An acute inflammatory process, which, usually starting from the labia minora or majora, gradually spreads to the clitoris and vagina, is called vulvitis in medical practice. This pathological condition is accompanied by acute symptoms, which can manifest in the fair sex, regardless of age.
Vulvitis requires immediate consultation with a specialist, as it can lead to adhesions in the mucous membranes of the external genitalia, which subsequently causes serious problems in the intimate area, and in the case of the disease in young women, becomes a cause of infertility.
Causes of inflammation of the clitoris and labia
The content of the article
Most often, the pathology is of an infectious-inflammatory nature. Depending on the cause of the development of vulvitis, there are two main forms of the disease.
- Primary vulvitis. This inflammation is somewhat less common than secondary inflammation, and usually affects either patients of a younger age category or women in the postmenopausal period. The cause of the development of primary inflammation of the labia and clitoris is the following factors: failure to comply with the rules of personal hygiene, too tight synthetic underwear, allergic reactions to shower gel or other hygiene products, mechanical damage to the external genitalia and hormonal imbalances. Little girls may experience similar inflammation if they have helminthiasis - infestation with worms.
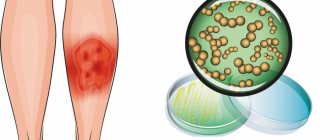
- Secondary vulvitis . The most common form of inflammatory processes of the clitoris and labia resulting from infectious infection. Nonspecific pathogens of vulvitis include all representatives of opportunistic flora, which are normally natural inhabitants of female microflora - Escherichia coli, staphylococci, streptococci, yeasts, etc. Specific infections include sexually transmitted infections. Secondary vulvitis occurs more often in young patients of childbearing age, as they are sexually active.
Symptoms of vulvitis in women
How to detect the development of the disease in the early stages? It is enough just to be attentive to your health and not to neglect the obvious signs of pathology. The most characteristic symptoms of vulvitis in girls include the following local manifestations:
- Itching and burning are the main diagnostic signs of vulvitis in women. The patient experiences very severe discomfort, especially when the inflamed surface comes into contact with the fabric of the underwear. Also, burning and itching intensify and transform into pain during physical exercise, during sexual intercourse and after genital hygiene.
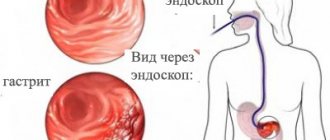
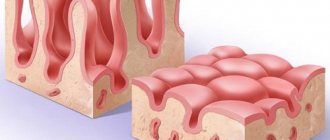
- Swelling and redness are easily detected by the naked eye. The patient notices hyperemia of the tissues of the labia, clitoris and vaginal vestibule, which is especially pronounced in the area of delicate mucous membranes.
- The roughness of the surface of the labia minora is a consequence of the enlargement of the sebaceous glands, which protrude above the smooth surface of the mucous membrane.
- Specific discharge - may have a different appearance and consistency. Most often, clear, watery leucorrhoea is observed, which does not have an unpleasant odor. However, some infectious pathogens cause putrefactive, purulent, curdled and even bloody discharge, which requires immediate contact with a gynecologist.
- The appearance of small ulcers and uncharacteristic plaque - these signs are not detected in all forms of vulvitis, but they allow a fairly accurate diagnosis to be made for herpetic, candidiasis and diphtheria forms of the disease.
- Changes in general condition include weakness and increased body temperature, acting as rare symptoms of vulvitis.
It is almost impossible not to notice the development of pulpitis, since even the less pronounced, from the point of view of symptoms, chronic form of the disease is characterized by causing severe discomfort to the patient. Acute vulvitis in women can deprive the patient of sleep and ability to work.
Symptoms of inflammation of the clitoris and labia
The symptoms of the pathological process are vivid, so it is impossible not to notice it, and includes the following signs:
- itching, burning and soreness of the affected area;
- tissue swelling;
- hyperemia (change in color) of the skin;
- development of small ulcerative lesions;
- discomfort during sexual intercourse.
All of the above symptoms usually intensify during urination and during intensive walking. Lack of rational and timely treatment can lead to the spread of an infectious and inflammatory process to the tissue of the inner thighs and vagina.
Diagnostic procedures
The vulva is examined during a pelvic examination. A gynecologist performs vaginal examinations. A transvaginal ultrasound is prescribed. If necessary, vulvoscopy and colposcopy. A bacterial smear is examined to exclude infectious diseases. Clarification of the nature of the neoplasm using histological examination. For biological analysis, scrapings and punctures of tumors are taken.
Removing the tumor often causes a new growth to appear. Removing papillomas requires long-term treatment. Surgeries and the postoperative period may occur with complications. Hematomas may form, the urinary system may be disrupted, and severe bleeding may occur.
