Nephrosclerosis
(
nephrosclerosis
; Greek nephros kidney + sclerosis) - replacement of the kidney parenchyma with connective tissue, leading to their compaction, wrinkling and dysfunction.
“Nephrosclerosis” is a clinical and anatomical concept. The process can develop as a result of various diseases of the kidneys and their blood vessels. In 1872, Gull and Sutton (WW Gull, HG Sutton) first suggested that the cause of N. is damage to the vessels of the kidneys, and called it arteriolocapillary fibrosis. In 1914, Volhard and Far (F. Volhard, Th. Fahr) identified arteriolosclerotic changes in the kidneys as an independent nosological form of diffuse bilateral kidney disease and associated them with hypertension; They also proposed to distinguish between simple renal sclerosis - in a benign form of hypertension and its combined form - in hypertension with a malignant course.
General information about what nephrosclerosis is
The kidney is a paired organ responsible for filtering and removing excess fluid and waste from the body. blood clots are dissolved .
Nephrosclerosis is a chronic disease characterized by the replacement of renal tissue (parenchyma) with connective tissue that is unable to perform all basic functions.
With nephrosclerosis, the walls of arterioles and arteries thicken, which negatively affects the blood supply to the kidneys. With prolonged lack of nutrition, the death of the tubules and glomeruli begins, which are responsible for the formation of urine, which leads to the formation of renal failure .
The outcome of the disease can be very different and directly depends on how timely the diagnosis was made and how timely and correctly the treatment was started. With active therapy in the early stages, recovery occurs. In advanced cases, deaths occur. A synonym for nephrosclerosis is a wrinkled kidney .
Mechanism of development of kidney nephrosclerosis
| GreenFlames09 Flickr |
Nephrosclerosis is not an independent disease and, as a rule, it is provoked by other pathologies.
But, despite the cause of development, nephrosclerosis has a common pathogenesis. Under the influence of provoking factors, destruction of the renal epithelium occurs with damage to some nephrons. Since the cells of the organ are not able to regenerate, the damaged areas are replaced by connective fibers, and a gradual compaction of the organ occurs.
In unaffected areas, filtration and blood circulation increase, as a result of which the volume of urine excreted increases, but its density decreases. Due to disruption of blood flow that regulates glomerular filtration, arterial hypertension develops or worsens.
Pathogenesis
Long-term exposure to negative factors leads to persistent vasospasm and impaired trophism. This leads to irritation of histocytic elements, and as a consequence, to local or diffuse proliferation of connective tissue, which cannot perform the functions of the renal system.
The affected buds first become denser, and then shrink and decrease in volume. As the connective tissue grows, it compresses the tubules and glomeruli, causing their atrophy. Part of the glomerular apparatus leaves the systemic circulation, and capillaries in the affected areas cease to function. As a result of impaired blood flow, the formation and release of angiotensin and renin into the blood increases, which leads first to hypertension , and then to hypertrophy of the heart chambers . As the process progresses, the death of tubules and glomeruli is noted.
Causes
Nephrosclerosis is a complication of diseases such as arterial hypertension , glomerulonephritis , diabetes mellitus , gradually leading to the development of chronic kidney disease.
It is customary to highlight:
- primary (hypertensive) nephrosclerosis;
- secondary nephrosclerosis.
The primary form (primarily wrinkled kidney) develops against the background of a pathology that is not related to the functioning of the renal system, but disrupts normal blood circulation in the kidney. A primary wrinkled kidney can be caused by:
- hypertonic disease;
- thrombosis;
- atherosclerosis.
Types of primary nephrosclerosis
- Atherosclerotic nephrosclerosis . When atherosclerotic plaques form on the walls of renal vessels, blood flow decreases, which leads to the death of renal tissue. The characteristic localization of atherosclerotic plaques is the branching of the renal artery. This type of nephrosclerosis is considered the safest compared to others, because it is characterized by only partial kidney damage. The left kidney is most often affected; bilateral nephrosclerosis .
