SPECIALISTS Gynecologist Gynecologist-endocrinologist Pediatric gynecologist Mammologist-oncologist Dermatologist Hirudotherapist Intimate plastic surgery Doctor Contour plastic doctor Ultrasound doctor SERVICES AND PRICES Gynecology Mammology Ultrasound diagnostics Paid tests Intimate surgery Contour plastic Treatment for women PROMOTIONS AND DISCOUNTS Students Teams Friends and subscribers am For residents of the region For pensioners Promotions in clinic
Redness of the vagina, the desire to “scratch” between the legs, discomfort when urinating - these symptoms often occur in many girls of different age groups. When faced with these sensations for the first time in her life, a woman almost always experiences stress, since this is often associated with something indecent, usually with “bad diseases.”
No one will argue that this is an unpleasant specific sensation. It is difficult to meet women who have not encountered this unpleasant feeling at least once in their lives. Every year, about 10% of patients consult gynecologists whose leading complaint is burning and itching in the intimate area. In girls, vaginal itching can be due to physiological reasons, appear and disappear on its own before menstruation and do not require drug treatment. So, sometimes, to overcome unpleasant sensations in the genital area, it is enough to resort to simple rules of personal hygiene, change your diet, and give up tight underwear, especially synthetic ones.
Itching of the labia - causes
Itchy labia is usually caused by inflammation of the vagina (vaginitis) and vulva (vulvitis), called vulvovaginitis. The vulva is a woman's external reproductive organ, which includes the labia majora, labia minora, and clitoris.
If a disease that causes itching affects the internal genital organs, then the same symptom affects the external ones. In this case, peeling of the labia often occurs. The most common are atopic dermatitis, psoriasis and lichen planus.
Itching can occur when ingrown hairs appear after shaving.
Complications
To relieve intense discomfort, women often rub or scratch the itchy areas. Mechanical stress increases irritation, which leads to the formation of scratching, erosion, and ulceration. Infection of the mucous membrane aggravates the course of the underlying pathology due to the addition of vulvitis. In chronic somatic, endocrine and inflammatory genital diseases, dysplastic and neoplastic processes may occur against the background of prolonged irritation of the vulvar mucosa. Constant discomfort in the genital area causes the development of anxiety-depressive, hypochondriacal and other neurotic disorders.
Vulvoscopy
Vaginal infection
Genital irritant dermatitis (irritative dermatitis)
Irritant genital dermatitis is a genital rash that occurs after touching the sensitive skin of the genitals with certain chemicals. Some people will react with itching and a short-term rash, while others will develop long-term dermatitis.
Irritants can be any drugs applied to the skin of the genital organs. The most common are soap, other detergents and condoms.
Frequent irritants:
- soap and detergents;
- fabric softeners;
- hygiene products (for example, tampons, sanitary pads, wet wipes);
- baths, shower gel, oils, perfumes;
- toilet paper;
- condoms (latex);
- washing the genitals too often;
- wearing synthetic underwear.
The rash appears as redness on the vulva, which causes genital itching, discomfort and pain in women. After redness, blisters and scabs appear on the genitals, which are a potential site for the development of a genital infection.
Treatment of genital irritant dermatitis is based on recognizing the irritant and avoiding its use. To relieve symptoms, it is recommended to use corticosteroid cream and take cool baths.
Fungal infection of the vagina
A vaginal yeast infection is an inflammation of the vagina (vaginitis). It is characterized by irritation, redness, itching and white discharge. This infection is caused by the fungus Candida, and is therefore called candidiasis (popularly thrush).
Candida is commonly found in the vagina of some women and does not cause illness or symptoms because it is present in small quantities. If a woman takes antibiotics for a bacterial infection, they also kill the good bacteria in the vagina. Then there are more nutrients and places for candida to reproduce, and no one suppresses its vital activity. Due to an increase in the amount of fungus, inflammation occurs. That is why it is useful to use probiotics simultaneously with taking antibiotics to maintain normal vaginal microflora.
Although candidiasis can be transmitted sexually, it is not a classic sexually transmitted disease. Thrush can affect people who have never had sexual intercourse (genital fungus in girls).
A vaginal fungal infection can affect the vagina and vulva, a woman’s external genitalia – the labia majora and minora, the clitoris and the vestibule of the vagina. And inflammation of the labia occurs. Swollen labia and itching create noticeable discomfort.
Symptoms of a vaginal yeast infection are:
- vaginal itching;
- swelling and itching of the labia;
- burning sensation during urination and sexual intercourse;
- vaginal pain;
- cheesy white discharge without odor.
