Shortness of breath, constant weakness, unexplained swelling, chest pain - grounds for a cardiological examination. The listed phenomena may indicate a risk of chronic heart failure. The first mild symptoms should not be ignored. Without appropriate therapy, the condition will worsen. The IMMA medical clinics provide therapeutic and cardiological appointments.
In our clinics you can:
- Get a consultation with a cardiologist;
- Take an ECG and get a professional interpretation of the results;
- Complete the ABPM procedure;
- Undergo Holter monitoring;
- Take advantage of other services of our clinics.
For more details and any questions, please contact the number listed on the website
Congestive heart failure - decreased contractions of the heart muscle. This pathological condition is not an independent disease, it is a consequence of various disorders of the cardiovascular system.
The prevalence of heart failure among the population is constantly growing, the disease is considered a social problem along with oncology and AIDS. The reasons for the spread are different: poor environmental conditions, sedentary lifestyle, ignoring healthy eating rules, bad habits. Inattention to health leads to various damage to the circulatory system. Heart failure is a common complication.
About the structure of the cardiovascular system
The heart is a unique organ on which human life depends. It works without rest, has its own control center, which sends electrical impulses that stimulate muscle contractility.
The structure of the heart is widely known: it has two ventricles and two atria. By contracting, they ensure blood circulation through two vascular systems: the small and large blood circles. To more accurately explain the characteristics of different types of heart failure, it is necessary to mention the characteristics of blood flow.
The systemic circulation involves the flow of blood from the left ventricle into the aorta, oxygenation of all important organs and limbs and the return of venous blood to the right atrium. The pulmonary circulation is the flow of blood from the right ventricle to the lungs and the movement of oxygenated blood into the left atrium.
Symptoms of heart failure depend on which part of the heart is affected. This is reflected in disruption of the functioning of blood circulation.
Heart failure, depending on the nature of its course, can be of two types. The chronic form develops over a long period of time and has several stages. Acute heart failure progresses rapidly. The duration of the process is from an hour to two days. This condition requires urgent hospitalization.
The classification of heart failure based on the localization of the pathology distinguishes several types:
- Left ventricular failure;
- Right ventricular failure
- Total form.
As the disease progresses, isolated variants lead to the formation of a general, total form of the lesion. Damage to the left ventricle causes disturbances in the systemic circulation. Pathology of the right ventricle - affects the lungs or pulmonary circulation.
Synonyms:
- encephalopathy,
- chronic cerebral ischemia,
- slowly progressive cerebrovascular accident,
- chronic ischemic brain disease,
- cerebrovascular insufficiency,
- vascular encephalopathy,
- atherosclerotic encephalopathy,
- hypertensive encephalopathy,
- atherosclerotic angioencephalopathy,
- vascular (atherosclerotic) parkinsonism,
- vascular (late) epilepsy,
- vascular dementia.
The most widely used term in domestic neurological practice is “dyscirculatory encephalopathy ,” which retains its meaning to this day.
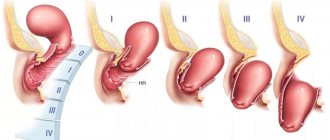
Degrees of chronic pathology
There are several degrees of chronic heart failure. The earlier a problem is identified, the easier it is to treat. In the later stages of the disease, mortality is 50%.
The first stage of chronic insufficiency is characterized by shortness of breath and rapid fatigue after active physical work or sports. Treatment at this time is most effective. Early detection of symptoms of chronic deficiency will not only help to cope with it, but also to determine the true cause.
In the second stage of heart failure, symptoms become more pronounced:
- cyanosis, or blue discoloration of the fingertips, nose and nasolabial folds, lips. The reason is a change in blood composition, insufficient oxygen content.
- With low-intensity loads, typical symptoms appear: shortness of breath, rapid heartbeat, weakness.
- Dry cough not associated with a cold.
The second stage is characterized by damage to the pulmonary circulation, the lungs suffer, so a cough occurs, and the blood is poorly saturated with oxygen.
Another variant of the manifestation of the second stage is damage to the systemic circulation. First of all, swelling appears. They can be hidden: fluid accumulates in body cavities, for example, filling the abdominal cavity. Swelling of the legs is more noticeable. This condition is called dropsy.
In addition, stagnation begins in all organs: liver, kidneys, digestive system, brain. Associated pathologies develop and the functioning of these organs is disrupted.