Diagnosis and treatment of inflammation of the external genitalia
The diagnosis can only be made by a gynecologist. At the same time, no special diagnostics are needed at the first stage. The doctor will immediately notice inflammation during a routine gynecological examination. Next, the doctor determines the cause of the inflammation, after which a treatment regimen is selected.
Depending on the cause of the development of the pathology - an allergic factor, injury, incorrectly selected underwear - it is enough to simply limit the direct contact of the provoking agent with the organs and apply symptomatic therapy (local treatment that relieves unpleasant symptoms). You can easily identify this cause by donating blood for allergies. The analysis will show the cause due to the presence in the blood of special antibodies that are formed only during allergic reactions.
When diagnosing the infectious nature of the disease, microbiological culture is carried out on nutrient media in order to identify the causative agent and the correct selection of antibiotic therapy. To do this, the gynecologist takes swabs from the genital tract and sends them to the laboratory.
There, they first determine the type of infection, and then test different drugs on the samples. Since almost all pathogens of sexual diseases easily adapt to medications, choosing pills that will help you completely recover is not easy. Sometimes specialists go through up to a dozen different medications.
Unfortunately, inflammation is rarely caused by a single pathogen; more often, the cause is a whole bunch of infections, starting with thrush and ending with gonorrhea. In such cases, it will not be enough to simply take smears - the examination will continue further. You will have to donate blood for syphilis, hepatitis and undergo a pelvic ultrasound, as the process quickly spreads through the genital tract, affecting internal organs.
Leading specialists in the treatment of inflammatory diseases of the genitals in the Southern Federal District
Ermolaeva Elvira Kadirovna is a well-known and recognized specialist in the North Caucasus in the diagnosis and treatment of inflammatory diseases of the genitals. She is a gynecologist, ultrasound doctor, physiotherapist-resortologist. Elvira Kadirovna is approached by women who want to improve the aesthetics of the genital organs, reduce the size of the vagina and refresh intimate relationships from all regions Russia and foreign countries.
Ermolaev Oleg Yurievich Candidate of Medical Sciences, gynecologist-endocrinologist with 25 years of successful experience in the treatment of inflammatory diseases of the genitals. Able to see relationships that elude others.
Shchepkin Petr Sergeevich Gynecologist, specialist in the diagnosis and treatment of inflammation of the genital organs. Experienced ultrasound doctor.
About the doctors of the Clinic in detail...
| INTERNATIONAL RECOGNITION of the reputation and achievements of the Women's Health Resort Clinic in the development and implementation of effective and safe treatment methods and the quality of medical services provided is the AWARDING of the Women's Health Resort Clinic in Pyatigorsk with the SIQS International QUALITY CERTIFICATE in the field of medicine and healthcare. International Socratic Committee, Oxford, UK and Swiss Institute for Quality Standards, Zurich, SWITZERLAND. |
The resort clinic for women's health operates both for paid services and in the voluntary health insurance system.
We work seven days a week and on holidays:
Monday - Friday from 8.00 to 20.00, Saturday, Sunday, holidays from 8.00 to 17.00.
Treatment of inflammation of the genital organs by appointment by multi-channel telephone 8 (800) 500-52-74 (toll-free within Russia), or +7.
| ONLINE information about the treatment of inflammation of the genital organs can be found at: REGISTER ONLINE for the treatment of inflammatory diseases of the genitals here. REGISTER online for treatment of inflammatory diseases of the genitals here. Buy coursework by phone +7 (928) 022-05-32 or here. |
Make an appointment with a gynecologist
With respect for the religion and different habits of our Patients, we achieve high efficiency and comfort of treatment.
We are at your FULL DISPOSAL if you have any doubts or wishes.
- Reviews about the treatment of inflammatory and infectious diseases of the pelvis in our Clinic
- About the Clinic
- Why choose us?
- Clinic team
- Cost of visiting a gynecologist for the purpose of “Checking for EVERYTHING”
Diagnostics
Cancer is diagnosed using a biopsy. High accuracy of the study helps to distinguish a malignant tumor from a benign one. A gynecologist examines a woman using a colposcope. The skin is treated with a special solution, which makes the lesions appear more pronounced. If the tumor spreads beyond the vulva, perform the following steps:
- Research of the genitourinary system and rectum.
- Detection of tumor growth and penetration into lymph nodes and organs using CT or MRI.
- Search for metastases using radiography.
Prevention
In order to prevent the development of vulvitis, you must adhere to the following rules:
- Be sure to practice preventive examinations with a gynecologist twice a year.
- Maintain personal hygiene carefully.
