try to eliminate the cause of EMD.
Tactics for asystole
The tactics for eliminating this cause of circulatory arrest are practically no different from the treatment regimen for EMD. It is necessary to pay attention to the fact that an ECG in one lead with small-wave ventricular fibrillation can simulate extrasystole, so asystole must be confirmed in several ECG leads. Electrical defibrillation in this case is not only not indicated, but is even harmful, since it increases vagotonia. Treatment includes ORM, adrenaline is injected into a vein - 1 mg every 3-5 minutes, atropine - 1 mg every 3-5 minutes, electrical cardiac stimulation is performed, and at the 15th minute of resuscitation, the administration of sodium bicarbonate is indicated. It is necessary to try to eliminate the cause of asystole. The algorithm of actions for asystole is presented in Fig. 3.
Conclusion
In case of successful resuscitation measures, it is necessary:
- make sure that there is adequate ventilation of the lungs (airway patency, symmetry of breathing and chest excursion; assess the color of the skin, if you have a pulse oximeter, make sure that oxygen saturation is at least 90%);
- continue the administration of antiarrhythmics for prophylactic purposes;
- try to identify what pathological condition led to circulatory arrest and begin treatment of the underlying disease.
A. L. Vertkin, Doctor of Medical Sciences, Professor O. B. Talibov, Candidate of Medical Sciences O. N. Tkacheva MGMSU, NNPOSMP, Moscow
How does VF affect the duration of future life?
If defibrillation is successful (and it is more effective in large-wave forms of VF), the patient survives and the prognosis for future life is relatively favorable.
During ventricular fibrillation, the myocardium is more susceptible to damage (large infarction) as a result of lack of oxygen (hypoxia). This may increase the risk of sudden death, especially if:
- there is atherosclerotic damage to the coronary arteries;
- chronic physical inactivity is observed;
- the patient smokes;
- he drinks alcoholic beverages often and in large quantities;
- are overweight or obese;
- the person suffers from diabetes;
- arterial hypertension is present, and basic drug therapy is not used.
With properly selected antiarrhythmic therapy, the prognosis for life is favorable.
conclusions
Irregular contraction of individual muscle bundles in the ventricular myocardium causes their fibrillation. Without immediate cardioversion (restarting the rhythm), the likelihood of sudden cardiac death is very high.
The clinic is nonspecific: the patient is found unconscious, pale, often with no pulse, no breathing, and dilated pupils. The criterion for diagnosis is a characteristic electrocardiographic pattern (waves of different amplitudes).
Specific therapy is defibrillator discharge. In the future, drug and surgical (if necessary) treatment makes sense.