Artificial respiration (AR) is an urgent emergency measure if a person’s own breathing is absent or impaired to such an extent that it poses a threat to life. The need for artificial respiration may arise when providing assistance to those who have received sunstroke, drowned, suffered from electric current, as well as in case of poisoning with certain substances.
The purpose of the procedure is to ensure the process of gas exchange in the human body, in other words, to ensure sufficient saturation of the victim’s blood with oxygen and the removal of carbon dioxide from it. In addition, artificial ventilation has a reflex effect on the respiratory center located in the brain, as a result of which independent breathing is restored.
Mechanism and methods of artificial respiration
Content:
- Mechanism and methods of artificial respiration
- Indications and contraindications
- Preparing for artificial respiration
- Artificial respiration from mouth to mouth
- Artificial respiration from mouth to nose
- How long does artificial respiration last?
- Features of the procedure in children
- Manual methods of artificial respiration
- Hardware artificial respiration methods
- Complications of artificial respiration
Only through the process of breathing does a person’s blood become saturated with oxygen and carbon dioxide is removed from it. After air enters the lungs, it fills the lung sacs called alveoli. The alveoli are pierced by an incredible number of small blood vessels. It is in the pulmonary vesicles that gas exchange takes place - oxygen from the air enters the blood, and carbon dioxide is removed from the blood.
If the body's supply of oxygen is interrupted, vital activity is at risk, since oxygen plays the “first fiddle” in all oxidative processes that occur in the body. That is why, when breathing stops, artificially ventilating the lungs should be started immediately.
The air entering the human body during artificial respiration fills the lungs and irritates the nerve endings in them. As a result, nerve impulses are sent to the respiratory center of the brain, which are a stimulus for the production of response electrical impulses. The latter stimulate contraction and relaxation of the diaphragm muscles, resulting in stimulation of the respiratory process.
Artificially supplying the human body with oxygen in many cases makes it possible to completely restore the independent respiratory process. In the event that cardiac arrest is also observed in the absence of breathing, it is necessary to perform a closed cardiac massage.
Please note that the absence of breathing triggers irreversible processes in the body within five to six minutes. Therefore, timely artificial ventilation can save a person’s life.
All methods of performing ID are divided into expiratory (mouth-to-mouth and mouth-to-nose), manual and hardware. Manual and expiratory methods are considered more labor-intensive and less effective compared to hardware methods. However, they have one very significant advantage. They can be performed without delay, almost anyone can cope with this task, and most importantly, there is no need for any additional devices and instruments, which are not always at hand.
The essence and meaning of cardiac massage
The purpose of cardiac massage is to artificially recreate and replace cardiac activity if it stops. This can be achieved by squeezing the cavities of the heart from the outside, which imitates the first phase of cardiac activity - contraction (systole) with further weakening of pressure on the myocardium, which imitates the second phase - relaxation (diastole).
This massage can be done in two ways: direct and indirect. The first is possible only with surgery, when there is direct access to the heart. The surgeon takes it in his hand and performs a rhythmic alternation of compression and relaxation.
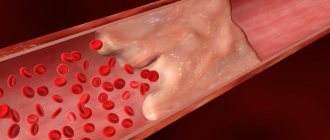
Indirect cardiac massage is called indirect because there is no direct contact with the organ. Compression is applied through the chest wall, as the heart is located between the spine and the sternum. Effective pressure on this area can release about 60% of the blood volume into the vessels compared to self-contracting myocardium. Thus, blood will be able to circulate through the largest arteries and vital organs (brain, heart, lungs).
Indications and contraindications
Indications for the use of ID are all cases where the volume of spontaneous ventilation of the lungs is too low to ensure normal gas exchange. This can happen in many urgent and planned situations:
- For disorders of the central regulation of breathing caused by impaired cerebral circulation, tumor processes of the brain or brain injury.
- For medicinal and other types of intoxication.
- In case of damage to the nerve pathways and neuromuscular synapse, which can be caused by trauma to the cervical spine, viral infections, the toxic effect of certain medications, and poisoning.
- For diseases and damage to the respiratory muscles and chest wall.
- In cases of lung lesions of both obstructive and restrictive nature.
