ANTIPLAGANT DRUGS (Part 1)
Preferanskaya Nina Germanovna Associate Professor, Department of Pharmacology, Educational Department, Institute of Pharmacy and Translational Medicine, Multidisciplinary Center for Clinical and Medical Research, International School “Medicine of the Future”, First Moscow State Medical University. THEM. Sechenov (Sechenov University), Ph.D.
Platelets [from Greek. θρóμβος - clot; kukτος - cell] - these are nuclear-free red plates of blood, disc-shaped or spherical in shape, small in size, the diameter of which is ~1.5–4 µm. Normally, the number of platelets in an adult reaches 180–320 thousand per 1 ml of blood. Platelets circulate in the blood for 6 to 12 days, then are captured and used by endothelial cells (15–25%), the rest are destroyed by tissue macrophages. The main function of platelets is hemostasis, eliminating endothelial damage. The endothelium is the inner layer of the wall of blood vessels and capillaries; it is a continuous membrane of flattened cells of mesenchymal origin. The endothelium ensures metabolic processes between blood and tissues, influences the functional activity of platelets, secretes substances released into the bloodstream: prostacyclin (PGI2) and endothelial vascular relaxation factor (nitric oxide - NO), prevents platelet aggregation, reduces blood clotting, promotes thrombus lysis . All this ensures the antithrombogenic properties of intact vascular endothelium.
When vascular damage is caused by various factors, including mechanical trauma, infections, atherosclerotic changes in the vascular wall, vasospastic vascular diseases, etc., the antithrombogenic properties of the endothelium are reduced and conditions are created for the formation of a blood clot and stopping bleeding. Under these conditions, processes leading to thrombus formation proceed quickly and uncontrollably. Platelets and plasma clotting factors accumulate at the site of injury. At the same time, a functional narrowing of the lumen of damaged vessels occurs due to the secreted serotonin and thromboxane. The synthesis of PGI2 and NO is disrupted, which facilitates platelet contact with the damaged endothelial surface. Platelets begin to interact with the subendothelial layer and bind to its proteins - von Willebrand factor and collagen. The process is initiated with the participation of specific glycoproteins localized in the platelet membrane. Von Willebrand factor binds to glycoprotein Ib, and collagen binds to glycoprotein Ia of the platelet membrane. During the process of platelet adhesion, collagen and thrombin act on them (the latter is formed locally, in small quantities, already at the initial stage of thrombus formation), which causes activation of platelets and changes their condition. Platelets change their shape, they become round with many spiny processes (pseudopodia) and in this form cover the damaged surface of the vessel. When activated, various biologically active substances (BAS) are released from platelets - serotonin, adenosine diphosphate (ADP), thromboxane , etc. In non-activated platelets, BAS are located in dense granules, which are their storage. The release of substances from platelet granules occurs as a result of an increase in the intracellular concentration of Ca2+, when collagen, thrombin and other aggregation inducers act on platelets. Thrombin, reacting with specific receptors in the platelet membrane, initiates irreversible platelet aggregation, causes phosphorylation of intracellular proteins and the release of Ca2+ ions. ADP released into the bloodstream stimulates specific purinergic receptors (localized in the platelet membrane) and causes inhibition of adenylate cyclase, a decrease in the level of cAMP, which also increases the level of Ca2+ in the cytoplasm of platelets.
When platelets are activated, the activity of the platelet membrane enzyme, phospholipase A2, which is involved in the formation of arachidonic acid from membrane phospholipids, increases. From arachidonic acid, under the influence of cyclooxygenase (COX), cyclic endoperoxides are first synthesized in platelets, and from them, with the participation of thromboxane synthetase, thromboxane A2 (PGA2) is formed. Thromboxane is an active stimulator of platelet aggregation and a powerful vasoconstrictor. Once released into the bloodstream, thromboxane A2 stimulates thromboxane receptors in the platelet membrane. As a result, phospholipase C is activated and the formation of inositol-1,4,5-triphosphate increases, which contribute to the release of Ca2+ from the calcium store of platelets. The concentration of Ca2+ in the cytoplasm of platelets and in vascular smooth muscle cells increases, which contributes to increased vascular contraction.
Cytoplasmic Ca2+ causes a change in the conformation of glycoproteins IIb/IIIa in the platelet membrane, as a result of which they acquire the ability to bind fibrinogen. One fibrinogen molecule has two binding sites for glycoproteins IIb/IIIa and thus can unite two platelets. The joining of many platelets by fibrinogen bridges leads to the formation of platelet conglomerates of various sizes and densities. This combination of platelets is called platelet aggregation.
Prostacyclin has the opposite effect on platelet aggregation . Prostacyclin is formed from cyclic endoperoxides, but unlike thromboxane, prostacyclin synthetase is required for its conversion. Prostacyclin is synthesized by endothelial cells and released into the bloodstream, where it stimulates prostacyclin receptors in the platelet membrane and the associated adenylate cyclase. As a result, the level of cAMP in platelets increases and the concentration of cytoplasmic Ca2+ decreases. This prevents the conformation of glycoproteins IIb/IIIa from changing, and they lose their ability to bind fibrinogen. Thus, prostacyclin prevents platelet aggregation. Under the influence of PGI2, the Ca2+ concentration decreases, vascular smooth muscle fibers relax, and vasodilation occurs. Prostacyclin causes platelet disaggregation and promotes fibrinolysis.
Platelet aggregation and blood clotting are interrelated. The predominance of one or another process in the mechanism of thrombus formation depends on the caliber of the vessel and the speed of blood flow. Platelet aggregation is of great importance for the formation of blood clots in arteries where blood flow velocity is high. In venous vessels, where the blood flow velocity is low, the process of blood clotting predominates.
The main focus of the action of antiplatelet agents used in clinical practice is mainly related to the elimination of the action of PGA2, ADP, as well as the blockade of glycoproteins IIb/IIIa of platelet membranes. In clinical practice, substances are also used that act in a different way, for example, they increase the concentration of cAMP in platelets and, therefore, reduce the concentration of Ca2+ in them.
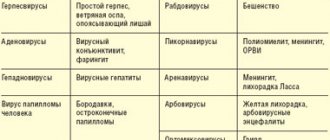
The following groups of antiplatelet drugs are distinguished:
I. Agents that inhibit the enzyme cyclooxygenase (COX) and reduce the synthesis of thromboxane (PGA2):
- a) salicylic acid derivative - acetylsalicylic acid ;
- b) combination drugs with acetylsalicylic acid .
