Classification of the disease
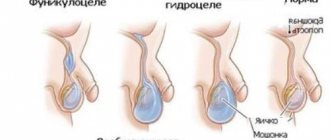
Based on the nature of localization, there are two types of hydrocele: isolated and communicating.
The isolated form of the pathology is characterized by the accumulation of fluid directly in the scrotum. Communicating hydrocele of the testicles is characterized by the free transfusion of fluid from the abdominal cavity into the child’s scrotum, where it accumulates in a large volume. In some cases, when the processus vaginalis closes, the communicating hydrocele becomes isolated. There are also congenital and acquired hydrocele of the testicles. Congenital pathology is a physiological feature and most often resolves during the first 2 years of life without any consequences. The acquired form of the disease develops after injury, infection and requires medical attention.
Another classification involves dividing hydrocele into a primary form, when the pathology is caused by the anatomical features of the baby, and a secondary form, in which the disease develops due to external factors.
Complications of dropsy
Infertility. Impaired spermatogenesis - one of the most common causes of infertility can be a consequence of impaired blood microcirculation and temperature due to the pressure of excess fluid in the testicles.
Hernias (inguinal or inguinoscrotal). With a communicating form of dropsy, the unclosed lumen of the vaginal process of the peritoneum can gradually increase and turn into a hernia.
Pain syndrome. Pain, which can become a serious psychological problem for a child, is uncommon with dropsy. The exception is acute hydrocele with a significant increase in testicular volume.
Symptoms of hydrocele in boys
Pathology, as a rule, is discovered completely by accident by a pediatrician during preventive examinations or by parents during daily hygiene procedures. Visually, you can notice an enlargement of the scrotum on one or both sides. In an isolated form of the disease, the volume of tissue increases gradually; in the case of a communicating pathology, the size may vary depending on the position of the body, motor activity and the location of fluid accumulation. Hydrocele of the testicles itself does not cause pain, discomfort, itching or other unpleasant symptoms in the child.
Babies are often capricious, toss and turn, and restless, and older children may complain of discomfort when walking, running, a feeling of heaviness and fullness in the groin. In some cases, hydrocele is accompanied by the formation of a unilateral or bilateral inguinal hernia.
When is surgery needed and how is it performed?
When acute dropsy appears against the background of another disease or injury, surgery is performed. In addition, surgical intervention is indicated when puncture has no effect and fluid continues to accumulate. Four different operations are performed to treat children - Lord's, Ross's, Winkelmann's and Bergmann's.
Bergman's operation
Indicated for large-scale accumulation of fluid in the scrotum. Complete excision of the vaginal membrane, removal of lymph with a syringe, and suturing of the scrotal membranes are expected. In early childhood, this operation is not performed because the testicles need to be fully formed.
Most often, for hydrocele in children, Ross and Winkelmann operations are performed.
Operation Ross
A small incision is made in the groin and the canal between the scrotum and the abdominal cavity is sutured through it. The Ross operation is indicated for congenital communicating hydrocele. The procedure lasts about 30 minutes and general anesthesia is used. After surgery for hydrocele, children are advised to limit physical activity and not to wet the surgical wound. After 1-2 weeks, the stitches are removed.
Winkelmann operation
This operation is performed if the disease is caused by the fact that the lymphatic system produces excess lymph, which overflows the testicular membrane. An incision is made on the front of the scrotum. The testicle is removed, the lymph is removed through the dissected membrane. In this case, the shell is turned inside out and stitched in this position. As a result, excess lymph is no longer formed - it is absorbed into the connective tissue.
Reasons for the development of pathology
The need to treat testicular hydrocele directly depends on the cause of the disease in the child.
In general, factors contributing to the development of hydrocele can be divided into two large groups depending on the form of the pathology. Reasons that can provoke congenital hydrocele include:
- various infectious diseases suffered by the mother during pregnancy;
- birth injuries;
- birth of a baby prematurely;
- developmental anomalies;
- congenital defects of the abdominal wall;
- malformations of the genitourinary sphere and pelvic organs.
The main reason for the formation of testicular hydrocele in a child at birth remains cleft processus vaginalis, which allows peritoneal fluid to circulate freely between the scrotum and peritoneum.
Factors that can provoke an acquired form of hydrocele are:
- acute infectious and inflammatory diseases of a general and local nature;
- chronic pathologies;
- complications after surgery for the pelvic organs;
- injuries and bruises;
- growth of tumors;
- testicular torsion.