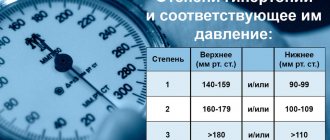
- Hypertensive nephrosclerosis . With constantly elevated blood pressure , blood vessels lose their elasticity and there is a tendency to spasm. With insufficient oxygen and nutrition, cell death occurs. Types of hypertensive nephrosclerosis: arteriolonecrotic - observed in malignant hypertension and leads to the death of capillaries and arterioles; arterilosclerotic – there is an excessive proliferation of connective tissue on the vascular wall.
- Involutive nephrosclerosis . Changes are formed as a result of involutional, age-related changes upon reaching a certain age. After 45-50 years, more calcium is deposited on the walls of veins and arteries, the number of muscle fibers increases, which negatively affects blood circulation. The cause of the pathology may be atrophy of the elements of the urinary tubules, which also manifests itself with age.
- Diabetic nephrosclerosis . A complication of diabetes mellitus is necrotization of the kidney tissue, which prevents the organ from fully functioning and doing its job. Patients note swelling and increased blood pressure. Deviations in the general blood test are recorded.
- Infarction nephrosclerosis . It is formed as a result of blockage of the renal artery by an embolus or thrombus, which causes necrosis of the feeding area of the renal tissue.
- Venous nephrosclerosis . With venous congestion of the kidneys, blood flow becomes difficult, venous stagnation is formed, which creates optimal conditions for an increase in the number of tropocollagen molecules.
Secondary nephrosclerosis (secondary wrinkled kidney) is formed as a result of the progression of pathology of the renal system.
Diseases that provoke the development of a secondary wrinkled kidney:
- Glomerulonephritis . In inflammatory diseases of the throat (pharyngitis, sore throat , laryngitis ), hyaline is deposited on the vessels of the kidneys, impairing their elasticity.
- Nephritis , pyelitis , pyelonephritis . Inflammatory disease of the kidney tissue or parts of the kidney. Infectious agents penetrate the tubules and glomeruli, affecting the parenchyma and forming blood clots.
- Systemic lupus erythematosus . A disease in which the body produces antibodies against its own organs and systems, damaging the structure and disrupting their functioning.
- Nephropathy of pregnancy. A specific change in hormonal levels leads to instability of blood pressure, vasospasm, and fluid retention in the body.
- Nephrolithiasis. Concretions and stones are most often found in the right kidney.
- Tuberculosis . The tuberculosis bacillus, circulating throughout the body, affects the renal system.
- Diabetes . High sugar levels in uncontrolled diabetes negatively affect the condition of the vascular wall.
- Traumatic injury to renal tissue . Blockage of blood vessels occurs as a result of the detachment of particles of parenchyma, which negatively affects the blood circulation of the organ and leads to the death of nephrons and tubules.
- Ionizing radiation . It negatively affects the functioning of the entire body, including the renal system.
Pathological anatomy
Rice.
3. Microscopic specimens of the kidney in a malignant form of nephrosclerosis: a - in the center the renal glomerulus is visible with fibrinoid necrosis of the afferent vessel (1) and glomerular blood capillaries (2); hematoxylin-eosin staining; x 310; b— glomerulus with severe sclerosis of the loops of blood capillaries and a decrease in the number of endothelial cells; hematoxylin-eosin staining; x 525. Fig. 4. Macroscopic specimen of a kidney in a malignant form of nephrosclerosis: on the left - general view (the kidney capsule has been removed, the surface of the kidney is uneven, fine-grained, mottled due to numerous hemorrhages); on the right is a sagittal section of the kidney (the pattern of the structure is disturbed, numerous hemorrhages of various sizes are visible). Of the primary nephrosclerosis, the most common is hypertensive, or arteriolosclerotic, nephrosclerosis. Far (Th. Fahr), depending on the nature, prevalence, degree of plasmorrhagia (see) and hyalinosis (see), and the exclusion of new groups of nephrons, renal failure develops (see).