II. Agents that irreversibly block purinergic receptors and prevent the action of ADP on platelets:
- a) thienopyridine derivative - ticlopidine ; heterocyclic phenylacetate derivative - clopidogrel ;
- b) fluorinated derivatives - ticagrelor, prasugrel .
III. Agents that inhibit phosphodiesterase and increase the level of cAMP in platelets - dipyridamole, pentoxifylline .
IV. Prostacyclin receptor agonists - epoprostenol, iloprost .
V. Agents blocking glycoproteins IIb/IIIa of platelet membranes:
- a) monoclonal antibodies - abciximab ;
- b) synthetic blockers of glycoproteins IIb/IIIa - eptifibatide .
DRUGS THAT REDUCE THROMBOXANE A2 SYNTHESIS
Acetylsalicylic acid (Aspirin Cardio, CardiASK, Thrombo ACC) is an ester of salicylic acid. Belongs to the group of non-steroidal anti-inflammatory drugs, has analgesic, antipyretic and anti-inflammatory effects. Currently widely used as an antiplatelet agent. The antiplatelet effect of acetylsalicylic acid is associated with its inhibitory effect on the synthesis of thromboxane (PGA2) in platelets. Acetylsalicylic acid is the only selective irreversible inhibitor of type 1 cyclooxygenase (COX-1) in platelets (causes irreversible acetylation of the enzyme) and thus disrupts the formation of cyclic endoperoxides, precursors of thromboxane A2, from arachidonic acid, thereby reducing not only the synthesis of PGA2 in platelets, but also synthesis of prostacyclin in vascular endothelial cells, which is undesirable.
Platelets (unlike endothelial cells) are not able to synthesize COX again, because are anucleate cells and do not have a protein resynthesis system. With irreversible inhibition of COX-1, the disruption of PGA2 synthesis persists throughout the life of the platelet, for 7–10 days. Resynthesis of COX occurs in endothelial cells and activity is restored within a few hours after its irreversible inhibition by acetylsalicylic acid. Therefore, when prescribing the drug once a day, there is no significant reduction in the synthesis of prostacyclin. The antiplatelet effect of acetylsalicylic acid lasts for a shorter period of time due to the formation of new platelets. The predominant effect of acetylsalicylic acid on the synthesis of PGA2 can be achieved by selecting appropriate doses of the dosage regimen, and to achieve a stable effect it is recommended to prescribe it once a day.
Acetylsalicylic acid undergoes first-pass metabolism in the liver (~30%), as a result of which its concentration in the systemic circulation is lower than in the portal blood. As a result, acetylsalicylic acid acts on platelets circulating in the portal bloodstream in higher concentrations than on endothelial cells of systemic vessels. Therefore, to suppress the synthesis of thromboxane A2 in platelets, smaller doses of acetylsalicylic acid are required than to suppress the synthesis of prostacyclin in endothelial cells. As the dose of acetylsalicylic acid increases, its inhibitory effect on PGI2 synthesis becomes more pronounced, which may lead to a decrease in the antiplatelet effect of the drug. These features of acetylsalicylic acid must be taken into account and prescribed as an antiplatelet agent only in small doses.
Acetylsalicylic acid as an antiplatelet agent is used for the prevention of acute myocardial infarction, for unstable angina, for the prevention of ischemic stroke, for the prevention of thrombosis of peripheral vessels, in coronary artery bypass grafting and coronary angioplasty, stenting of coronary arteries, atrial fibrillation of non-rheumatic origin, pulmonary infarction, acute thrombophlebitis, active rheumatism and rheumatoid arthritis.
Acetylsalicylic acid preparations are prescribed orally in doses from 25–125 mg to 325 mg once a day for a long time.
IMPORTANT! The main side effects of acetylsalicylic acid are associated with inhibition of COX and disruption of the formation of prostaglandins E2 and I2, which have a gastroprotective effect. As a result, even with short-term use, acetylsalicylic acid can cause damage to the epithelium of the stomach and duodenum (ulcerogenic effect). When used, gastrointestinal bleeding and other hemorrhagic complications are possible. Selective inhibition of COX leads to activation of the lipoxygenase pathway for the conversion of arachidonic acid and the formation of leukotrienes, which have bronchoconstrictor properties. In patients with bronchial asthma, acetylsalicylic acid can provoke the onset of a bronchospastic attack (“aspirin asthma”). Allergic reactions are possible (anaphylactoid reaction, allergic dermatitis, angioedema, urticaria).
Antiplatelet agents in the treatment of cardiovascular diseases
Thrombosis plays a key role in the development of various cardiovascular complications. In the pathogenesis of ischemic diseases of organs and systems of the human body: coronary heart disease (CHD) [acute coronary syndrome (ACS), myocardial infarction (MI)], ischemic cerebral stroke, gangrene of the extremities and other disorders of the blood supply to organs and tissues, inflammatory and atherosclerotic vascular damage with a violation of the integrity of the intima, slowing of blood flow, an imbalance of the coagulation and anticoagulation systems and a violation of the rheological parameters of the blood.
When the vascular endothelium of various etiologies is damaged, a blood clot forms and, as a result, a critical narrowing of the lumen of the vessels or its complete closure (partial or complete occlusion). In violations of the rheological parameters of blood, the aggregation state of platelets and erythrocytes plays a leading role [1, 6, 8, 10, 17].
Modern treatment and prevention of cardiovascular complications, in particular MI, are impossible without a clear understanding of the mechanisms of thrombus formation, the material substrate of which is platelets, erythrocytes, and fibrinogen. MI - ischemic necrosis of the heart muscle - in 95% of cases develops as a result of the formation of a blood clot in the coronary artery, which is confirmed by autopsy data among those who died in the first 3 hours from the onset of pain syndrome and the results of coronary angiography in patients admitted to the hospital in the first hours of the development of myocardial disasters [10].
In the process of thrombus formation, a platelet goes through four stages: activation, release of active biological substances (thromboxanes, adenosine diphosphate ADP, serotonin, glycoprotein (GP) receptors - IIb/IIIa), aggregation and adhesion. These processes (macro- and microthrombotic formation) are especially pronounced during destabilization of coronary blood flow - ACS, including MI. Macro- and microthrombosis are based on mechanisms that stimulate the aggregation activity of platelets and erythrocytes - the presence of accelerated, turbulent blood flow in the area of the vessel narrowed by an atherosclerotic plaque, which contributes to damage to the endothelium (with the development of endothelial dysfunction) and “exposure” of collagen, one of the main factors of aggregation and platelet adhesion. Platelets come into contact with the subendothelial layer, in particular with the main adhesion stimulator - collagen, form processes with the formation of platelet conglomerates (aggregation) and stick (adhesion) to these areas, creating a white thrombus.
