Asphyxia of newborns is a condition of newborns in which, due to disruption of the breathing process, oxygen deficiency develops. There are two types of asphyxia: primary, which occurs at the time of birth, and secondary, which develops in the first days after birth.
Causes of newborn asphyxia
Of course, asphyxia will not occur in a newborn baby without any significant reasons. As a rule, the causes of asphyxia are either acute or chronic intrauterine hypoxia. In addition, the cause of asphyxia may be:
- Birth intracranial trauma of a newborn.
- Immunological incompatibility of mother and fetus.
- Blockage of the respiratory tract of a newborn baby - complete or partial, either by amniotic fluid or mucus.
- Fetal malformations that cause difficulty breathing.
In addition to problems with the health of a newborn child, asphyxia can also be caused by such problems as the presence of extragenital diseases of pregnant women. For example, such as:
- Diseases of the cardiovascular system, especially those in the acute stage.
- Severe iron deficiency anemia, especially in the last trimester of pregnancy.
- Diabetes mellitus, especially the insulin-dependent form.
- Late toxicosis is gestosis, accompanied by swelling of the legs and high blood pressure.
Very often, the pathological course of pregnancy also leads to asphyxia of newborns. Pathology of the structure of the umbilical cord, placenta and membranes, premature placental abruption, premature rupture of amniotic fluid and a long anhydrous period are all increased risk factors.
Also, very often, asphyxia of newborns occurs if there are any anomalies of labor, improper insertion of the fetal head, a pathologically narrow pelvis of the woman in labor, etc.
The causes of secondary asphyxia can be such health problems in the child as congenital pneumonia, cerebrovascular accidents, vomit entering the respiratory tract, and some types of disruption of the central system of the newborn child.
What happens during asphyxia?
What happens in the body of a newborn baby at the time of asphyxia? Regardless of what exactly caused the asphyxia, the child begins to immediately change metabolic processes, blood microcirculation and hemodynamics. How strongly these changes will be expressed depends on the duration of asphyxia and the degree of its intensity.
During acute hypoxia, the child's total blood volume increases significantly. This occurs due to the fact that the volume of red blood cells circulating in the blood increases. In the event that acute asphyxia develops against the background of chronic fetal hypoxia preceding it, hypovolemia develops. Hypovolemia is a change in blood consistency: it thickens, its viscosity increases, and red blood cells and platelets acquire increased aggregation ability.
In the internal vital organs of a newborn child - in the liver, in the kidneys and adrenal glands, in the heart and brain - swelling and hemorrhages that occur as a result of tissue hypoxia can be detected. Due to a decrease in peripheral and central hemodynamics, the number of heartbeats decreases and blood pressure drops. Due to disruption of the normal course of the metabolic process, the urinary function of the kidneys is impaired.
Diagnostics
When making a diagnosis: “Asphyxia of a newborn,” data from the obstetric history, how the birth proceeded, the child’s Apgar assessment at the first and fifth minutes, and clinical and laboratory tests are taken into account.
Determination of laboratory parameters:
- pH level, pO2, pCO2 (test of blood obtained from the umbilical vein);
- definition of base deficiency;
- level of urea and creatinine, diuresis per minute and per day (function of the urinary system);
- level of electrolytes, acid-base status, blood glucose;
- level of ALT, AST, bilirubin and blood clotting factors (liver function).
Additional methods:
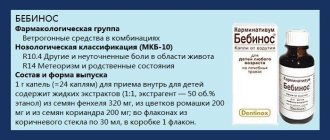
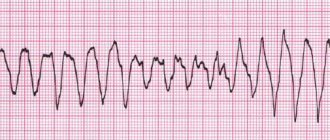
- assessment of the functioning of the cardiovascular system (ECG, blood pressure control, pulse, chest x-ray);
- assessment of neurological status and brain (neurosonography, encephalography, CT and NMR).
Signs of newborn asphyxia
The most important sign of asphyxia in a newborn child is a violation of the respiratory process, which leads to a change in the rhythm of cardiac activity, as well as a pathological change in the functioning of the nervous system: impaired neuromuscular conduction and extinction of reflexes. In the very first seconds after birth, neonatologists carefully examine the child and assess his condition. The child’s condition is assessed using a special Apgar scale:
- Mild form of asphyxia
In the event that asphyxia is not pronounced, and the child’s body has not suffered much, the assessment of the child’s condition on the Apgar scale will be 6 – 7 points. A child born with a mild form of asphyxia takes his first breath within the first minute after birth. However, despite this, the baby’s breathing is weakened, there is a decrease in muscle tone and cyanosis (blue discoloration) of the nasolabial triangle.
- Moderate severity of asphyxia
In the same case, if the baby is diagnosed with an average degree of hypoxia, the score will be 4–5 points. If a child was born with moderate asphyxia, he will also take his first breath within a minute after birth, but breathing is greatly weakened and may be irregular, and the baby’s cry is very weakened.