The development of testicular hydrocele in a newborn child is promoted by hysterical crying, screaming, colic, and frequent constipation. In older children and schoolchildren, the starting mechanism can be physical labor, active sports with minimal rest, lifting heavy objects, prolonged coughing, tension in the abdominal wall during bowel movements.
Hydrocele of the testicle in a child and newborn
Hydrocele of the testicle in newborns and young children is a fairly common occurrence.
Communicating hydrocele of the testicle in a child and newborn
In newborns and young children, the main cause of testicular hydrocele is an open processus vaginalis . What the processus vaginalis is, how it is formed, and what significance it has in the development of the disease, you will find in the article “Causes of hydrocele.”
Here we will only briefly repeat that the processus vaginalis is formed during intrauterine development, when the testicle descends from the abdomen into the scrotum. The process communicates with the abdominal cavity . By birth, it should be overgrown and only the vaginal membrane remains around the testicle. Often, by the time of birth, the appendix does not close and the connection with the abdominal cavity remains.
Drawing. Hydrocele of the testicle of communicating type.
An interesting fact is that even after birth, the processus vaginalis can close on its own. The older the child becomes, the less likely it is to be saved. In 80%-95% of all newborns the processus vaginalis is not closed ; by 2 years this figure is 25%-40%.
The incidence of hydrocele in newborns is 1%-2%. In 10% of cases, testicular hydrocele can be bilateral. In premature newborns weighing less than 1500 grams, the risk of the disease is 20 times higher than in full-term infants.
As you can see, not all newborns and children who have an open appendix develop testicular hydrocele. Why this happens is still not clear enough.
Isolated hydrocele of the testicle in a child and newborn
In children over 12 years of age, hydrocele is often presented as an isolated type. You can read about the main reasons leading to the formation of this type of hydrocele in the section “Causes of hydrocele”.
Drawing. Isolated hydrocele of the testicle in a child and newborn.
Please note that at any age, from newborns to adolescence, children can experience both communicating hydrocele and isolated hydrocele.
Symptoms of hydrocele in newborns and children
The main symptom of hydrocele in a newborn baby is an increase in the volume of the scrotum . Of course, the first people to notice this are parents. Pain is an uncharacteristic symptom of testicular hydrocele. Hydrocele does not cause discomfort or anxiety in the child. Pain and anxiety may appear when the hydrocele increases in size too quickly or when a section of the intestine enters the processus vaginalis, i.e. an inguinal hernia forms .
Drawing. Hydrocele of the testicle in a child.
Parents may also note another characteristic manifestation of a communicating hydrocele in a child and newborn - the size of the scrotum changes throughout the day . The size of the dropsy increases when the child is active, screaming or crying, sneezing, or other physical stress. In the supine position and at rest, the size of the scrotum decreases again.
Parents should always be on guard. If the child suddenly becomes restless, screams and refuses to eat, the scrotum feels more tense to the touch, vomiting appears or the temperature rises, you should immediately seek help from a doctor. These symptoms may be signs not only of the formation of an inguinal hernia, but also of its strangulation, which can be fraught with serious complications. You can read about this in the article “What is the danger of hydrocele and its complications.”
Is it necessary to see a doctor?
If parents notice an increase in the size of the scrotum in a newborn or child, even though it does not affect his general condition, it is worth consulting a doctor to rule out another more serious pathology.
Medical examination
First, the doctor examines the child while he is lying on his back. During the examination of the newborn, parents help the doctor by lifting the leg up and fixing the arms.
To the touch, the hydrocele is not tense, smooth and painless. The scrotum is increased in volume, but the color and temperature of the skin are not changed. During compression, i.e. by gently squeezing the scrotum, the volume of testicular hydrocele decreases, because fluid from the hydrocele moves freely through the open channel into the abdominal cavity.
Diaphanoscopy and ultrasound examination may also be performed, and additional laboratory tests may be prescribed, which you can read about in more detail in the section “Examination for testicular hydrocele.”
Treatment of hydrocele in a child and newborn
If a child has idiopathic isolated hydrocele, treatment is not required. It tends to gradually decrease in size and resolves on its own within 12-24 months. If this does not happen, you should consult a doctor to decide on surgical intervention.