Platelet activation is carried out by catecholamines, thrombin, ADP, serotonin, collagen, thromboxane A2, a product of arachidonic acid metabolism.
As a result of platelet activation, the latter are released from biologically active substances (ADP, thromboxane A2, serotonin) and labilization of the platelet membrane with the formation of GP IIb/IIIa receptors under the influence of ADP and thromboxane A2.
Platelet aggregation—the formation of platelet conglomerates in the blood plasma—occurs with the activation and interaction of GP IIb/IIIa receptors through the formation of fibrin bridges between platelets.
Adhesion - the adherence of platelet conglomerates to damaged vascular intima - is controlled by von Willebrand factor.
Thus, platelet activation is a key point in the pathogenesis of cardiovascular complications, largely determining the severity of disturbances in the blood supply to organs and tissues (heart, brain, peripheral vessels), therefore antiplatelet therapy is pathogenetically justified.
Currently, there are four groups of antiplatelet drugs, the division of which is based on the principles of evidence-based medicine, taking into account the effectiveness and presence of side effects. The first group of antiplatelet drugs, the use of which is not recommended for practical cardiology due to the lack of evidence of advantages over Aspirin, ineffectiveness and potential danger: sulfinpyrazone, dipyridamole, prostacyclin, thromboxane A2 synthetase blockers, thromboxane A2 receptor antagonists, platelet IIb/IIIa receptor inhibitor drugs for use inside. The second group, which forms the basis of modern antiplatelet therapy, is cyclooxygenase (COX) inhibitors: acetylsalicylic acid (ASA) - Aspirin. The third group is thienopyridines (clopidogrel - Plavix, ticlopidine - Tiklin). The fourth group is GP IIb/IIIa receptor blockers for intravenous use (abciximab, eptifibatide, tirofiban, framone) [1, 3, 8, 9, 11, 12].
ASA has been used in medical practice for more than a hundred years. Since the 1980s, Aspirin has been actively used in clinical practice in the treatment of ACS to prevent the development of MI. Several significant studies have been conducted (VA, RISC, ISIS-2) that have convincingly demonstrated the ability of Aspirin to reduce the risk of acute MI and death from acute coronary insufficiency by 41–70%. In 2002, the Antithrombotic Trialists Collaboration published the largest meta-analysis of 287 randomized clinical trials involving 135,000 patients. The data obtained indicate the benefits of Aspirin in patients at high risk of complications. A meta-analysis convincingly shows that the use of high doses of Aspirin (500–1500 mg) has no advantage in therapeutic efficacy compared with medium (160–325 mg) and low (75–150 mg) doses and is quite often accompanied by side effects from the gastrointestinal tract. -intestinal tract (GIT). Similar results formed the basis for the postulate: the optimal dose of Aspirin for long-term prevention of cardiovascular complications in patients at high risk is in the range of 75–150 mg/day [1, 4, 8, 11, 13, 17].
The American Diabetes Association recommends the use of ASA in a dose of 81 to 325 mg for the secondary prevention of large vessel lesions in diabetic patients over 30 years of age, combined with components of the metabolic syndrome: overweight (> 120% of ideal body weight, body mass index (BMI) > 28 for women and > 27.3 for men), atherogenic dyslipidemia (triglycerides > 250 mg%, low-density lipoprotein cholesterol > 130 mg% and high-density lipoprotein cholesterol < 40 mg%), high blood pressure, family history of coronary artery disease, smoking [1, 5, 12].
In addition, a meta-analysis established the advisability of prescribing Aspirin to patients with atrial fibrillation (as an alternative to warfarin), peripheral arterial disease (carotid artery stenosis) and end-stage chronic renal failure (requiring hemodialysis).
A number of independent studies have found that in patients with ACS without ST-segment elevation of the ECG (ESSENCE, PRISM PLUS), the immediate prognosis depends on previous use of Aspirin before the development of exacerbation of coronary artery disease. Thus, in the PRISM PLUS study, during the use of Aspirin for ACS, the incidence of myocardial infarction, refractory angina and sudden death by the 7th day of observation was 12.1% among patients who had not previously taken this drug, and 23.5% among those who had not previously taken this drug. who took it before the exacerbation developed. This fact was called the “aspirin paradox,” which led DL Bhatt and EJ Topol (2004) to classify Aspirin as a “suboptimal antiplatelet agent” [12].
The mechanism of action of ASA is shown in the figure. Aspirin primarily inhibits COX of platelets and vascular endothelium, suppresses the formation of thromboxane A2 (a powerful inducer of platelet aggregation and vasoconstriction) - a product of arachidonic acid metabolism, and in high doses - the synthesis of prostacyclin (a disaggregant and vasodilator). ASA and other non-steroidal anti-inflammatory drugs (indomethacin) act at the level of arachidonic acid metabolism, and in large doses (Aspirin - from 300 to 500 mg) simultaneously block the synthesis of prostacyclin, which indirectly can maintain the aggregation state of platelets as a result of a quantitative decrease in prostacyclin and its disaggregation effect .
There are other mechanisms of action of ASA, which distinguish it from other antiplatelet drugs and determine its uniqueness. Aspirin has an inhibitory effect on fibrin formation through suppression of thrombin formation (FII → FIIa) and the functional state of fibrinogen FI (blocks lysine in fibrinogen molecules). At the same time, ASA is able to activate fibrinolysis through the release of plasminogen activators and “loosening” fibrin fibers [3].
In recent years, the problem of resistance to Aspirin therapy has been actively discussed, which is understood as the inability of the drug in some patients to adequately suppress platelet function, reduce the synthesis of thromboxane A2 and/or prolong bleeding time. The prevalence of resistance to Aspirin therapy, according to various studies, ranges from 10 to 45% [2, 7, 17]. Among the possible reasons for this phenomenon are the following:
- pharmacodynamic interactions of Aspirin with non-steroidal anti-inflammatory drugs;
- the presence of non-platelet sources of thromboxane A2 synthesis (endothelium, monocyte/macrophage COX-2);
- expression of COX-2 in newly formed platelets;
- hydrolysis of Aspirin by esterases of the gastrointestinal mucosa;
- increased synthesis of thromboxane A2;
- hyperlipidemia;
- genetic features.