At the third stage, irreversible changes occur. Usually the functioning of the entire circulatory system is disrupted. Lesion of the small circle is characterized by a strong cough with sputum production, the appearance of pink foam not only when coughing, but also at rest. This is explained by a violation of the permeability of numerous vessels, lymphatic fluid fills the lungs, and edema occurs. The condition is fatal and requires urgent hospitalization. Shortness of breath accompanies a person at rest. Worsens when lying down. Periodically there are attacks of suffocation, accompanied by fear of death. They force the patient into a sitting position with his legs down.
At the same time, all vital organs suffer. Signs of congestive liver damage:
- increase in organ volume;
- formation of sclerotic and connective tissue;
- cirrhosis of the liver.
Congestive kidney damage leads to chronic renal failure. At the same time, the amount of urine excreted decreases, swelling increases and no longer goes away under the influence of medications. Intestinal dysfunction occurs, constipation or diarrhea is possible.
The third stage is irreversible. A person completely loses the ability to be active. Even household chores become beyond his power. Usually the patient is assigned a certain form of disability. The survival rate in this case is 50%. Medicine in this case can only offer supportive therapy.
Important! The third stage of the formation of congestive heart failure occurs as a result of the lack of treatment for the disease. If you consult a doctor in a timely manner in the early stages, you can not only stop the progression of the disease, but also be completely cured.
If you notice the following signs of heart failure, you should immediately contact a cardiologist:
- Shortness of breath with minor physical exertion;
- Blueness of fingers, lips, nose;
- Unreasonable dry cough, sometimes accompanied by sputum production;
- Pain in the chest, under the shoulder blade;
- Swelling of the legs, enlargement of the abdomen, which may be hidden edema.
Mild heart failure responds well to treatment, so a preventive examination by a therapist and cardiologist and the necessary diagnostic methods will help avoid serious consequences.
Kidney failure
Pyelonephritis
Diabetes
4195 07 October
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Kidney failure: causes, symptoms, diagnosis and treatment methods.
Definition
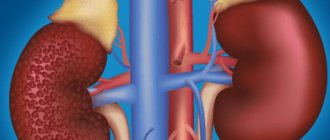
Kidney failure is a condition in which one or both kidneys cannot fully perform their functions. This occurs as a result of some disease when the kidneys stop fully filtering the blood. Substances that should be eliminated from the body end up back into the bloodstream. Impaired kidney function may be associated with a decrease in blood flow through them and a sharp decrease in oxygen supply.
The main function of the kidneys is excretory, that is, cleansing the body of waste and toxins, while the kidneys are responsible for maximum preservation of nutrients.
The kidneys take part in phosphorus-calcium metabolism and the formation of bone tissue by producing calcitriol (the active form of vitamin D), so in children, kidney failure negatively affects bone growth and abnormal development, and in adults it can cause fragility.
The kidneys regulate blood pressure, so kidney failure causes it to rise.
The kidneys are involved in the formation of red blood cells - erythrocytes. With kidney failure, the number of red blood cells decreases and anemia develops.
The kidneys regulate the amount of water and salts - maintaining the water-salt balance.
Causes of kidney failure
There are many reasons for the development of kidney failure. Some lead to a rapid deterioration of kidney function, most often of ischemic or toxic origin (acute kidney injury, or acute renal failure). Others lead to a gradual deterioration of kidney function (chronic kidney disease, or chronic renal failure). In addition to the inability of the kidney tissue to filter the body's metabolic waste products (particularly creatinine and urea nitrogen) from the blood, the kidneys' ability to control the amount and distribution of water in the body (fluid balance) and the level of electrolytes in the blood is reduced. Acute kidney injury is a sudden decline in kidney function over several days or weeks, causing a buildup of nitrogenous compounds in the blood (azotemia). Causes of renal failure in the acute form of the disease:
- acute disturbances of renal hemodynamics (collapse, shock);
- intoxications of various origins (medicinal, insect and snake bites, household poisons);
- acute infectious kidney damage;
- acute inflammatory kidney diseases (pyelonephritis, acute glomerulonephritis);
- injury to the kidney or other organ with large blood loss;
- urinary tract obstruction;
- kidney removal.
Among all the causes of chronic renal failure, a special place is occupied by diseases that affect the renal glomeruli:
- renal diseases - chronic pyelonephritis and glomerulonephritis;
- metabolic diseases: amyloidosis, gout, diabetes;
- congenital renal diseases: narrowing of the renal arteries, underdevelopment of the kidneys, polycystic disease;
- rheumatic diseases: hemorrhagic vasculitis, scleroderma, systemic lupus erythematosus;
- serious disorders of the cardiovascular system: arterial hypertension and diseases leading to significant changes in renal blood flow (heart failure, arrhythmia);
- diseases that cause problems with the outflow of urine.
Acute renal failure is always a consequence of other pathological processes in the body.