Treatment is carried out with antifungal drugs. The most commonly used vaginal products are: creams, tablets, suppositories, which are inserted into the vagina at night.
Over-the-counter genital fungus cream. It is recommended, for example, to use Canesten vaginal cream for external use.
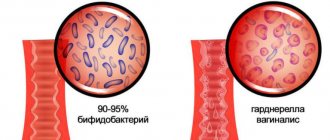
Bacterial vaginosis
Bacterial vaginosis is a condition that indicates an imbalance in the physiological microflora of the vagina. The vagina is usually home to bacteria that maintain an acidic pH and protect the mucous membrane - these are the so-called lactobacilli.
The bacterium that predominates in bacterial vaginosis is Gardnerella vaginalis. It is estimated that up to 50% of all vaginitis have this etiology.
Bacterial vaginosis is not a classic sexually transmitted disease, but it can be transmitted this way. This disease can also be present in women who are not sexually active.
Bacterial vaginosis can cause vulvovaginitis, an inflammation of the vulva and vagina.
The most common symptom is a grayish or milky discharge with an unpleasant odor. Inflammation of the labia manifests itself as itching and irritation of the external genitalia.
Treatment is carried out with metronidazole, a drug against anaerobic bacteria.
Chlamydia
Chlamydia is one of the most common sexually transmitted diseases, caused by the bacterium Chlamydia trachomatis. It is estimated that one in ten women aged 25 years is infected with chlamydia.
Chlamydia is transmitted through body secretions during vaginal, anal or oral sex. Transmission is also possible through infection of the fingers. Unprotected sex is one of the main risks of contracting any sexually transmitted disease.
Symptoms of chlamydia in women:
- painful sexual intercourse;
- burning or tingling when urinating;
- unusual vaginal discharge with an unpleasant odor;
- mild itching of the vulva, burning in the vaginal area, pain in the lower abdomen,
- light bleeding.
Treatment is with antibiotics, for example, a single dose of 1 g of azithromycin (Sumamed). Both sexual partners should be treated at the same time.
Genital herpes
Genital herpes is caused by herpes simplex virus type 1 and herpes simplex virus type 2.
Genital herpes is one of the most common sexually transmitted diseases today because the virus is highly contagious and is transmitted through all types of sexual contact (oral, vaginal, anal, and skin-to-skin contact).
Symptoms of genital herpes in women:
- a rash on the vulva that forms blisters; they burst and ulcers form on the labia, healing in about 15 days;
- itching of the external genitalia;
- pain;
- burning and tingling sensation;
- Possible fever, headache and other flu-like symptoms during primary infection.
Genital herpes is an incurable disease because the herpes simplex virus survives in the ganglia of the spinal cord after infection and can recur after some time.
Trichomoniasis
Trichomoniasis is a sexually transmitted disease caused by a microscopic single-celled animal from the protozoan subkingdom Trichomonas vaginalis. This parasite is the third most common cause of vaginitis - inflammation of the vagina.
Trichomoniasis can occur alone or in combination with other sexually transmitted diseases.
In many women and men, trichomoniasis is asymptomatic. But in women it can manifest as:
- vaginal discharge with an unpleasant odor, white, gray, yellow or green;
- itching of the external genitalia;
- burning and redness of the genitals;
- pain when urinating;
- painful sexual intercourse.
Trichomoniasis is treated with the drug metronidazole. It must also be taken by both sexual partners.
Condylomas acuminata
Genital warts are changes caused by infection with the human papillomavirus (HPV). There are many types of this virus, and some of them cause cervical cancer.
HPV is one of the most common sexually transmitted diseases, and it is estimated that more than 60% of sexually active people are infected with the virus. Not every infected person will develop genital warts, making the epidemic difficult to suppress. HPV is transmitted through vaginal, oral or anal sex.
Genital warts (bumps on the genitals of women) can be red, pink, brown or black depending on the patient's skin tone.
A growth at the vaginal opening (condyloma at the vaginal opening) can cause unpleasant itching of the external genitalia.
Treatment is carried out with antiviral drugs. HPV vaccination is available.
Prognosis and prevention
With adequate diagnosis and treatment, in most cases it is possible to completely get rid of vulvar itching or significantly reduce its manifestations. Longer treatment is required for atrophic diseases of the vulvar region, neoprocesses, and mental etiology of the disorder. For preventive purposes, timely treatment of extragenital and gynecological diseases, giving up bad habits, proper care of the genitals, and the use of soft cotton underwear are recommended. It is important to maintain a sleep and rest schedule, eat rationally, and avoid significant psycho-emotional stress and exposure to harmful environmental factors.