There is reason to believe that resistance to Aspirin therapy may be associated with polymorphism of the COX gene affecting the active center of the enzyme (Ser529), polymorphism of genes encoding other enzymes involved in the mobilization and metabolism of arachidonic acid (phospholipases, thromboxane synthetase) and polymorphism of genes encoding other Platelet GP receptors [7].
The most promising in terms of the effectiveness of prevention and treatment of thrombosis is the use of ASA in combination with thienopyridines [6, 9, 12, 13, 17, 18].
ASA, dipyridamole, sulfinpyrazone have a number of side effects that reduce their therapeutic effect, therefore, currently the group of thienopyridines - Aspirin synergists - is of interest for practical medicine. According to the TASS (Ticlopidine Aspirine Stroke Study) study, which was performed to compare the preventive activity of ticlopidine (500 mg/day) and ASA (1300 mg/day) in patients with coronary artery disease, the effectiveness of ticlopidine was significantly higher with fewer side effects: the risk of stroke and MI in the group of patients taking ticlopidine was 24% lower in the first year of observation compared to the group of patients taking only Aspirin at the indicated dose [9, 11, 12, 13, 17].
The mechanism of action of thienopyridines is mediated through the blockade of platelet P2Y12 receptors, which prevents the stimulating effect of ADP on them and the subsequent activation of GP IIb/IIIa receptors.
Experimental studies of the mechanisms of action of thienopyridines have shown that the drugs are highly effective only in vivo. Unlike ASA, which inhibits only the second phase of platelet aggregation induced by ADP, ticlopidine inhibits both phases - aggregation and adhesion. Thienopyridines also inhibit platelet activation caused by collagen, epinephrine, thrombin and serotonin. At the same time (unlike ASA), they do not affect the metabolism of arachidonic acid and, thus, do not affect the synthesis of prostacyclin by the vascular endothelium [1, 11].
In addition to the above, thienopyridines increase the plasticity (deformability) of erythrocytes, helping to improve the rheological properties of blood and microcirculation, which is confirmed in our studies: an increase in the electrophoretic mobility of erythrocytes under the influence of ticlopidine at a dose of 400 mg/day was noted; at the same time, the drug lowered blood viscosity by reducing plasma fibrinogen [9].
Currently, significant clinical experience has been accumulated in the use of thienopyridines in various cardiovascular pathologies: ACS, stroke, obliterating atherosclerosis of the vessels of the lower extremities and diabetic angiopathy. In the CAPRIE study, when comparing the effectiveness of clopidogrel and Aspirin for the secondary prevention of cardiovascular complications, the rates of ischemic stroke, MI and death from sudden heart failure per year in the groups of patients using clopidogrel and Aspirin also demonstrated a decrease in the relative risk of developing these complications against the background taking clopidogrel by 8.7%. Clopidogrel belongs to the group of thienopyridines and has the most complete antithrombotic effect; with a loading dose of 300 mg (600 mg), its effect begins 2–4 hours from the start of taking the drug and reaches its maximum antiplatelet effect by the end of the second or third day of treatment. Ticlopedine is currently rarely used in the treatment of ACS due to the delayed onset of antiplatelet action, the lack of a calibrated loading dose, and the more frequent development of complications than clopidogrel - neutropenia, thrombocytopenia, liver dysfunction [1, 11, 13].
The best results were obtained with combined treatment with thienopyridines in combination with Aspirin, which made it possible to reduce the therapeutic doses of these drugs, reduce the number of side effects and reduce the cost of treatment.
The CATS (Canadian-American Ticlopidin Study) study, which included 1053 patients who had recently (within the last 4 months) episodes of ischemic attacks, demonstrated a 30.2% reduction in the risk of developing MI, recurrent stroke and death from cardiovascular failure. [1, 8, 11, 12].
Similar results were presented by French scientists YC Aican et al. (1989), similar data were obtained from the Swedish multicenter STIM study. French researchers followed 169 patients, and the STIM study included 687 patients with intermittent claudication. Ticlopidine was prescribed according to the standard method at a dose of 250 mg/day with the addition of 75–100 mg of Aspirin per day. In both observation groups, the number of vascular complications decreased by 38–40% (with a simultaneous improvement in peripheral blood flow).
The CLARITI-TIMI 28 study, when clopidogrel was added to standard aspirin therapy in 3491 patients with ST-segment elevation ACS by day 30 of treatment, documented a 20-fold reduction in the risk of death from cardiovascular failure, myocardial infarction, and recurrent ischemia (requiring emergency revascularization). % compared to the group of patients treated with placebo. Similar results were obtained in the COMMIT-CCS-2 study, which included 45,852 patients receiving ASA 162 mg per day and clopidogrel 75 mg per day: the risk of sudden death, recurrent MI and stroke decreased by 10% during hospital stay [1].
Thus, at present, the most preferable (compared to monotherapy) in terms of effectiveness in preventing episodes of ischemia, the development of MI and the cost of treating patients with ACS is the use of thienopyridines (clopidogrel - once with a loading dose of 300 mg, then 75 mg/day) in combination with Aspirin (100 mg/day) for 9–12 months, since they are powerful inhibitors of aggregation and adhesion of platelets and erythrocytes, and therefore effective antithrombotic agents used in cardiological practice, with minimal side effects.
In acute situations of ACS, when performing balloon angioplasty with stenting, the effectiveness of antiplatelet therapy increases when using a combination of ASA with clopidogrel and/or GP IIb/IIIa receptor antagonists. In these situations, loading doses of antiplatelet drugs are used (Aspirin - 150-300 mg, clopidogrel - 300-600 mg once) followed by a transition to maintenance doses (Aspirin - 75-150 mg/day, clopidogrel 75 mg/day) for 12 months .
The CHARISMA study, which examined the effectiveness of therapy by adding clopidogrel at a dose of 75 mg/day to standard therapy with Aspirin 75–150 mg/day over a long period of time (over one year) in 15,603 patients with chronic forms of cardiovascular disease, showed results similar compared to the group of patients receiving ASA monotherapy (7.3%)—a reduction in the incidence of myocardial infarction, stroke, and death from sudden heart failure to 6.8% with minimal complications from the gastrointestinal tract [1].
The main clinical problem with the use of Aspirin, in addition to the risk of bleeding (especially in elderly patients), is complications from the gastrointestinal tract in the form of the development of dyspeptic disorders and erosive-ulcerative gastritis. Erosive and ulcerative changes in the gastrointestinal mucosa while taking ACS in standardized doses used in cardiological practice are a well-known fact [14, 15, 16, 18, 19].