If you immediately pay attention to its symptoms and take action, it is possible to completely restore the function of the affected kidney. In chronic renal failure, the kidneys are damaged irreversibly. In some cases, kidney failure in women can develop during pregnancy.
Although decline in kidney function is possible at any age, chronic kidney failure and acute kidney injury are more common in older adults. Many diseases that cause deterioration of kidney function can be treated to restore kidney function. Thanks to the availability of dialysis and kidney transplantation, kidney failure has become a manageable disease rather than a fatal one.
Classification of the disease
The International Classification of Diseases (ICD) 10 has been amended to replace the outdated term “chronic renal failure” with the term “chronic kidney disease” (code N18).
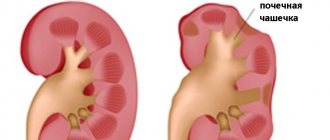
Modern classification is based on two indicators - glomerular filtration rate and signs of renal damage (proteinuria, albuminuria). Depending on their combination, there are five stages of chronic kidney disease.
The immediate causes of acute renal failure (code N17) are low blood flow velocity, acute destruction of the glomerulus with loss of afferent and efferent arteries and glomerular capillaries, damage to nephron tubules, or impaired outflow of urine from the kidney due to obstruction. Depending on this, there are three forms of acute renal failure:
- prerenal (70%),
- parenchymal (25%),
- obstructive (5%).
Symptoms of kidney failure
Kidney failure has the following main symptoms:
- decreased amount of urine excreted, urination disorder (oliguria, dysuria);
- swelling;
- general lethargy, drowsiness;
- nausea, vomiting, loss of appetite;
- tachycardia, increased blood pressure;
- bloating, loose stools.
Since in renal failure the kidneys do not perform their main - excretory - function, metabolism is disrupted.
Often the dominant symptoms of acute renal failure are manifestations of the underlying disease or symptoms caused by surgical complications of an operation that led to impaired renal function.
Chronic renal failure is characterized by an asymptomatic onset of the disease. At this stage, patients often do not complain; in extreme cases, they report increased fatigue with moderate physical activity, as well as dry mouth and weakness, which manifests itself in the late afternoon. Further attention is drawn to pale skin and flabby muscles that lose tone. Based on the results of a biochemical blood test, patients are often informed about the presence of protein in the urine and minor changes in the electrolyte composition of the blood.
The severity of symptoms depends on the stage of chronic kidney disease. The disease has an undulating course: the patient’s condition either improves or worsens again.
The terminal stage of chronic kidney disease is extremely dangerous, when the patient’s emotional reactions are disrupted (apathy sharply turns into excitement, night sleep is disturbed, and signs of lethargy appear). There is an ammonia odor from the mouth, swelling, the face becomes puffy, yellowish in color, traces of scratching are visible on the skin, the hair becomes dull, brittle, and dystrophy increases. Symptoms of uremic intoxication increase: ascites, pleurisy, pericarditis, uremic coma. Severe arterial hypertension often occurs.
Diagnosis of kidney failure
To diagnose renal failure, the following examinations are prescribed:
- general (clinical) blood test;
The mechanism of pathology formation
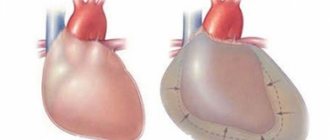
Chronic cardiovascular failure develops slowly due to the body's compensatory mechanisms.
At the compensatory stage of the myocardium, the heart muscle begins to hypertrophy. The vessels expand, causing their walls to become more fragile and permeable over time. Hormones are produced that change the composition of the blood, which becomes more liquid, its volume increases due to increased work of the bone marrow and an increase in the amount of water due to retention.
Compensatory possibilities dry up, and the decompensatory stage begins, which is characterized by a weakening of the functions of the entire cardiovascular system.
As the muscle mass of the myocardium grows, its small vessels lag behind in development, as a result, the heart muscle lacks oxygen and nutrients. Pathological changes occur: the proliferation of connective and sclerotic tissue. The heart becomes unable to pump the increasing volume of blood. Extensive oxygen starvation begins, which covers all organs.
Along with this, the walls of blood vessels become more fragile and permeable. Lymph leaks from the vessels. Swelling begins. These phenomena are especially dangerous in the lungs. They quickly fill with liquid and stretch. A person is tormented by a severe cough, and the discharge of sputum does not provide relief.
How to live with mitral regurgitation
At the initial stage, when there are no circulatory problems, the patient can simply lead a normal healthy lifestyle. Strong psycho-emotional shocks and heavy physical labor in unfavorable conditions are contraindicated for him. When the first signs of abnormality develop, we recommend:
- transition to easier work;
- for young people – learning a new profession;
- mental activity is not limited;
- service in the army is determined by a commission; most often the conscript is sent to the communications and radio engineering departments.