The malignant form is characterized by fibrinoid necrosis of arterioles (arteriolonecrosis) and capillary loops of the glomeruli (Fig. 3, a), stromal edema, hemorrhages, protein degeneration of the tubular epithelium. Renal sclerosis develops very quickly in response to necrotic changes (Fig. 3, b). Similar changes can occur with eclampsia (malignant post-eclamptic nephrosclerosis).
Macroscopically, the surface of the buds is mottled and fine-grained (Fig. 4); the kidneys are not much different from the “large motley kidney” with glomerulonephritis (see). Renal arteriolonecrosis leads to renal failure.
According to M. Lohlein, the benign form of arteriolosclerotic N. corresponds to the first stage of N. (initial N.), which occurs clinically without manifestations from the kidneys, and the malignant form corresponds to the second stage of N. (progressive N.), for which characterized by a rapid course with the development of renal failure.
However, this sequence of the process is not recognized by everyone.
According to N. N. Anichkov, K. G. Volkova, M. A. Zakharyevskaya, the morphology of arteriolosclerotic nephrosclerosis reflects the features of the course of hypertension.
Atherosclerotic N. occurs when there is a narrowing (caused by an atherosclerotic plaque) of the renal artery at the site of its origin or division into first- and second-order branches.
More often this process is one-sided, less often two-sided. In the kidney, wedge-shaped areas of parenchymal atrophy develop with collapse of the stroma and replacement of these areas with connective tissue or infarctions with their subsequent organization and scar formation (atherosclerotic wrinkled kidney, atherosclerotic nephrocirrhosis). Macroscopically, the kidney becomes coarsely tuberous, and it is often difficult to distinguish it from a kidney in case of infarction. The function of such a kidney (kidneys) suffers little, since most of its parenchyma remains intact. As a result of ischemia of the renal tissue, in some cases with stenotic atherosclerosis of the renal arteries, symptomatic (renal) hypertension develops.
Secondary N., which most often develops with chronic glomerulonephritis, is associated not only with glomerulonephritis as such (fibroplastic transformation of glomerular changes), but also with those changes in the vessels of the kidneys, which constantly occur in this disease, reflecting the state of renal allergy (proliferative endarteritis ), arterial hypertension (arteriolosclerosis, arteriolonecrosis), adaptation of the vascular system to the shutdown of the “peripheral bed” of the kidneys (progressive elastofibrosis of the arteries with secondary lipoidosis). Thus, secondary N. always has features of angiogenic.
Therefore, the morphological criteria for the differential diagnosis of primary (hypertensive) and secondary (nephritic) renal shrinkage are usually unclear.
Involutive changes in the kidneys are detected starting from 40-50 years of age and by 70 years of age lead to a reduction in the mass of active nephrons by approximately 40%.
Age-related renal atrophy is accompanied by a gradual thinning of the cortical layer of both kidneys, atrophy of the tubular epithelium until death and replacement of the tubules with scar tissue. The glomeruli undergo hyalinosis, and their number gradually decreases. Vascular resistance, which increases with age, leads to emptying of the glomerular capillaries and the formation of anastomoses between the afferent and efferent arteries, bypassing the glomeruli.
Nephrosclerosis in old age is associated primarily with age-related changes in the vessels of the kidneys, so it approaches the primary mechanism of development.
Main clinical signs. Wedge, manifestations of primary N. usually occur in the late stages of hypertension, both in its benign and malignant course. One of the early signs of kidney damage may be polyuria (see) and nocturia (see), however, nocturia is not always a consequence of polyuria and may indicate a disturbance in the circadian rhythm of the kidneys. Proteinuria (see), observed with N., is usually small and inconsistent.