For a long time, many clinicians considered the only and almost 100% solution to this problem to be the use of enteric-soluble forms of ASA: Thrombo ACC, Aspifat, Aspirin-S, Aspirin Upsa, etc. However, according to the results of recent studies, the formation of erosions and gastric ulcers has been noted even with the use of enteric-coated aspirin (they scarred in 90% of cases when using cimetidine and antacids only after discontinuation of these forms) [18, 19].
Relatively little known are the recently described lesions of the small and large intestines caused by Aspirin and other non-steroidal anti-inflammatory drugs: hidden and obvious bleeding, perforation, strictures, exacerbation of chronic enterocolitis. The frequency of these complications is significantly less than those localized in the stomach and the initial part of the duodenum. However, they also have a negative impact on the practical significance of Aspirin in the prevention of ischemic attacks.
Lesions of the small intestine in the form of enteropathies when taking ASA were more common than in the control group of patients (who did not take Aspirin). The most common were diaphragm-like strictures (small bowel obstruction syndrome) and aspirin-induced enteropathy (a syndrome characterized by intestinal bleeding, protein loss and malabsorption).
Pathological changes in the large intestine when taking non-steroidal anti-inflammatory drugs are of two types:
- in a previously unchanged large intestine (acute colitis, single ulcers-erosions in the cecum, colon, sigmoid colon);
- in a previously altered intestine (perforation due to diverticulosis, exacerbation of chronic inflammatory processes).
The issues of preventing damage to the gastrointestinal mucosa when prescribing ASA have not been fully studied and remain relevant in clinical practice. At present, according to the literature, it is only obvious that the use of enteric-soluble forms of ASA does not solve this problem.
All of the above poses the challenge for pharmacologists and clinicians to create and introduce into clinical practice new forms of drugs that can protect the gastrointestinal tract from the damaging effects of oral non-steroidal anti-inflammatory drugs.
Aspirin-induced complications in the gastrointestinal mucosa dictate its abolition and the prescription of cytoprotectors - antacids. A number of clinical and experimental studies have shown that antacids are effective in the treatment and prevention of erosions and ulcers of the gastric mucosa when using non-steroidal anti-inflammatory drugs. It has been demonstrated that the cytoprotective effect of antacids is realized through stimulation of the formation of prostaglandins in the gastric wall (a decrease in the level of prostaglandins in the gastric mucosa is the main mechanism of the erosive-ulcerative process caused by the use of Aspirin), increased secretion of bicarbonates and an increase in glycoproteins in the gastric mucosa.
Of particular interest is the drug Cardiomagnyl, which is a combination of ASA (in the most effective and safe doses - 75 and 150 mg) with a non-absorbable antacid - magnesium hydroxide [3].
Non-absorbable antacids are one of the most commonly used drugs in gastroenterological practice in the treatment of stomach diseases, including peptic ulcers. They realize their positive effect through the absorption of hydrochloric acid in the stomach. In addition, non-absorbable antacids have a number of other positive effects: they reduce the proteolytic activity of gastric secretions (adsorb pepsin, reduce its activity by increasing the pH of the environment), have an enveloping property, bind lysolecithin and bile acids, which have an adverse effect on the gastrointestinal mucosa.
Magnesium hydroxide, which is part of Cardiomagnyl, acts faster than aluminum hydroxide, which is extremely important when using this drug in antiplatelet treatment. ASA is quickly absorbed from the gastrointestinal tract: therapeutic concentrations of Aspirin in the blood plasma are achieved 15–20 minutes after taking the drug, while special studies have shown that magnesium hydroxide in the composition of Cardiomagnyl does not affect the rate of absorption of ASA [3, 10].
Cardiomagnyl is indicated:
- elderly people (after 60 years);
- patients with ischemic heart disease;
- patients suffering from cerebrovascular diseases;
- patients who have suffered heart attacks and strokes;
- middle-aged people (35–50 years old) who have a high risk of cardiovascular disease.
Doses and methods of use of Cardiomagnyl:
- for primary prevention: the first 2–3 days, 150 mg, then 75 mg/day in the evening after meals;
- for secondary prevention and treatment: 150 mg/day for a long time.
Thus, the prevention of thrombosis and thromboembolism, which constitute a key point in the development of cardiovascular pathologies (ACS, acute MI, ischemic strokes, pulmonary embolism, kidney damage, peripheral angiopathies), with the help of antiplatelet drugs is the determining direction in the treatment of patients in therapeutic and surgical practice. Thienopyridines (in particular, clopidogrel (Plavix)), ASA contribute to the active prevention of thromboembolism, and their combination allows you to reduce the amount of the drug taken with an increase in therapeutic activity and a decrease in side effects.
Cardiomagnyl, the first combination of ASA (antiplatelet agent) and magnesium hydroxide (antacid component) used in Russia, eliminates the ulcerogenic and dyspeptic effects of Aspirin, which makes it possible to recommend it for use in widespread practice in the treatment and prevention of cardiovascular pathologies.
For questions regarding literature, please contact the editor.
A. M. Shilov, Doctor of Medical Sciences, Professor S. A. Knyazeva , Candidate of Medical Sciences S. A. Matsevich MMA named after. I. M. Sechenova, Moscow
Modern antiplatelet therapy: place of ticagrelor in clinical guidelines
The leading cause of mortality worldwide is still cardiovascular pathology, despite the high level of development of cardiology over the past decades [1, 2]. The various clinical manifestations of vascular pathology are based on a common anatomical substrate in the form of dysfunction of the arterial endothelium, chronic inflammation and damage to the cap of the atherosclerotic plaque, slowing of blood flow, and the formation of an intravascular thrombus [3]. In this regard, reducing the risk of developing thrombotic complications is the main task that a doctor who wants to increase the duration and improve the quality of life of patients with cardiovascular diseases should set.
The pathogenesis of thrombosis includes three main points for drug action: platelet link - the action of antiplatelet agents, the coagulation system - the zone of action of anticoagulants, fibrin - the action of fibrinolytics. Platelets are the first to respond to the rupture of an atherosclerotic plaque, launching a coagulation cascade; they are a source of active synthesis of humoral factors that simultaneously stimulate the processes of thrombus formation and inflammation. According to a meta-analysis of 287 randomized studies on secondary prevention and 6 studies on primary prevention, the use of antiplatelet therapy can reduce the risk of non-fatal myocardial infarction and non-fatal cerebral infarction by 23% [4]. This meta-analysis confirms that the leading role in the prevention of complications of atherosclerosis should be given to antiplatelet agents.