The baby may also experience tachycardia, bradycardia, decreased muscle tone and all reflexes. The skin of the hands and feet, as well as the face, has a pronounced bluish tint. The umbilical cord of such a baby is characterized by intense pulsation.
- Severe form of hypoxia
With a pronounced form of asphyxia, doctors assess the child’s condition at 1 – 3 points.
In severe asphyxia, breathing is irregular (individual breaths) or absent, the child does not scream, sometimes groans, the heartbeat is slow, in some cases replaced by single irregular heart contractions, muscle hypotonia or atony is observed, there are no reflexes, the skin is pale as a result of spasm of peripheral vessels, the umbilical cord is not pulsates; Adrenal insufficiency often develops.
- Clinical death
If the overall Apgar score is 0, the child is in a state of clinical death. In this case, in order to save the child’s life, resuscitators immediately begin a set of resuscitation measures.
Consequences and complications
The pathology is quite dangerous and is one of the most common causes of child mortality. How favorable the prognosis will be depends on the severity of the baby’s condition and the Apgar indicator. If the score increases, the prognosis is considered favorableSource: Modern methods of treating neonatal asphyxia. Cherednikova E.N., Sherstnev D.G. Bulletin of Medical Internet Conferences, 2021. p.824.
However, with severe pathology, serious complications develop during the first year of life. Early consequences that may appear in the first few days after resuscitation include :
- respiratory arrest (the most common and dangerous complication);
- pulse failure;
- convulsions;
- cerebral edema;
- disruption of the urinary and digestive systems.
Later disorders include the following diagnoses:
- syndrome of increased excitability (hyperexcitability);
- increased intracerebral pressure (hypertension syndrome);
- lesions of the central nervous system (perinatal encephalopathy);
- disruptions in the functioning of the endocrine and vegetative-vascular systems (hypothalamic disorders).
With timely and competent medical intervention, as well as a high-quality recovery period, asphyxia of newborns may not have dangerous consequences in the future. Mild forms of asphyxia have almost no effect on the child; after the illness, his further development will proceed in the same way as in other babies.
Treatment of acute asphyxia of newborns
Strictly speaking, all children, without exception, born in a state of asphyxia require immediate intensive care. How effective all medical procedures will be depends on how quickly after birth they began. All intensive care activities begin immediately after the birth of the child, right in the delivery room.
During resuscitation measures, the child’s condition is continuously monitored by all the basic parameters of his body’s vital functions:
- Heart rate.
- Hematocrit
- Respiratory frequency and depth.
Based on these indications, doctors have the opportunity to monitor the effectiveness of their actions and, if necessary, adjust them.
Immediately after the fetal head is born, the doctor inserts a soft probe into the newborn’s mouth and nose and, using electric suction, removes all the contents of the upper respiratory tract: residual amniotic fluid, mucus. After this, the child’s umbilical cord is cut, and the baby is placed on a special resuscitation table, under the rays of a special lamp. After this, repeated aspiration of the contents of the nasopharynx, as well as the contents of the stomach, is performed.
After the child’s cardiac and respiratory activity is restored and his condition is stabilized, the baby will be transferred to the intensive care unit. All further medical measures will be aimed at preventing or eliminating existing cerebral edema, normalizing metabolic processes, restoring kidney function and hemodynamics.
Rules for caring for a child who has suffered asphyxia
In order for the child to recover from the effects of asphyxia as quickly as possible, it is very important to provide him with proper medical care. The child should be completely at rest, and his head should be in an elevated position. Intensive oxygen therapy for all babies without exception who have suffered asphyxia is very important.
Children born with a mild form of asphyxia are placed in a special oxygen tent. This tent is a kind of dome, inside of which there is a high oxygen content. The child spends there from several hours to several days, depending on his state of health.
In the same case, if the child has suffered moderate or severe asphyxia, he should be placed in an incubator. Oxygen is supplied to the incubator; its concentration inside should be approximately 40%. In the same case, if for some reason the maternity hospital does not have the necessary equipment, oxygen can be supplied through a special nasal cannula or through a breathing mask.
Very often, a newborn baby needs repeated suctioning of the contents, usually mucus, from the baby’s upper respiratory tract. Careful monitoring of indicators such as bowel function, diuresis, and body temperature is also necessary.
The first feeding of a child who has suffered mild to moderate asphyxia is performed approximately 16 hours after birth. Those children who were born in a state of severe asphyxia are fed for the first time after 24 hours, using a special tube. But the question is about that. When a baby can begin to be put to the breast is decided individually in each case, depending on the child’s condition.
Prevention of suffocation in a newborn
- After each feeding, the baby should be given the opportunity to burp the air swallowed with food. To do this, you need to hold it vertically for some time and under no circumstances put it down immediately after feeding. Some babies (especially premature or weak ones) may burp repeatedly while in the crib. To prevent inhalation of contents, always turn the infant's head to the side. If regurgitation is frequent and profuse, then this is a reason to consult a doctor.