The need to use artificial respiration is judged based on a combination of clinical symptoms and external data. Changes in pupil size, hypoventilation, tachy- and bradysystole are conditions that require artificial ventilation. In addition, artificial respiration is required in cases where spontaneous ventilation is “turned off” with the help of muscle relaxants administered for medical purposes (for example, during anesthesia for surgery or during intensive care for a seizure disorder).
As for cases where ID is not recommended, there are no absolute contraindications. There are only prohibitions on the use of certain methods of artificial respiration in a particular case. So, for example, if venous return of blood is difficult, artificial respiration modes are contraindicated, which provoke even greater disruption. In case of lung injury, ventilation methods based on high-pressure air injection, etc., are prohibited.
Emergency assistance from the medical team: what is the algorithm of action?
To provide emergency care in case of sudden cardiac arrest, a special cardiology team arrives on site, whose task is to carry out advanced resuscitation measures and immediately transport the patient to the hospital. It works according to a protocol that includes the following sequence of actions:
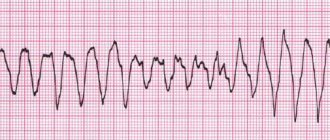
- Checking vital signs and making a diagnosis. For this purpose, a wider arsenal of equipment is used, including an electrocardiograph. It is necessary to exclude other causes of clinical death, such as bleeding or blockage.
Resumption of conductivity of the upper respiratory tract. To ensure maximum oxygen supply, they are intubated.- Resuscitation measures are carried out according to the same algorithm as indicated above, but for mechanical ventilation they use breathing masks, an Ambu bag or a ventilator.
- In the presence of atrial fibrillation or ventricular fibrillation on the ECG, the question of using defibrillation is raised.
- Drug support is provided by intravenous or intracardiac administration of drugs such as Adrenaline (1 ml 0.1% in 19 ml NaCl 0.9%) and Cordarone (in the presence of arrhythmias, 300 mg IV).
Preparing for artificial respiration
Before performing expiratory artificial respiration, the patient should be examined. Such resuscitation measures are contraindicated for facial injuries, tuberculosis, poliomelitis and trichlorethylene poisoning. In the first case, the reason is obvious, and in the last three, performing expiratory artificial respiration puts the person performing resuscitation at risk.
Before starting expiratory artificial respiration, the victim is quickly freed from clothing squeezing the throat and chest. The collar is unbuttoned, the tie is undone, and the trouser belt can be unfastened. The victim is placed supine on his back on a horizontal surface. The head is tilted back as much as possible, the palm of one hand is placed under the back of the head, and the other palm is pressed on the forehead until the chin is in line with the neck. This condition is necessary for successful resuscitation, since with this position of the head the mouth opens and the tongue moves away from the entrance to the larynx, as a result of which air begins to flow freely into the lungs. In order for the head to remain in this position, a cushion of folded clothing is placed under the shoulder blades.
After this, it is necessary to examine the victim’s oral cavity with your fingers, remove blood, mucus, dirt and any foreign objects.
It is the hygienic aspect of performing expiratory artificial respiration that is the most delicate, since the rescuer will have to touch the victim’s skin with his lips. You can use the following technique: make a small hole in the middle of a handkerchief or gauze. Its diameter should be two to three centimeters. The fabric is placed with a hole on the victim’s mouth or nose, depending on which method of artificial respiration will be used. Thus, air will be blown through the hole in the fabric.
The essence and algorithm of massage
External cardiac massage is a rhythmic compression of the heart by compression between the sternum and the spine. Experts note that the chest of a person with cardiac arrest becomes more pliable due to loss of muscle tone, making it easy to perform compressions. The person providing assistance, if the NMS technique is followed, can easily displace the chest by three to five centimeters. Compression of the heart leads to a decrease in its volume and an increase in intracardiac pressure.
Rhythmic pressure on the chest area results in a difference in pressure inside the heart cavities, the blood vessels that extend from the heart muscle. Blood from the left ventricle travels through the aorta to the brain, while from the right ventricle it flows to the lungs, where it is oxygenated.
After the pressure on the chest stops, the heart muscle straightens, intracardiac pressure decreases, and the chambers fill with blood. As a result, artificial circulation is recreated.
You can perform a closed massage of the heart muscle only on a hard surface. The person must be placed on the floor. After this, it is necessary to perform the so-called precordial punch. It should be directed to the middle third of the chest. The impact height should be thirty centimeters. However, according to recent data, the value of the precordial stroke is significantly reduced, and many experts do not recommend starting resuscitation measures with it. In order to conduct a closed cardiac massage, the person providing assistance places the palm of one hand on the other, after which he begins to carry out uniform pushes according to the established technique.