Antiplatelet agents are medications that prevent thrombosis by reducing the functional activity of platelets. To date, more than 20 different drugs are known that can inhibit platelet function through various mechanisms of action. However, during many years of practice and clinical studies, effectiveness was confirmed only for cyclooxygenase inhibitors (acetylsalicylic acid), adenosine diphosphate (ADP) receptor blockers - P2Y12 (clopidogrel, prasugrel, ticagrelor), phosphodiesterase inhibitors (dipyridamole) and glycoprotein IIb-IIIa antagonists for intravenous use (abciximab, tirofiban, eptifibatide). Activation of platelets and their subsequent aggregation occur under the influence of various mediators, the most important of which are thromboxane A2 and ADP, therefore acetylsalicylic acid (ASA) and ADP inhibitors (clopidogrel, prasugrel, ticagrelor) are most widely used.
The history of the creation of the class began with the discovery of the antiplatelet properties of ASA. In 1987, the first randomized Canadian trial was published involving 585 stroke patients treated with ASA for 26 months. The study demonstrated the effectiveness of ASA against recurrent stroke [5]. This was the reason that in 1980, the US Food and Drug Administration (FDA) approved ASA for the treatment of patients after stroke. Subsequently, the effectiveness of ASA in reducing the risk of death and recurrent myocardial infarction in patients with unstable angina and non-ST segment elevation myocardial infarction was proven [4]. Thus began the era of antiplatelet therapy and its first worthy representative - acetylsalicylic acid.
Acetylsalicylic acid blocks platelet activation by inhibiting cyclooxygenase (COX), preventing the formation of thromboxane A2. Platelets are anucleate cells, so they lack the ability to synthesize proteins. Irreversible inhibition of COX-1, the impossibility of its resynthesis due to the absence of a nucleus, as well as the daily renewal of the platelet pool by only 10% lead to the fact that the blockade of thromboxane synthesis during ASA therapy persists throughout the platelet life span, up to 10 days. Complete suppression of thromboxane production is achieved with constant long-term administration of ASA in doses ≥ 75 mg/day. In most patients with stable coronary heart disease (CHD), low-dose ASA is preferable due to its favorable benefit-risk ratio. ASA for this category of patients remains the basis of drug prevention of arterial thrombosis [6]. The damaging effect of ASA on the gastrointestinal tract (GIT) increases as the dose increases. The drug is recommended for all patients with an established diagnosis of coronary artery disease without any restrictions on the duration of use. The optimal benefit-risk ratio is achieved when using ASA in a dose range from 75 to 150 mg/day; when used as part of dual antiplatelet therapy, the dose is 75–100 mg.
However, in recent years, the problem of resistance to ASA therapy has been actively discussed, which is understood as the inability of the drug in some patients to adequately suppress platelet function, reduce the synthesis of thromboxane A2 and/or prolong bleeding time. The prevalence of resistance to ASA therapy, according to various studies, ranges from 10% to 45% [7]. Among the possible reasons for this phenomenon are the following:
- pharmacodynamic interactions of ASA with non-steroidal anti-inflammatory drugs (NSAIDs);
- the presence of non-platelet sources of thromboxane A2 synthesis;
- expression of COX-2 in newly formed platelets;
- hydrolysis of ASA by esterases of the gastrointestinal mucosa;
- increased synthesis of thromboxane A2;
- hyperlipidemia;
- genetic features.
A number of independent studies have found that in patients with acute coronary syndrome (ACS) without ST segment elevation (ESSENCE, PRISM PLUS), the immediate prognosis depends on previous use of ASA before the development of exacerbation of coronary artery disease. Thus, in the PRISM PLUS study, when using ASA for ACS, the incidence of myocardial infarction, refractory angina and sudden death by the 7th day of observation was 12.1% among patients who had not previously taken ASA, and 23.5% among those taking ASA before the development of an exacerbation. This fact was called the “aspirin paradox,” which led DL Bhatt and EJ Topol (2004) to classify ASA as “suboptimal antiplatelet drugs” [8, 9]. All this contributed to the development and study of new antiplatelet drugs - ADP P2Y12 receptor inhibitors and the identification of approaches to dual antiplatelet therapy.
The group of ADP-P2Y12 receptor blockers includes the drugs ticlopidine, clopidogrel, prasugrel, and ticaglerol. These drugs inhibit platelet aggregation induced by adenosine diphosphate by causing changes in the platelet ADP receptor, which is called P2Y12 [9]. There are significant differences between the drugs listed above, for example, irreversible inhibitors of P2Y12 receptors include thienopyridines (ticlopidine, clopidogrel and prasugrel), and reversible inhibitors include triazolopyridines (ticagrelor). Comparative characteristics of the drugs are presented in table. 1.
Clopidogrel is the most well-known and actively used antiplatelet agent after ASA in domestic medicine today [10]. The results of large clinical trials have proven the effectiveness of reducing the incidence of complications in a wide range of patients with coronary artery disease when adding clopidogrel to ASA [11, 12], which served as the basis for the development of indications for dual antiplatelet therapy in patients with ACS without ST elevation, as well as after coronary artery bypass grafting (CABG) and percutaneous coronary intervention (PCI) for the prevention of thrombosis [13].
Clopidogrel, as can be seen from the table, is a prodrug; the drug has a complex metabolism. The absorption of clopidogrel in the intestine is controlled by a special protein (P-glycoprotein), encoded by the ABCB1 gene, in this regard, only about 15% of the absorbed clopidogrel in the liver is converted into an active metabolite. The process is two-step (oxidation and hydrolysis), depending on several isoenzymes of the cytochrome P450 system, the most important of which are CYP2C19 and CYP3A4 [14]. Despite the wide evidence base for the effectiveness of this drug, clopidogrel has a number of disadvantages, which include a delayed antiplatelet effect, since it is a prodrug and requires time to activate; maximum suppression of ADP receptors occurs only on the 4th–5th day of regular use. In addition, there is variability in the antithrombotic effect of clopidogrel in different patients, which may be due to a number of pharmacokinetic factors, including insufficient loading and maintenance doses of the drug, impaired absorption and formation of the active metabolite, drug interactions, in particular with proton pump inhibitors, which are often prescribed for the prevention of bleeding from the upper gastrointestinal tract [15, 16].