In case of edema, enlarged liver, ascites, severe shortness of breath and arrhythmia, a person must undergo a commission where he may be assigned a disability with the possibility of partial work or complete exemption from it. In this case, the conscript is considered unfit for service.
Causes of the disease
The causes of congestive heart failure are pathologies of the cardiovascular and endocrine systems. They can be congenital or acquired:
- genetic predisposition;
- ischemic disease.
- myocarditis
- diseases resulting in thickening of the walls of the myocardium and pericardium;
- thyroid diseases;
- diabetes.
Factors that provoke the occurrence of pathological processes include:
- bad habits, smoking and alcoholism;
- sedentary lifestyle;
- excessive body weight;
- severe infections (usually viral);
- heavy physical activity;
- frequent stress, improper daily routine, lack of sleep.
Congestive heart failure is more common in old age, occurring in 10% of people after sixty years of age. However, the disease also affects young people. In adolescence, it is necessary to carefully monitor the state of the cardiovascular system. The rapid growth of bone and muscle tissue, hormonal changes increase the load on the heart, which does not have time to grow with such rapid growth of the body as a whole.
Young athletes are at risk. Typically, training for teenagers is more gentle; children undergo annual examinations. If signs of congestive heart failure are detected, not only urgent treatment is necessary, but also a temporary refusal to exercise. Doctors recommend taking a break for about a year.
What is heart failure
There is an acute and chronic form of the disease. Acute is very dangerous because pulmonary edema and also cardiogenic shock can develop. Chronic causes hypoxia of various organs to develop over time. Heart failure kills many people every year and is considered one of the most common causes of death.
Once the pumping function of the heart is reduced in the case of heart failure, there is a difference between the body's need for blood supply and the fact that the heart cannot provide it. This difference is expressed in the fact that venous inflow increases. The resistance that the heart muscle must overcome in order to direct blood into the vascular bed increases.
Heart failure is not considered an independent disease. It is a consequence of various lesions of the heart and blood vessels. These include ischemia, arterial hypertension, valve defects, etc.
There are diseases, including, in particular, arterial hypertension, in which signs of heart failure in women and men increase gradually. This can happen over several years. In other diseases, for example, acute heart attack, in which some of the working cells die, this happens quite quickly. This period ranges from several days to several hours. If heart failure develops very quickly, its acute form is present; if it develops slowly, it is chronic.
What chronic heart failure is is known to 0.5-2 percent of all people from their own experience. After age 75, the incidence rises to 10 percent. The problem of prevention and treatment of this disease is very important, because the number of patients is constantly increasing. In addition, the disease often leads to disability and death.
Acute form
Along with chronic, there is an acute form of heart failure. The reasons for its occurrence are:
- myocardial infarction;
- major stroke;
- structural defects of the heart, congenital and acquired;
- hypertension.
A distinctive feature of acute cardiovascular failure is the suddenness of the attack and the absence of the listed stages of development. The person's condition quickly deteriorates and death is possible within a few minutes. The occurrence of pathology is indicated by a sharp deterioration in condition, suffocation, severe cough with foam or red sputum, blue discoloration of the skin, and cold sweat.
In such cases, first aid is to call an ambulance. Then the victim should be taken out into the open air, the collar and other tight clothing should be unbuttoned. The best pose is considered to be sitting, with legs down. A nitroglycerin tablet should be given under the tongue. Repeat the dose every 10 minutes until the ambulance arrives.
Important! In acute heart failure, you should not take a supine position.
Treatment
Aortic insufficiency is treated by a cardiologist and cardiovascular surgeon.
Drug treatment
Drug treatment is prescribed depending on the cause of aortic insufficiency. It is considered as an option in preparation for surgery or to reduce the symptoms of heart failure and alleviate the condition of patients who have contraindications to surgical treatment.
For rheumatism and infective endocarditis, a course of antibacterial therapy is prescribed. In the first case, penicillin antibiotics (benzathine benzylpenicillin) are used to prevent exacerbation of the disease. For infective endocarditis, amoxicillin, ceftriaxone, gentamicin, and, less commonly, vancomycin are usually prescribed for a long course of 2 weeks. Drugs are prescribed based on the clinic and the resistance of bacteria to them. Can be used as a single drug or in combination.
Treatment of arterial hypertension consists of prescribing ACE inhibitors (perindopril, enalapril, lisinopril) or sartans (valsartan, losartan) and dihydropyridine calcium antagonists (nifedipine, amlodipine).