- Treat all infectious diseases of the genitourinary system in a timely manner, do not ignore even minor symptoms.
- Avoid hypothermia.
- Conduct periodic examinations for helminthiasis .
- Avoid casual sex and use barrier contraception.
- Wear high-quality underwear made from natural materials.
During pregnancy
Vulvitis can occur at any stage of pregnancy, since during this period a woman is more susceptible to infections and exacerbation of chronic diseases. In addition, during the period of bearing a child, the immune defense weakens, which also contributes to the proliferation of pathogens.
Treatment of vulvitis in a pregnant woman should be carried out under the supervision of a doctor after all the necessary tests have been carried out. The doctor prescribes safe medications, mainly for topical use. It is also important to take measures to boost your immunity . Antibacterial and antifungal agents are prescribed only when absolutely necessary.
The expectant mother should understand that if vulvitis remains untreated during pregnancy, this risks infecting the child during childbirth.
Types of surgery
Based on the characteristics of the tumor, its treatment is prescribed. Surgical interventions to eliminate this disease:
- Cryodisruption. Nitrogen exposure is carried out. Freezing tissue stops cell development. During the operation, low-temperature liquid nitrogen is applied to the condyloma. The operation is performed without anesthetic. Not painful. The operation was well tolerated. Removing tumors with liquid nitrogen is a special technology; not every clinic performs these manipulations. The operation has minimal complications. There may be a small scar or burn.
- Radio wave excision. A directed flow of low frequencies dissects the tumor. Radio wave is the most gentle method in relation to neighboring tissues. There is no pain. There is no risk of scarring, bleeding, suppuration, or necrosis. Healing occurs in the shortest possible time.
- Laser. A directed laser evaporates the tufted growths. Laser ablation is used to excise resistant condylomas. The skin is not injured, and under the influence of the laser, epithelial cells grow. The depth of laser exposure is controlled. Does not leave scars. No contact with tissue occurs.
- Electrical coagulation. Electric current is used to cauterize the damaged area. The removed material is sent for histological analysis. The process has a number of contraindications. For example, herpes, oncology, hemostasis, inflammation of neoplasms. There are cases of relapse. There may be a small scar on the surface of the vulva.
- Chemical exposure. The destruction method involves applying a special drug to the affected area. A special composition with organic and inorganic acids, nitrates causes burning and death of condyloma cells. It is not accompanied by pain and is used without anesthesia.
- Plasma coagulation. An arc discharge containing gas penetrates the tissue and vaporizes areas with growths. Cauterizes blood vessels. The method has a high level of efficiency. Thermal damage to tissue occurs at a minimum depth, which promotes rapid healing. No scars are formed and pain is minimal.
Pathogenesis
Bacterial vulvitis develops after infection with staphylococci, E. coli, and streptococci. Candidiasis vulvitis is caused by exposure to Candida fungi. The disease manifests itself against the background of a decrease in the body’s immune reactivity.
Its development is caused by an excess of the total amount of opportunistic or pathogenic microflora in the vagina. This leads to the progression of the inflammatory process in the vaginal mucosa. In more rare cases, vulvitis is of viral origin and is caused by herpes , adenoviruses , etc.
The inflammatory process can also occur against the background of an allergic reaction. Due to the anatomical features of the skin in girls, sensitivity to fungal and bacterial pathogens increases.
Consequences and complications
If the disease is not treated promptly, it can become chronic. Complications may be as follows:
- ulcers on the genitals;
- vulvovaginitis;
- cervicitis, endometritis ;
- candidiasis;
- urethritis , cystitis ;
- formation of scarring, condylomas .
If the disease is not treated and, accordingly, complications develop, a kind of “vicious circle” can be observed when complications, in turn, will provoke the re-development of vulvitis .
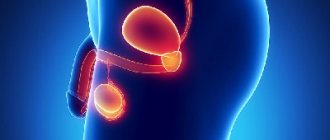
Treatment of bartholinitis
Treatment of bartholinitis must begin at the first symptoms (signs) of trouble.
If you consult a doctor early, based on our experience, there is a real chance to stop the inflammatory process and prevent the formation of an abscess or cyst of the Bartholin gland.
Treatment of bartholinitis in the acute stage consists of quickly limiting and stopping the inflammatory process.
Treatment of bartholinitis with delayed treatment is to accelerate the maturation of the pseudoabscess and shorten the period of physical and moral disability.
At the same time, there remains a chance (small chance) of stopping the process without surgical treatment.
To treat bartholinitis, the Women's Health Resort Clinic uses a combination of herbal remedies and modern physiotherapy.
Physiotherapy potentiates (manifold enhances) the effect of herbal medicines.