Due to the existing shortcomings of clopidogrel and the inability to solve this problem, the need to create a new drug from the group of ADP receptor blockers - P2Y12 - became obvious to the world community.
A new antiplatelet drug is ticagrelor, a direct-acting reversible antagonist of P2Y12 receptors. The drug is an active substance that is metabolized via the CYP3A4 isoenzyme to form an active metabolite. The degree of inhibition of P2Y12 receptors is determined primarily by the plasma levels of ticagrelor and, to a lesser extent, its active metabolite. The half-life is about 12 hours, and therefore the drug is prescribed twice a day. Ticagrelor has a faster onset of therapeutic action and provides a more pronounced and persistent inhibition of platelet activation compared to clopidogrel. At the same time, recovery of platelet function after discontinuation of ticagrelor occurs faster compared to clopidogrel. The presence of more attractive pharmacological properties, as well as existing problems associated with taking clopidogrel, were the main reasons for organizing the large-scale PLATO (Platelet inhibition and patient outcomes) study, which compared the effectiveness and safety of ticagrelor compared with clopidogrel in patients with ACS [17] . According to a study published on August 30, 2009 at the Congress of the European Society of Cardiology (ESC), the new antithrombotic drug ticagrelor is more effective than clopidogrel in treating patients with acute coronary syndrome and does not increase the risk of bleeding.
Researchers led by Lars Wallentin randomized 18,624 patients with ACS hospitalized between 2006 and 2008 at 862 hospitals included in the PLATO trial. Patients were divided into 2 groups: in the first group, patients received ticagrelor (180 mg loading dose and 90 mg twice a day), in the other - clopidogrel (300 or 600 mg loading dose and 75 mg daily). All patients also took ASA at a dose of 75–100 mg. The groups were carefully balanced taking into account baseline clinical parameters, concomitant diseases and treatment tactics. 37.5% of patients had acute myocardial infarction with ST segment elevation, 42.9% had acute myocardial infarction without ST segment elevation, and 16.6% had unstable angina. The duration of medication use ranged from 6 to 12 months, with an average of 277 days. The results showed that with ticagrelor compared with clopidogrel there was a significant reduction in the total number of primary endpoints (cardiovascular death, myocardial infarction or stroke): 9.8% versus 11.7%, a risk reduction of 16%, p < 0.001. In those receiving ticagrelor, compared with those treated with clopidogrel, there was a significant decrease in the incidence of myocardial infarction: from 6.9% to 5.8%, and cardiovascular death - from 5.1% to 4%. At the same time, the total number of strokes was the same in both subgroups: 1.5% and 1.3%. The incidence of the combined secondary endpoint (death from vascular causes, myocardial infarction, stroke, recurrent myocardial ischemia, transient ischemic attack or other types of arterial thrombosis), as well as death from all causes, was significantly lower in the ticagrelor group compared with clopidogrel: 14.6 % versus 16.7% and 4.5% versus 5.9%, respectively. There were no significant differences between the groups in the incidence of major bleeding or fatal or life-threatening bleeding. It is interesting to note that the risk of major bleeding, including fatal intracranial bleeding not related to the CABG procedure, was slightly higher in the ticagrelor group compared with clopidogrel (4.5% vs. 3.8%, p = 0.03). However, the incidence of CABG-related bleeding was lower among those receiving ticagrelor (7.4% vs. 7.9%) [18].
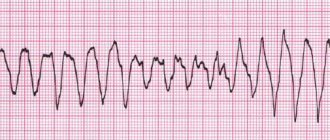
The results of 13,408 (72%) patients with an invasive treatment strategy planned at the randomization stage were analyzed separately [18]. 49.1% of patients were diagnosed with acute coronary syndrome with ST segment elevation on electrocardiography (ECG) and 50.9% with acute coronary syndrome without ST segment elevation on ECG. During the first hospitalization, PCI was performed in 10,298 (72%) patients and CABG in 782 (5.8%). The average time to PCI was 2.4 (0.8–20.1) hours after randomization in patients with ACS without ST segment elevation on the ECG and 0.5 (0.2–1) hours in patients with ACS with ST segment elevation on the ECG . The median time to CABG was 6 (3–10) days. The total number of myocardial infarctions, strokes and cardiovascular deaths during therapy with ticagrelor decreased to 9% (clopidogrel - by 10.7%), i.e., the risk reduction was 16%, p < 0.0025.
It is important to emphasize that the benefit of ticagrelor on the primary endpoint was observed in different subgroups and was independent of the loading dose of clopidogrel. Major bleeding was equally common in those treated with ticagrelor and those treated with clopidogrel (11.6% vs. 11.5%). The incidence of stent thrombosis was significantly lower in the ticagrelor group, both with and without drug-eluting stents. The incidence of certain stent thrombosis in patients receiving ticagrelor was significantly lower at both 30 days and 360 days of follow-up compared with those treated with clopidogrel, including those patients taking a loading dose of 600 mg or more.
In a substudy analysis of 1,261 patients undergoing CABG within 7 days of the last study drug dose, there was no significant difference in the reduction in primary endpoints (10.6% in the ticagrelor group and 13.1% in the clopidogrel group). Moreover, among those taking ticagrelor, there was a significant decrease in overall mortality by 51%, and cardiovascular mortality by 48%, both in the early and late periods after surgery [19].
Thus, PLATO was the first large-scale study to demonstrate the clinical effectiveness of ticagrelor in reducing the incidence of major vascular events in patients with ACS, without a significant increase in the risk of bleeding. A more significant reduction in the risk of thrombotic episodes during therapy with ticagrelor appears to be due to more rapid and intense inhibition of platelet P2Y12 receptors. When a loading dose of 600 mg of clopidogrel is administered, it takes 2–4 hours to achieve 50% inhibition of platelet aggregation, and the same effect is achieved after 30 minutes when taking 180 mg of ticagrelor. In addition, there is a fairly large group of patients with the presence of defective variants of alleles of the cytochrome P450 system, which is associated with a slowdown in the formation of the active metabolite of clopidogrel, insufficient suppression of platelet function when taking it, as well as with a higher risk of cardiovascular complications after acute coronary syndrome and during PCI. The advantages of ticagrelor also include the reversible nature of inhibition of platelet P2Y12 receptors, which means a more rapid cessation of the antiplatelet effect after discontinuation of the drug. This circumstance seems important during invasive interventions, as well as before the upcoming CABG procedure. Although the incidence of major bleeding was no lower with ticagrelor than with clopidogrel, it should be noted that the greater inhibition of platelet function was not associated with an increase in the incidence of major bleeding. This distinguishes ticagrelor from prasugrel, whose more pronounced antiplatelet effect is accompanied by an increased risk of major bleeding.