A communicating hydrocele in the first two years of a child’s life should also not be operated on ; there is a high probability of spontaneous closure of the processus vaginalis. If hydrocele persists after age two, surgery should also be considered.
The development of complications of the disease, namely hematocele, strangulated inguinal hernia, suppuration of hydrocele, etc., requires immediate medical attention .
More detailed information about surgical intervention can be found in the article “Surgery for hydrocele in newborns and children.”
Back to articles
Diagnostic methods
The examination for suspected hydrocele begins with a thorough examination. The doctor assesses the condition of the groin area, carefully checks the soft tissues and external genitalia, first in a vertical, then in a horizontal position. When palpating the scrotum, the doctor may feel tightness and tension, but the testicle cannot be felt. Based on the results of an in-person examination, one can draw a conclusion about the form and extent of the pathology.
Additionally, to clarify the nature of the hydrocele, the following are used:
- ultrasound examination of the groin area, which allows you to determine the presence and amount of fluid, identify the communication between the scrotum and the peritoneum, possible other diseases, and assess the general condition of the internal structures;
- diaphanoscopy or transillumination, which is the transillumination of the soft tissues of the scrotum with a narrow beam of light, which helps to clarify the nature and color of the liquid;
- scrotal biopsy, which is necessary in doubtful cases when malignant or other neoplasms are suspected.
A standard set of laboratory tests of blood and urine is also carried out. In rare cases, with extensive lesions and concomitant diseases, computed tomography or magnetic resonance imaging may be required.
Diagnostics
The scrotum is examined in a standing and lying position. This diagnostic technique is used to determine the form of hydrocele in boys (communicating or not communicating with the abdominal cavity). If the size of the hydrocele decreases in the supine position, you should think about communicating the hydrocele with the abdominal cavity. Also in favor of communicating hydrocele of the testicle is an increase in the size of the hydrocele during coughing, i.e., with an increase in intra-abdominal pressure. By palpation, hydrocele in boys is determined as a pear-shaped compaction, with its upper part facing towards the inguinal canal. Using an ultrasound of the scrotum and inguinal canals, the diagnosis of hydrocele in boys is confirmed and a more serious pathology (testicular cancer, inflammation or torsion of the testicle or its epididymis) is excluded. In addition, ultrasound of the scrotum is a highly sensitive method in determining the type of hydrocele in boys (communicating or non-communicating). In addition to the main study, it is advisable to conduct an ultrasound scan of the scrotal vessels.
Treatment of hydrocele
Treatment methods for hydrocele include therapeutic and surgical methods.
The choice of tactics depends on a number of factors: the boy’s age, general health, nature and form of pathology. In case of congenital disease, observation is usually indicated; if by 1.5–2 years the pathology does not go away on its own, surgical removal is resorted to.
Only surgical intervention can completely eliminate testicular hydrocele in infants and older children. There are several options for performing the operation:
- according to Bergman - this tactic is indicated for extensive accumulations of fluid in the scrotum area, but only if the boys have already formed testicles;
- according to Ross - an operation during which the duct between the peritoneum and the scrotum is sutured through a small incision in the groin area, prescribed for congenital communicating dropsy;
- according to Winkelmann - a similar technique is used in cases where the cause of the hydrocele is a violation of the outflow of lymph; after eliminating the pathology, excess fluid no longer accumulates.
Only the doctor decides how exactly to treat hydrocele, based on the information obtained during the examination of the child.
Hydrocele is quite easy to treat: in 98% of cases, the pathology completely disappears after surgery without any consequences. Re-development of testicular hydrocele is possible, but is rare, especially if treatment was carried out correctly and in a timely manner.
Price and cost of surgery for hydrocele in children
| Service | price, rub. |
| Surgical treatment of hydrocele of 1st category of complexity | 37000 |
| Surgical treatment of hydrocele of 2nd category of complexity | 49000 |
| Surgical treatment of hydrocele of 3rd category of complexity | 63000 |
The cost of the operation includes (no additional payment for services is necessary!):
- inpatient accommodation 1 day double room with all amenities
- preoperative tests
- disposable suture material Vicryl, PDS
- application of intradermal cosmetic suture
- disposable surgical consumables
- surgical instruments Ceatec GmbH Germany
- microsurgical instruments and equipment
- constant telephone communication with the attending physician
- examination any day in the clinic within 14 days after surgery
The cost of the operation does not include: anesthesia, additional diagnostics and treatment of concomitant diseases and their complications.