- When choosing children's bedding and clothing, preference should be given to products without all kinds of ties, ribbons, etc. Instead of a baby blanket, you can use a special sleeping envelope; do not use too large “adult” blankets. You can use special mesh blankets for babies.
- You should not leave older children alone near the newborn for a long time, hoping for their maturity and prudence, and also put the baby to sleep in the same bed with them. And sleeping together in the same bed with parents is not safe from the point of view of possible asphyxia.
- Co-sleeping can also be a risk factor for baby suffocation. Although many new mothers bring their babies to bed with them, it is still optimal to sleep in the parents' bedroom, but not in the parents' crib. Place the baby crib next to yours and lower the side rail. On the one hand, this will ensure the safety of the baby, on the other hand, you will be in close proximity to your child and you will not have to jump up several times at night. It will be convenient for you to feed the baby at night, and then, without getting up, transfer him to the crib.
- To prevent respiratory arrest, it is preferable to place the child alternately on one side or the other, since there are some disadvantages in the positions on the back and on the stomach.
Advertising
Scientists have identified a certain relationship between a child sleeping on his stomach and an increase in the incidence of sudden infant death syndrome (SIDS). This is the name for the sudden death of a child in the first year of life (especially the first to fourth month) for unknown reasons, against the background of complete health, often at night and in the early morning hours. Neither a detailed study of the baby’s medical history nor the results of a pathological examination help explain the reasons for this phenomenon. So far, only the factors influencing sudden death have been clarified, by which it is possible to identify children at risk and carry out preventive measures for them. However, in the prone position, gases are released more easily from the baby’s swollen belly, the back muscles are strengthened, and the correct position of the hip joints is formed. And if you don’t risk putting your baby to sleep on his stomach at night, then you can easily do this during the day when the baby is under your control. But the supine position also has its disadvantages. In this position, children suffering from regurgitation and vomiting may choke on vomit. And with an underdeveloped frenulum, the tongue can also easily sink.
In conclusion, we note that you should always think about the safety of the baby. He is very defenseless and can only help himself by calling on those around him to cry.
After discharge from the maternity hospital
After the baby is discharged home, he should be under medical supervision of specialists such as a pediatrician and a neurologist. This is necessary in order to prevent possible complications from the central nervous system.
The subsequent prognosis depends on several factors, in particular on the severity of asphyxia, the timeliness of the start of treatment measures and their adequacy. In the event that a child was born with primary asphyxia, the prognosis depends on the secondary assessment of the condition on the Apgar scale (performed 5 minutes after birth). If the second score is higher than the first, then the prognosis for the child’s life is quite favorable.
If a child is born in a state of asphyxia, such complications may occur during the first years of life. Asphyxia of newborns, consequences:
- Hyper and hypoexcitability.
- Hydrocephalic syndrome.
- Convulsive syndrome.
- Diencephalic disorders.
They occur especially often if there has been severe asphyxia of newborns. It is in order to reduce the risk of developing such complications and start treatment in a timely manner that clinical observation by specialists of the relevant profiles is necessary.
General information about the disease
Asphyxia is diagnosed in 4-6% of children. Moreover, the percentage varies depending on the degree of prematurity of the fetus. In babies born before 36 weeks, the incidence of pathology reaches 9%, and in children born after 37 weeks it decreases to 1-2%.
Scientific definitions of newborn asphyxia boil down to the fact that the child cannot breathe independently or makes superficial convulsive breathing movements that do not allow the body to receive sufficient oxygen. The authors consider infant asphyxia as suffocation, in which other signs that the fetus is alive remain: there is a heartbeat, the umbilical cord is pulsating, the muscles are weak but contracting.
The reasons for the development of newborn asphyxia include a complex of risk factors that disrupt the blood circulation and respiratory functions of the fetus in the womb and during birth. The most common reasons include:
- conflict of Rh blood between mother and child;
- abnormal fetal development;
- pathologies of the nervous system in a baby;
- circulatory disorders, heart disease in the baby;
- intracranial injury that the baby received during the birth process;
- infections affecting the fetus in the womb (chlamydia, herpes, rubella, etc.);
- extragenital pathologies of the mother (thyrotoxicosis, anemia, diabetes mellitus);
- infectious diseases in the second and third trimesters;
- complicated childbirth;
- premature or post-term pregnancy;
- bad habits of the mother (effects of alcohol, nicotine, drugs on the body);
- malnutrition during pregnancySource: Asphyxia of newborns. Zhetpisova L.B. West Kazakhstan Medical Journal, 2011.
The most common cause of asphyxia is intrauterine hypoxia, that is, the baby lacks oxygen in the womb.
Whatever the causes of the pathological condition, it causes the same processes in the child:
- disrupts metabolism and blood circulation;
- thickens and increases blood viscosity;
- damage is caused to the brain, liver, heart, adrenal glands;
- organs swell, bleeding occurs;
- disruptions in the functioning of the central nervous system occur.
The longer the body feels a lack of oxygen, the more serious the degree of damage to tissues, organs and systems becomes.