The European Society of Cardiology recommended the use of ticagrelor (at a loading dose of 180 mg and 90 mg 2 times a day as a maintenance dose) to all patients with ACS, regardless of the planned treatment strategy (invasive or conservative) as first-line therapy. If patients received clopidogrel at the very beginning of the disease, it should be replaced with ticagrelor. Taking clopidogrel in patients with ACS with invasive or conservative strategies is possible only in cases of absence or intolerance to ticagrelor or prasugrel. The duration of therapy with P2Y12 receptor inhibitors in patients who have suffered acute coronary syndrome is 12 months. In patients on therapy with P2Y12 receptor inhibitors, in cases of planned surgery (including CABG), ticagrelor and clopidogrel are discontinued 5 days before, and prasugrel 7 days before. Dual antiplatelet therapy is mandatory while taking ASA at a dose of 75–100 mg/day [13]. The use of dual antiplatelet therapy in stable coronary artery disease could provide more effective prevention of coronary thrombosis. However, in the CHARISMA study, which included stable patients with atherosclerotic lesions of various vascular territories or multiple cardiovascular risk factors, the addition of clopidogrel to ASA did not bring additional benefit [20]. The 2013 European Society of Cardiology guidelines indicate that dual antiplatelet therapy is beneficial only in certain categories of patients at high risk of ischemic events. Routine administration of this therapy to patients with stable coronary artery disease is not recommended [21].
Thus, atherothrombosis is the cause of high mortality in patients with cardiovascular diseases throughout the world. One of the key points of therapy is the competent prescription of antiplatelet drugs. The main effective oral drugs prescribed in clinical practice are ASA, clopidogrel, ticagrelor, prasugrel. In table Figure 2 presents an algorithm for selecting antiplatelet agents. Modern cardiology is actively developing, and one can hope that new facets of known drugs and the development of new ones will help doctors in the daily fight against cardiovascular diseases.
Literature
- Singh, VV, Toskes PP Small Bowel Bacterial Overgrowth: Presentation, Diagnosis, and Treatment // Curr Treat Options Gastroenterol. 2004. Vol. 7(1). R. 19–28.
- McMurray JJ, Adamopoulos S, Anker SD et al. Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology // Eur. Heart J. 2012. Vol. 33 (14). P. 1787–1847.
- Uster V., Fallon JT, Badimon JJ et al. The unstable atherosclerotic plaque: clinical significance and therapeutic intervention // Thrombosis and Hemostasis. 1997. Vol. 78(1). P. 247–255.
- Antithrombotic Trialists' Collaboration. Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial infarction? And stroke in high-risk patients // BMJ. 2002. Vol. 324. P. 71–86.
- A randomized trial of aspirin and sulfinpyrazone in threatened stroke. The Canadian Cooperative Study Group // N. Engl. J. Med. 1978. Vol. 299(2). P. 53–59.
- ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines // Circulation. 2012. Vol. 126. P. 354–471.
- Ushkalova E. A. Aspirin resistance: mechanisms of development, methods of determination and clinical significance // Farmateka. 2006. No. 13 (128). pp. 35–41.
- Ainetdinova D. Kh., Udovichenko A. E., Sulimov V. A. The role of antiplatelet therapy in the primary and secondary prevention of cardiovascular diseases // Effective pharmacotherapy in cardiology and angiology. 2007. No. 2. pp. 36–41.
- Shalaev S.V. Antiplatelet agents in the treatment of acute coronary syndromes // Pharmateka. 2003. No. 312. pp. 94–97.
- Kei A.A., Florentin M. et al. Antiplatelet Drugs: What comes next? // Clin. Applied Thrombosis // Hemostasis. 2011. Vol. 17(1). P. 9–26.
- Patrono C., Baigent C., Hirsh J. On behalf of the American College of Chest Physicians. Antiplatelet drugs: American College of Chest Physicians evidence-based clinical practice guidelines (8 th edition) // Chest 2008. Vol. 133(6). P. 1995–2335.
- Steg G., James SK, Atar D. et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation The Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) // European Heart Journal. 2012. Vol. 33. R. 2569–2619.
- ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST segment elevation. The Task Force for the management of acute coronary syndromes in patients presenting without persistent ST segment elevation of the European Society of Cardiology // Eur. Heart J. 2011. Vol. 32. P. 2999–3054.
- Cattaneo M. ADP receptors antagonists. In Michelson AD, ed Platelets. San Diego, Calif.: Academic Press. 2006. P. 1127–1144.
- Snoep JD, Hovens MM Clopidogrel nonresponsiveness in patients under-going percutaneous coronary intervention with stenting: a systematic review and meta-analysis // Am. Heart J. 2007. Vol. 154. P. 221–231.
- Norgard NB, Mathews KD, Wall GC Drug-drug interaction between clopidogrel and the proton pump inhibitors // Ann. Pharmacother. 2009. Vol. 43. P. 1266–1274.
- Wallentin L., Becker RC, Budaj A. et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes // N. Engl. J. Med. 2009. Vol. 361. P. 1045–1057.
- Cannon CP, Harrington RA, James S. et al. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomized double–blind study // Lancet. 2010. Vol. 375 (9711). P. 283–293.
- Held C., Asenblad N., Bassand JP et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes undergoing coronary artery bypass surgery, results from the PLATO // J. Amer. Coll. Cardiol. 2011. Vol 57. P. 672–684.
- Bhatt DL, Flather MD, Hacke W. et al. Patients with prior myocardial infarction, stroke, or symptomatic peripheral arterial disease in the CHARISMA trial // J. Am. Coll. Cardiol. 2007. Vol. 49. P. 1982–1988.
- ESC guidelines on the management of stable coronary artery disease. The Task Force on the management of stable coronary artery disease of the European Society of Cardiology // Eur. Heart J. 2013. Vol. 38. P. 2949–3003.
G. I. Nechaeva1, Doctor of Medical Sciences, Professor O. V. Drokina, Candidate of Medical Sciences N. I. Fisun, Candidate of Medical Sciences
State Budgetary Educational Institution of Higher Professional Education Omsk State Medical Academy of the Ministry of Health of the Russian Federation, Omsk
1 Contact information
* The drug is not registered in the Russian Federation.