Artificial respiration from mouth to mouth
To perform artificial respiration using the mouth-to-mouth method, the person who will provide assistance must be on the side of the victim’s head (preferably on the left side). In a situation where the patient is lying on the floor, the rescuer kneels. If the victim's jaws are clenched, they are forced apart.
After this, one hand is placed on the victim’s forehead, and the other is placed under the back of the head, tilting the patient’s head back as much as possible. Having taken a deep breath, the rescuer holds the exhalation and, bending over the victim, covers the area of his mouth with his lips, creating a kind of “dome” over the patient’s mouth. At the same time, the victim’s nostrils are pinched with the thumb and index finger of the hand located on his forehead. Ensuring tightness is one of the prerequisites for artificial respiration, since air leakage through the victim’s nose or mouth can nullify all efforts.
After sealing, the rescuer quickly, forcefully exhales, blowing air into the airways and lungs. The duration of exhalation should be about a second, and its volume should be at least a liter for effective stimulation of the respiratory center to occur. At the same time, the chest of the person receiving assistance should rise. If the amplitude of its rise is small, this is evidence that the volume of air supplied is insufficient.
Exhaling, the rescuer unbends, freeing the victim's mouth, but at the same time keeping his head thrown back. The patient should exhale for about two seconds. During this time, before taking the next breath, the rescuer must take at least one normal breath “for himself.”
Please note that if a large amount of air enters the patient's stomach rather than the lungs, this will significantly complicate his rescue. Therefore, you should periodically press on the epigastric region to empty the stomach of air.
Rules for external cardiac massage
If the victim does not have a pulse, in order to maintain the vital functions of the body (to restore blood circulation), it is necessary, regardless of the reason that caused the cessation of heart function, to perform external cardiac massage simultaneously with artificial ventilation (artificial respiration). It should be borne in mind that without correct and timely preliminary assistance to the victim, the assistance of the arriving doctor may turn out to be late and ineffective.
External (indirect) massage is performed by rhythmic compression through the anterior wall of the chest while pressing on the relatively mobile lower part of the sternum, behind which the heart is located. In this case, the heart is pressed against the spine, and blood from its cavities is squeezed into the blood vessels. By repeating pressure at a frequency of 60-70 times per minute, you can ensure sufficient blood circulation in the body in the absence of heart function.
To carry out external cardiac massage, the victim should be laid with his back on a hard surface (low table, bench or floor), his chest should be exposed, and his belt, suspenders and other items of clothing that would restrict breathing should be removed. The person providing assistance should stand on the right or left side of the victim and take a position in which a more or less significant bend over the victim is possible. Having determined the position of the lower third of the sternum, the person providing assistance should place the upper edge of the palm of the hand extended to the fullest on it, and then put the other hand on top of the hand and press on the victim’s chest, while slightly helping by tilting his body.
Pressing should be done with a quick push so as to move the lower part of the sternum down towards the spine by 3-4 cm, and in obese people - by 5-6 cm. The pressure when pressing should be concentrated on the lower part of the sternum, which, due to its attachment to the cartilaginous ends the lower ribs are movable. The upper part of the sternum is fixedly attached to the bony ribs and can break if pressure is applied to it. You should also avoid pressing on the end of the lower ribs, as this can lead to their fracture. In no case should you press below the edge of the chest (on soft tissues), as you can damage the organs located here, primarily the liver. Pressing on the sternum should be repeated approximately 1 time per second.
After a quick push, the arms remain in the achieved position for approximately one-third of a second. After this, the hands should be removed, freeing the chest from pressure to allow it to expand. This favors the flow of blood from the large veins into the heart and its filling with blood.
Since pressing on the chest makes it difficult to expand during inhalation, inflation should be done in the intervals between compressions or during a special pause provided every 4-6 compressions on the chest.
If the person providing assistance does not have an assistant and is forced to perform artificial respiration and external cardiac massage alone, the above operations should be alternated in the following order: after 2-3 deep blows into the victim’s mouth or nose, the person providing assistance makes 4-6 pressures on the chest , then again makes 2-3 deep breaths and again repeats 4-6 pressures to massage the heart, etc.