In combination with herbal medicines, physiotherapy allows you to achieve recovery WITHOUT ANTIBIOTICS.
All physiotherapeutic procedures at the Women's Health Resort Clinic are performed WITHOUT PAIN in comfortable conditions by professionally trained midwives.
Contraindications to physiotherapeutic treatment are general contraindications to physiotherapy: stage 3 hypertension, oncological processes in the body, severe somatic (therapeutic) diseases in the stage of decompensation.
Contraindications for each specific procedure are described in detail on the website in the corresponding paragraph of the article “Physiotherapy”.
Medicines based on herbal and mineral raw materials according to the prescriptions of the Clinic’s doctors have detoxifying, analgesic and local (local) anti-inflammatory effects, forcing the immune system to actively fight the infectious process.
Our experience in the treatment of bartholinitis shows that the use of medicines based on natural raw materials is an important physiological (corresponding to human physiology) component of treatment.
In case of suppuration of the Bartholin gland - filling the gland with pus with the formation of a pseudo-abscess of the Bartholin gland - it is necessary to open the Bartholin gland.
The opening of the Bartholin gland in our Clinic is performed WITHOUT PAIN using a non-contact method using the Surgitron apparatus.
In some cases, up to 25 ml of pus leaks out.
The internal pressure is so great that when a pseudoabscess of the Bartholin gland is opened, a stream of pus sometimes reaches one meter.
The cost of opening the Bartholin gland WITHOUT PAIN is 4250 rubles.
| Photo of bartholinitis. Suppuration (pseudoabcess) of the right Bartholin gland |
| Photo of bartholinitis. After non-contact opening and drainage of a pseudoabcess of the right Bartholin gland in our Clinic |
Within 5-7 days, professionally trained midwives of the Clinic CLEAR the remaining pus and WASH the Bartholin gland, perform magnetic laser and ultrasound treatment.
After non-contact opening of the Bartholin gland, the wound is epithelialized (heals) with the formation of an aesthetic, thin, barely noticeable scar.
Hospitalization (inpatient treatment) is not required.
During the treatment of bartholinitis, a fortified diet is necessary. There are no restrictions or dietary requirements.
Sexual intimacy is possible after complete relief (cure) of acute bartholinitis or complete epithelization (healing) of a postoperative wound.
Complete healing, as a rule, occurs 9-12 days after non-contact opening of the Bartholin gland in our Clinic.
During the period of an open wound and incomplete healing, if it is impossible to avoid sexual intercourse, surrogate forms of love and anal sex are allowed.
In case of recurrent (recurring) bartholinitis, the Women's Health Resort Clinic performs extirpation (husking, complete removal) of the Bartholin gland or marsupalization of the Bartholin gland.
After extirpation (husking) of the Bartholin gland, Bartholin gland pseudoabscess and Bartholin gland cyst never occur again.
We accept girls, young women and women from all cities of Russia, near and far abroad.
The resort clinic for women's health operates both for paid services and in the voluntary health insurance system.
The spa clinic for women's health facilitates the accommodation and accommodation of women, women with children and couples during examination and treatment.
About living conditions and transfer from Mineralnye Vody airport and Pyatigorsk railway station in detail in the article “Accommodation”.
If you need to book accommodation, please coordinate your arrival date no later than 7 days in advance.
Reception only by appointment no later than 3 days in advance by phone 8 (800) 500-52-74 (free call within Russia) or +7 (928) 022-05-32.
Diet
Diet for candidiasis
- Efficacy: therapeutic effect after 10 days
- Terms: 3 months or more
- Cost of products: 1400-1500 rubles per week
Hypoallergenic diet
- Efficacy: therapeutic effect after 21-40 days
- Timing: constantly
- Cost of products: 1300-1400 rubles. in Week
If you have vulvitis, your diet should include the following foods:
- Fermented milk products - fermented baked milk, kefir, milk, sour cream, whey, natural yogurt.
- To compensate for the deficiency of vitamins E and A - broccoli, viburnum, spinach, seaweed, dried apricots, prunes.
- To replenish the lack of vitamin C - currants, strawberries, wild strawberries, sea buckthorn, apples.
- Sources of vitamin B are nuts, legumes, liver, mushrooms, cheese.
- Sources of zinc are buckwheat, peas, nuts, turkey, beef.
- Sources of calcium are dairy products, barley porridge.
- The diet for vulvitis should not include fatty, sweet, spicy, salty foods.
The following should be excluded from the menu:
- Smoked meats.
- Pickles.
- Alcohol.
- Ketchups, mayonnaise.
- Canned food.
- Yeast baked goods.
For allergic vulvitis, a hypoallergenic diet is prescribed, which excludes all foods that cause allergic reactions.