Anesthesiological support: anesthesiological apparatus Drager Fabius Plus (Germany), combined general anesthesia (inhalation anesthesia, caudal/local anesthesia).
** This is not a public offer agreement. Check the cost of services on the day of your request.
Don't waste your precious time - call!
Our specialists will be happy to answer all your questions
+7
Our advantages
Experienced surgeons
Individual approach
Without pain and fear
Comfortable conditions
Prevention
At the stage of planning and maintaining pregnancy, the expectant mother needs to carefully monitor her health, promptly eliminating infectious and inflammatory diseases. To prevent a newborn child from developing hydrocele of one or both testicles, it is necessary:
- regularly examine the baby’s genitals and properly care for them;
- avoid hypothermia and overheating of the scrotum;
- teach children the rules of personal hygiene to avoid infection;
- prevent the development of obesity in children;
- stimulate adequate physical activity.
In the case of a congenital form of hydrocele, the child should be under regular supervision of a urologist or surgeon until complete recovery or surgery.
Hydrocele of the testicle is one of the diseases that can cause male infertility. Do not ignore a visit to a urologist-andrologist; at the slightest sign of a problem, make an appointment with an experienced specialist at the SM-Doctor clinic.
Causes of non-fusion of the peritoneal process.
Many theories explain non-fusion of the processus vaginalis of the peritoneum. Thus, in the open vaginal process of the peritoneum, smooth muscle fibers were found, which are not found in the normal peritoneum. Smooth muscles can prevent fusion of the peritoneal process.
According to our data, there is a higher incidence of reported hydrocele in children born after a pathological pregnancy with threatened miscarriage, as well as in premature children.
Another reason lies in the increase in intra-abdominal pressure, which is observed during resuscitation measures, with frequent restlessness of the child or during physical exercise.
Complications of operations.
The overall risk of complications ranges from 2 to 8%.
Relapses of dropsy occur with a frequency of 0.5 to 6%. In adolescence, relapses of dropsy are more common.
The risk of infertility after such operations is due to surgical trauma and averages about 2-5% and mainly depends on the technique of performing the intervention.
Infertility is not always a manifestation of damage to the vas deferens. In 5-8% of patients, there are rudiments of the rudiments of the female genital organs, which indicate the presence of more or less pronounced defects of the reproductive system that arise in utero or are genetically predetermined.
One of the complications is high fixation of the testicle, when the testicle is pulled up to the inguinal canal and is subsequently fixed there with scar adhesions.
Testicular atrophy can be observed due to impaired blood circulation in the testicle, which occurs during mobilization of the peritoneal process from the elements of the spermatic cord.
Unpleasant or painful sensations in the area of the wound or scrotum on the side of the operation - hyperesthesia associated with pinching in the scar or damage to nerve endings. These phenomena usually disappear 6-12 months after surgery.
Prevention of complications.
The development of complications can be prevented by a high level of surgical technology and timely determination of indications for surgical treatment.
Complications of varicocele
As a rule, physiological dropsy disappears on its own during the first year of life. If surgical intervention was performed according to indications, then most often the disease goes away and does not occur again.
Chronic testicular hydrocele, which is a consequence of neglected treatment, poses a significant danger. It can cause spermatogenesis disorders and complete infertility in older age. The disease can also provoke a sensitivity disorder in the testicle and, as a result, its atrophy.
Treatment of hydrocele (hydrocele) and lymphocele without surgery. Duration of observation.
Hydrocele in children under 1 year of age requires observation by a pediatric urologist-andrologist. If fluid accumulates and tension appears in the membranes of the testicle, punctures are performed to remove hydrocele. Sometimes repeated punctures are required.
Communicating hydrops with a narrow peritoneal process is usually observed up to 2 years.
Observation is also required for traumatic dropsy, which occurs as a result of a bruise without compromising the integrity of the testicle. As a rule, 3 months are enough to assess the dynamics of the process and, if there is no improvement, prescribe surgical treatment. The same applies to hydrocele formed after inflammation.
The most difficult is the management of patients with lymphocele that forms after surgical treatment of an inguinal hernia and varicocele. In this case, prematurely performed surgery has little chance of success. For 6-12 months, it is necessary to monitor the condition of the testicle according to ultrasound and duplex examination of the scrotal organs in order to assess the dynamics of the process and the effectiveness of the therapy.