If there is an assistant, one of those providing assistance - less experienced in this matter - should perform artificial respiration by insulating air as a less complex procedure, and the second - more experienced - should perform external cardiac massage. In this case, air injection should be timed to coincide with the end of pressure on the chest or interrupting cardiac massage for the duration of inflation.
If the persons providing assistance are equally qualified, it is advisable for each of them to perform artificial respiration and external cardiac massage, alternately replacing each other every 5-10 minutes. Such alternation will be less tiring than continuously performing the same procedure, especially cardiac massage.
The effectiveness of external cardiac massage is manifested primarily in the fact that each pressure on the sternum leads to the appearance of a pulsating oscillation of the artery walls in the victim (checked by another person).
When artificial respiration and cardiac massage are performed correctly, the victim will show the following signs of recovery:
- improvement in complexion, acquiring a pinkish tint instead of the gray-sallow color with a bluish tint that the victim had before receiving assistance;
- the appearance of independent respiratory movements, which become more and more uniform as assistance (resuscitation) measures continue;
- constriction of the pupils.
The degree of pupil constriction can serve as the most reliable indicator of the effectiveness of the assistance provided. The narrow pupils of the person being revived indicate a sufficient supply of oxygen to the brain, and the beginning dilation of the pupils indicates a deterioration in the blood supply to the brain and the need to take more effective measures to revive the victim. To do this, you should also raise the victim’s legs approximately 0.5 m from the floor and leave them in the raised position during the entire time of external cardiac massage. This position of the victim’s legs promotes better blood flow to the heart from the veins of the lower body. To support your legs in an elevated position, you should put something under them.
Artificial respiration and external cardiac massage should be carried out until spontaneous breathing and heart function appear, however, the appearance of weak sighs (in the presence of a pulse) does not provide grounds for stopping artificial respiration. In this case, as already mentioned above, the injection of air should be timed to coincide with the moment the victim begins to inhale.
The recovery of the victim’s heart activity is judged by the appearance of his own regular pulse, which is not supported by massage. To check the pulse, interrupt the massage for 2-3 seconds, and if the pulse persists, this indicates that the heart is working independently. If there is no pulse during the break, the massage must be resumed immediately.
It should be remembered that even a short-term cessation of revitalizing activities (1 minute or less) can lead to irreparable consequences.
After the first signs of revival appear, external cardiac massage and artificial respiration should be continued for 5-10 minutes, timing the insufflation to coincide with the moment of one’s own inhalation.
Artificial respiration from mouth to nose
This method of artificial ventilation is carried out if it is not possible to properly unclench the patient’s jaws or there is an injury to the lips or oral area.
The rescuer places one hand on the victim’s forehead and the other on his chin. At the same time, he simultaneously throws back his head and presses his upper jaw to the lower. With the fingers of the hand that supports the chin, the rescuer must press the lower lip so that the victim’s mouth is completely closed. Taking a deep breath, the rescuer covers the victim’s nose with his lips and forcefully blows air through the nostrils, while watching the movement of the chest.
After artificial inspiration is completed, you need to free the patient's nose and mouth. In some cases, the soft palate may prevent air from escaping through the nostrils, so when the mouth is closed, there may be no exhalation at all. When exhaling, the head must be kept tilted back. The duration of artificial exhalation is about two seconds. During this time, the rescuer himself must take several exhalations and inhalations “for himself.”
How long does artificial respiration last?
There is only one answer to the question of how long ID should be carried out. You should ventilate your lungs in this mode, taking breaks for a maximum of three to four seconds, until full spontaneous breathing is restored, or until the doctor appears and gives other instructions.
At the same time, you should constantly ensure that the procedure is effective. The patient's chest should swell well, and the facial skin should gradually turn pink. It is also necessary to ensure that there are no foreign objects or vomit in the victim’s respiratory tract.
Please note that due to the ID, the rescuer himself may experience weakness and dizziness due to a lack of carbon dioxide in the body. Therefore, ideally, air blowing should be done by two people, who can alternate every two to three minutes. If this is not possible, the number of breaths should be reduced every three minutes so that the person performing resuscitation normalizes the level of carbon dioxide in the body.