Beta blockers (bisoprolol, metoprolol, nebivolol) are added to treatment in the case of reduced cardiac ejection fraction as determined by echocardiography.
Surgery
Aortic valve replacement is the only possible method of valve correction.
It is recommended for patients with:
- severe aortic regurgitation and the presence of symptoms regardless of ejection fraction;
- asymptomatic chronic severe aortic regurgitation and ejection fraction less than 50%;
- chronic aortic regurgitation in parallel with coronary artery bypass surgery or surgery on the aorta and other heart valves;
- asymptomatic severe aortic regurgitation with normal ejection fraction. on significant expansion of the left ventricle (EDV - more than 75 mm).
The duration of treatment for patients with aortic insufficiency varies greatly depending on the severity of the condition and the cause of the pathology. After the operation, it is recommended to undergo a course of rehabilitation in a cardiological sanatorium or rehabilitation center. The recovery period is at least 3 months, after which the patient can resume work with the doctor’s permission.
Age and gender factor
Statistical studies prove the connection between the spread of the disease and the gender and age of the patient.
In the age group up to 65 years, women suffer from congestive heart failure to a lesser extent; above this age, the rates become equal. Death as a result of acute heart failure is recorded in men after 45 years.
In old age, symptoms of congestive heart failure are more common, this is explained by chronic diseases, poor lifestyle, and reduced immunity.
Causes
The formation of a defect can occur in the prenatal period, in which case it is considered congenital. The causes of this pathology may be:
- alcoholism, drug use and maternal smoking during pregnancy;
- ionizing radiation;
- poisoning and taking certain drugs (antibiotics, non-steroidal anti-inflammatory drugs);
- systemic and infectious diseases.
The etiological factors of acquired deviation are usually:
- streptococcal and staphylococcal infections with the development of septic endocarditis;
- autoimmune diseases (lupus, multiple sclerosis);
- myocardial damage as a result of a heart attack;
- mitral valve prolapse;
- Marfan syndrome;
- chest injuries with rupture of the valves or fibers that hold them.
Relative mitral valve insufficiency is observed with pronounced enlargement of the left ventricle. The cause of this condition may be dilated cardiomyopathy, aortic valve disease, myocarditis and hypertension.
Diagnostics
Symptoms of congestive heart failure are observed by the therapist when examining the patient and listening to heart sounds. He refers the patient to a cardiologist. A number of studies are being carried out:
- ECG;
- ECHOCG
- HMEKG
- Radiography
- Coronary angiography
- MRI, MSCT
Research is being conducted on the characteristics of the heartbeat during physical activity. To do this, the patient is asked to perform a series of simple exercises, such as squats. After this, monitor the change and restoration of the pulse. More in-depth examinations of this kind are performed using a treadmill or exercise bike.
Surveys
Examination of a patient always begins with examining and listening to the heart. Already at this stage, the doctor is able to suspect a valve defect by the presence of a heart murmur. It is also possible to decrease diastolic (lower limit) blood pressure and, as a result, increase pulse pressure (the difference between the upper and lower limits of blood pressure). However, such signs of aortic insufficiency are detected only in chronic pathology, when the clinical picture of heart failure described above is already clearly manifested.
Instrumental methods are the only way to detect regurgitation on the aortic valve.
Echocardiography (ultrasound of the heart)
First line diagnostic method. It detects backflow of blood through the aortic valve. The doctor determines the degree of its severity and the possible cause - for example, trauma, vegetations on the valve (accumulations of bacteria on the valves - a sign of infective endocarditis), volumes of the left chambers of the heart, left ventricular ejection fraction and many other morpho-functional indicators.
Magnetic resonance imaging (MRI)
Used only if echocardiography is not available or visualization of the heart and its structures is extremely difficult.
Multislice computed tomography angiography and magnetic resonance imaging angiography (both contrast-enhanced procedures) are used in patients with a bicuspid aortic valve to evaluate the initial aorta to its arch, but only if echocardiographic findings are unsatisfactory.
X-ray of the chest organs
Used to assess the size of the heart and ascending aorta.
Electrocardiogram (ECG)
Allows you to identify rhythm disturbances, conduction disorders in the heart and signs of myocardial hypertrophy.
The methods listed are more than enough to make an accurate diagnosis of aortic insufficiency and begin treatment on time.
Symptoms
The most typical complaint is shortness of breath, which occurs with moderate and severe chronic mitral regurgitation and the clinic of acute left ventricular failure with acute mitral regurgitation. The presence of atrial fibrillation before surgery is an independent predictor of reduced long-term survival after mitral valve surgery for chronic mitral regurgitation.