4.Treatment
Itching in the perineum is not a disease, but only a symptom, and most often not the only one. Accordingly, desensitizing (reducing the sensitivity of skin receptors), anti-inflammatory, analgesic drugs have an auxiliary value and are prescribed symptomatically. The main goal is to find and eliminate the underlying disease, its causes and risk factors. Based on the diagnostic results, a course of etiopathogenetic therapy is prescribed: antiparasitic, antibiotic and/or antimycotic, in some cases psychotherapeutic, hormonal, proctological, etc. If a reliable cause-and-effect relationship is identified between itching in the perineum and the mechanical, chemical, and allergic factors described above, a full therapeutic effect is possible only if contact with such irritants (irritants) is excluded.
Pimples and irritation after shaving in the intimate area in women: how to properly remove hair with a razor?
Hair removal in intimate areas is a recent trend. How to avoid irritation after depilation?
- Be sure to apply shaving cream or foam to your skin before depilation.
- If you are removing hair with a reusable machine, treat it with a disinfectant such as alcohol or chlorhexidine.
- Use only a very sharp razor; a dull razor can damage delicate skin.
- Do not press the razor too tightly against the skin or run over one area several times in a row.
- After depilation, treat the skin with a septic cream and do not wear underwear until it dries to allow the area to calm down and not cause irritation.
1.General information
Itching is an extremely unpleasant skin reaction; if it “itches”, it is impossible to concentrate on something else, it is impossible to be distracted, to hide, to work, to take a forced position, to wait, to sleep. Only with the utmost effort of will can you restrain the persistent movement of your fingers in the direction of the itchy area, and sometimes this fails, and then the “combed” area itches even more, and you have to again...
The problem is greatly aggravated if the skin itches - and itches unbearably - in a place that cannot be declassified under any circumstances in the presence of other people. For example, in the perineum. And all that remains is to feign deep attention to the words of the interlocutor, but in reality make imperceptible movements on the chair, or shift from foot to foot, or sneak a glance at the watch: this torture must someday end.
Itching in the perineum, in principle, cannot be “normal,” “common,” or unimportant. This is a desperate attempt by the body to attract attention to the problem. Whatever the reasons (and there is no such thing as causeless itching), they are always pathological and always require a response, and the most appropriate response in this case is to see a doctor.
A must read! Help with treatment and hospitalization!
Cream or soap: how to properly care for the skin in intimate places?
- Use only special cosmetics for delicate intimate care. It contains natural ingredients, does not cause allergic reactions and is suitable for gentle cleansing of delicate areas. The composition of GINOCOMFORT washing gels corresponds to modern recommendations of gynecologists - GINOCOMFORT intimate cosmetics are not only suitable for daily care, but also help to maintain the cleanliness of the genitals during menstruation and during the treatment of gynecological diseases, when the body is especially vulnerable.
- If possible, wear comfortable underwear made from natural fabrics. If you want to wear erotic panties, be sure to take a shower before putting on such panties, and also change your underwear before going to bed - sleeping in thongs can increase the level of pathogenic bacteria in the vagina.
- Maintain personal hygiene: obstetricians-gynecologists recommend washing yourself 1-2 times a day, during menstruation up to 4 times a day, if possible, with each pad change.
Pads and tampons should be changed every 3-4 hours, regardless of the amount of discharge. - Pay attention to contraception: if you are allergic to latex, choose condoms made from other materials.
- Visit your obstetrician-gynecologist at least 2 times a year to rule out the development of diseases.
And remember: irritation in the intimate area, even if it just “itches” and there are no other more serious symptoms, is not the norm, and this condition is most often easy to eliminate.
There is no need to avoid the possibility of solving an unpleasant problem. The right cosmetics and treatment selected by an obstetrician-gynecologist will allow you to regain confidence in your beauty, comfort, feeling of freshness and good mood every day. Sources:
- Inflammatory diseases of the female genital organs. Modern perinatal technologies in strengthening the reproductive health of patients. Naumov I.A. // Monograph. Saarbrucken: LAP LAMBERT Academic Publishing GmbH end Co. KG. — 2011. — pp. 18–21.
- Microbiological characteristics of biotopes of the reproductive tract with endometritis. Glukhova E.V., Shakhovskaya I.N. // Togliatti honey. consultation – 2008. – 1 (2): pp. 38–44.
- Medical and social characteristics and forecasting of reproductive health of young women at the present stage. Torubarov S.F. // Social aspects of public health. – 2013. – 5 (33): P. 7.
- https://ciplamed.com/content/important-tips-to-maintain-intimate-hygiene
- https://www.lactacyd.eu/your-intimate-zone/
- https://www.medicalnewstoday.com/articles/321537.php