During artificial respiration, you should check every minute to see if the victim’s heart has stopped. To do this, use two fingers to feel the pulse in the neck in the triangle between the windpipe and the sternocleidomastoid muscle. Two fingers are placed on the lateral surface of the laryngeal cartilage, after which they are allowed to “slide” into the hollow between the sternocleidomastoid muscle and the cartilage. This is where the pulsation of the carotid artery should be felt.
If there is no pulsation in the carotid artery, chest compressions in combination with ID should be started immediately. Doctors warn that if you miss the moment of cardiac arrest and continue to perform artificial ventilation, it will not be possible to save the victim.
Sudden cardiac arrest on the street: what to do before the ambulance arrives?
Resuscitation measures are carried out after establishing a state of clinical death, the main signs of which are: absent breathing and heartbeat, unconsciousness, dilated pupils, lack of response to external stimuli. To reliably determine the severity of the situation, it is necessary to determine the following indicators of the victim:
- check the pulse in the carotid arteries of the neck at the jaw angle - when the pressure drops to less than 60-50 mm Hg. Art. the pulse on the radial artery of the inner surface of the hand is not detected;
- examine the chest, check for spontaneous breathing movements;
- approach the victim’s face to check breathing, determine inhalation and exhalation (air movement assessment);
- pay attention to the color of the skin - cyanosis and severe pallor appear when breathing stops;
- check consciousness - lack of response to stimuli indicates coma.
Cardiopulmonary resuscitation according to the new standards is carried out only in two cases. You should start performing CPR only after determining your pulse and breathing.
If the pulse is clearly detected for 10-15 seconds and atonal breathing is disturbed with episodes of convulsive sighs, artificial respiration is required. To do this, you need to take 10-12 breaths “mouth to mouth” or “mouth to nose” over the course of a minute. While waiting for an ambulance, you need to measure your pulse every minute; if it is absent, CPR is indicated.
If spontaneous breathing and pulse fail, a set of resuscitation measures is indicated strictly according to the algorithm.
Consciousness testing is carried out according to the following principle:
- Address the victim loudly. Ask what happened and how he feels.
If there is no response, use painful stimuli. Pinch the top edge of the trapezius muscle or apply pressure at the base of the nose.- If there is no reaction (speech, twitching, attempts to defend yourself with your hand) - there is no consciousness, you can move on to the next stage.
Breath test:
- Tilt your head back (holding it by the back of your head and chin) and open your mouth. Inspect it for foreign bodies. If they are there, remove them.
- Bend towards your face and for 10 seconds. check your breathing. You should feel it with your cheek and hear and see the movements of your chest. Normally, 2-3 breaths are sufficient.
- If there is no breathing or only 1 breath is felt (which can be considered its absence), we can assume the cessation of a vital function.
In such a case, it is necessary to call an ambulance and begin performing resuscitation measures in case of cardiac and respiratory arrest.
Features of the procedure in children
When performing artificial ventilation for babies under one year of age, the mouth-to-mouth and nose technique is used. If the child is older than one year, the mouth-to-mouth method is used.
Small patients are also placed on their back. For babies under one year old, place a folded blanket under their back or slightly raise their upper body, placing a hand under their back. The head is thrown back.
The person providing assistance takes a shallow breath, seals her lips around the child’s mouth and nose (if the baby is under one year old) or just the mouth, and then blows air into the respiratory tract. The volume of air blown in should be less, the younger the patient. So, in the case of resuscitation of a newborn, it is only 30-40 ml.
If a sufficient volume of air enters the respiratory tract, chest movement occurs. After inhaling, you need to make sure that the chest drops. If you blow too much air into your baby's lungs, this can cause the alveoli of the lung tissue to rupture, causing air to escape into the pleural cavity.
The frequency of insufflations should correspond to the breathing frequency, which tends to decrease with age. Thus, in newborns and children up to four months, the frequency of inhalations and exhalations is forty per minute. From four months to six months this figure is 40-35. In the period from seven months to two years - 35-30. From two to four years it is reduced to twenty-five, in the period from six to twelve years - to twenty. Finally, in a teenager aged 12 to 15 years, the respiratory rate is 20-18 breaths per minute.
Manual methods of artificial respiration
There are also so-called manual methods of artificial respiration. They are based on changing the volume of the chest due to the application of external force. Let's look at the main ones.
Sylvester's method
This method is most widely used. The victim is placed on his back. A cushion should be placed under the lower part of the chest so that the shoulder blades and the back of the head are lower than the costal arches. In the event that artificial respiration is performed using this method by two people, they kneel on either side of the victim so as to be positioned at the level of his chest. Each of them holds the victim’s hand in the middle of the shoulder with one hand, and with the other just above the level of the hand. Next, they begin to rhythmically raise the victim’s arms, stretching them behind his head. As a result, the chest expands, which corresponds to inhalation. After two or three seconds, the victim’s hands are pressed to the chest, while squeezing it. This performs the functions of exhalation.
In this case, the main thing is that the movements of the hands are as rhythmic as possible. Experts recommend that those performing artificial respiration use their own rhythm of inhalation and exhalation as a “metronome”. In total, you should do about sixteen movements per minute.
ID using the Sylvester method can be performed by one person. He needs to kneel behind the victim’s head, grab his arms above the hands and perform the movements described above.
For broken arms and ribs, this method is contraindicated.
Schaeffer method
If the victim's arms are injured, the Schaeffer method can be used to perform artificial respiration. This technique is also often used for the rehabilitation of people injured while on the water. The victim is placed prone, with his head turned to the side. The one who performs artificial respiration kneels, and the victim’s body should be located between his legs. Hands should be placed on the lower part of the chest so that the thumbs lie along the spine and the rest rest on the ribs. When exhaling, you should lean forward, thus compressing the chest, and while inhaling, straighten, stopping the pressure. The elbows are not bent.
Please note that this method is contraindicated for fractured ribs.
Laborde method
The Laborde method is complementary to the Sylvester and Schaeffer methods. The victim's tongue is grabbed and rhythmically stretched, imitating breathing movements. As a rule, this method is used when breathing has just stopped. The resistance of the tongue that appears is evidence that the person’s breathing is being restored.
Kallistov method
This simple and effective method provides excellent ventilation. The victim is placed prone, face down. A towel is placed on the back in the area of the shoulder blades, and its ends are passed forward, threaded under the armpits. The person providing assistance should take the towel by the ends and lift the victim’s torso seven to ten centimeters from the ground. As a result, the chest expands and the ribs rise. This corresponds to inhalation. When the torso is lowered, it simulates exhalation. Instead of a towel, you can use any belt, scarf, etc.
Howard's method
The victim is positioned supine. A cushion is placed under his back. Hands are moved behind the head and extended. The head itself is turned to the side, the tongue is extended and secured. The one who performs artificial respiration sits astride the victim’s thigh area and places his palms on the lower part of the chest. With your fingers spread, you should grab as many ribs as possible. When the chest is compressed, it simulates inhalation; when the pressure is released, it simulates exhalation. You should do twelve to sixteen movements per minute.
Frank Eve's method
This method requires a stretcher. They are installed in the middle on a transverse stand, the height of which should be half the length of the stretcher. The victim is placed prone on the stretcher, the face is turned to the side, and the arms are placed along the body. The person is tied to the stretcher at the level of the buttocks or thighs. When lowering the head end of the stretcher, inhale; when it goes up, exhale. Maximum breathing volume is achieved when the victim's body is tilted at an angle of 50 degrees.
Nielsen method
The victim is placed face down. His arms are bent at the elbows and crossed, after which they are placed palms down under the forehead. The rescuer kneels at the victim’s head. He places his hands on the victim’s shoulder blades and, without bending them at the elbows, presses with his palms. This is how exhalation occurs. To inhale, the rescuer takes the victim’s shoulders at the elbows and straightens, lifting and pulling the victim towards himself.
Stages of cardiopulmonary resuscitation according to new standards
It is extremely important to follow the correct procedure for resuscitation measures. According to the latest medical protocols, to save the victim it is necessary to adhere to the following algorithm:
- A - ensure airway patency for oxygenation, eliminate blockage of the lumen of the pharynx and trachea;
- B - perform breathing using the “mouth to mouth” or “mouth to nose” method;
- C - restore blood circulation using indirect massage.
Technique and procedure for performing indirect cardiac massage and artificial ventilation of the lungs
- It is important to maintain safety; before starting CPR, the person must be placed on a rigid, stable and solid surface or floor.
- After this, tilt your head to the side, open your mouth slightly and make sure that the airway is not blocked. If obstruction is detected, clear the airways using improvised means (handkerchief or napkin).
- For effective artificial respiration, perform the Safar maneuver - tilt your head back, push your jaw forward and upward, and open your mouth in one movement.
- If there are signs of a spinal fracture in the neck area, just move your jaw.
- The resuscitation complex begins with 30 compressions of the sternum, which are performed by one person rhythmically without breaks.
- To do this, you need to place your right hand with your palm resting on the lower part of the sternum in the center, place your left hand on top of your right hand and interlace your fingers.
To perform a heart massage, your arms should be straight, not bent at the elbow joints.- Perform 100-120 compressions per minute with rhythmic compression of the sternum 5-6 cm deep, until the chest is completely expanded after compression.
- After 30 compressions, exhale 2 times into the victim’s mouth or nose for 1 second.
- When breathing using the mouth-to-mouth method, you must close your nostrils with your fingers before exhaling.
- During two exhalations, you should look at the chest: straightening and lifting indicate correct execution.
- If the chest does not rise or fall, it is necessary to check whether the airways are passable, and you may need to repeat Safar.
- During CPR, be sure to check your pulse every 2 minutes. Resuscitate without stopping for up to 30-40 minutes.
Criteria for the effectiveness of activities
With timely assistance, the chance of saving a person increases. To do this, it is important to strictly follow the rules of cardiopulmonary resuscitation. The effective implementation of the CPR complex is indicated by:
- the appearance of a pulse in the carotid arteries - to make sure that the pulse is maintained, cardiac massage can be stopped for 3-5 seconds;
- return of the pupillary reaction to a light stimulus - narrowing indicates an enrichment of oxygenated blood in the brain;
- the appearance of spontaneous breathing with full, steady inhalation and exhalation, without episodes of convulsive inhalations followed by cessation (apnea);
- disappearance of blueness of the skin of the face, lips, hands;
After the heartbeat and breathing are restored, the resuscitation complex is stopped, but the victim must remain in the field of view of the resuscitator until the doctor arrives
Common mistakes in providing assistance
It should be remembered that incorrectly provided first aid often causes more harm than its absence. The following erroneous recommendations and myths are often found on the Internet (the rule of four “NOT”):
- Do not check your breath with a mirror or feather - you waste time looking for it, the humidity outside may interfere with your breathing, and when using a feather, the wind can interfere with the reliability of the result. In such a situation, you will mistakenly consider the dead person to be alive.
Do not check the pupillary reflex - you need to be able to do this correctly and not with the help of a regular flashlight. If a person is alive, too bright light in certain diseases can damage the retina. Finally, there are neurological disorders in which this reflex will not work in a person with preserved vital functions.- You shouldn't do a precordial blow. This requires appropriate practice, moreover, this method has not been proven in terms of effectiveness, and in some cases it can cause even greater harm.
- Do not perform mechanical ventilation without protection (without a film valve) on strangers - there is a high risk of transmission of infection. If the chest does not rise during artificial ventilation, it should be assumed that air is passing into the stomach, or the airways are blocked. In the first case, limit yourself to NMS; in the second, clean your mouth or use the Heimlich maneuver.
Hardware artificial respiration methods
For the first time, hardware methods of artificial respiration began to be used back in the eighteenth century. Even then, the first air ducts and masks appeared. In particular, doctors proposed using fireplace bellows to blow air into the lungs, as well as devices created in their likeness.
The first automatic ID machines appeared at the end of the nineteenth century. At the beginning of the twenties, several types of respirators appeared at once, which created intermittent vacuum and positive pressure either around the entire body, or only around the patient’s chest and abdomen. Gradually, respirators of this type were replaced by air-injection respirators, which had less solid dimensions and did not impede access to the patient’s body, allowing medical procedures to be performed.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
All ID devices existing today are divided into external and internal. External devices create negative pressure either around the patient's entire body or around his chest, thereby inhaling. Exhalation in this case is passive - the chest simply collapses due to its elasticity. It can also be active if the device creates a positive pressure zone.
With the internal method of artificial ventilation, the device is connected through a mask or intubator to the respiratory tract, and inhalation is carried out by creating positive pressure in the device. Devices of this type are divided into portable, intended for work in “field” conditions, and stationary, the purpose of which is long-term artificial respiration. The former are usually manual, while the latter operate automatically, driven by a motor.