Microhematuria is often observed with N., in some cases there may be macrohematuria (see Hematuria). A decrease in renal clearance (see) with a relative increase in the filtration fraction is manifested by a decrease in the concentrating ability of the kidneys (hyposthenuria), which is detected using the Zimnitsky test. Accordingly, the specific gravity of urine and its osmolarity decrease. In the case of severe vascular damage to the kidneys, leading to a significant decrease in renal blood flow, their pressor effect on blood pressure levels increases, which stabilizes at a high level and is difficult to correct with medication (see Arterial hypertension).
Particularly characteristic is an increase in diastolic blood pressure, which is always above 120-130 mm Hg. Art.
In this regard, phenomena of overload and insufficiency of the left ventricular myocardium, coronary insufficiency, cerebral hemorrhages, swelling of the optic papilla, retinal detachment, and in some cases progressive renal failure may occur.
Survey photographs reveal a decrease in the affected kidney (all or part) and unevenness of its contours.
With urography (see), there is a decrease in the volume of the kidney and the size of the cortical layer. On angiograms (see Renal angiography), convergence and deformation of small arterial vessels are observed (in the nephrogram phase, a decrease in the cortical layer and uneven outlines of the affected lobule are clearly visible).
With radioisotope renography (see Radioisotope renography), there is a slow accumulation, as well as a slow elimination of the radiopharmaceutical drug from the kidneys.
Scintigraphy (see) determines the uneven distribution of the radionuclide in the tissue of the affected kidney; in some cases, its image may be absent or certain areas of the parenchyma may be preserved.
Manifestations of secondary N. can vary from minor impairment of renal function (not clinically expressed) to conditions accompanied by severe arterial hypertension, edema, nephrotic syndrome, a significant decrease in renal function, and the development of severe renal failure.
General principles of treatment and prevention. For N. without signs of renal failure and an unstable increase in blood pressure, treatment consists of Sec. arr. in limiting the consumption of table salt (up to 0.5 g per day) and the use of antihypertensive drugs (rauwolfia derivatives, ganglion blockers, do-pegite, saluretics).
With the development of renal failure due to nephrosclerosis, the use of antihypertensive drugs is also indicated, however, intensive antihypertensive therapy can lead to a drop in renal blood flow and an increase in azotemia; They use a diet with limited salt and protein, anabolic agents, lespene-freel, saluretics.
In the malignant course of hypertension with the rapid development of nephrosclerosis and progression of renal failure, in order to turn off the renin-angiotensive mechanism, they resort to embolization of the renal arteries or nephrectomy (see), patients are transferred to hemodialysis (see) or a kidney transplant is performed (see Kidney transplantation ).
Prevention
nephrosclerosis lies in the timely treatment of diseases leading to its development.
Symptoms of nephrosclerosis
In the initial stages of the disease, specific symptoms may be completely absent. Pathology is often an incidental finding during routine diagnostics or medical examination based on the results of urine and blood tests. As the pathology progresses, the death of nephrons begins to affect the functioning of the renal system, which is manifested by certain, specific symptoms. The intensity and severity of the clinical picture depends on the degree of necrosis in the renal tissue.
Main symptoms:
- attacks of pain in the lumbar spine;
- increased blood pressure levels;
- swelling of the face and lower extremities;
- appetite disorders;
- pronounced, unreasonable weakness;
- aversion to meat dishes;
- decrease in daily urine volume;
- frequent urge to urinate;
- severe headaches that do not respond to analgesics;
- frequent night urination;
- weight loss;
- constant presence of thirst;
- change in urine color (appearance of cloudy sediment or blood);
- attacks of angina pectoris ;
- disturbance of visual perception;
- fragility of bones.
Prognosis for kidney cancer
There is no exact prognosis for survival; it highly depends on concomitant factors: other diseases, the environment, the size and shape of the tumor, and the psychological state of the patient. The most important thing is timely, qualified medical care, which you can receive at our medical center.
What are the numbers?
90% of kidney cancers detected at the first stage are curable. Survival of a patient with stage 4 cancer with metastases is usually less than 1 year.
The chance of surviving 5 years after diagnosis in the first and second stages is 76% and 54%, respectively, in the third stage it is already 42%, in the fourth stage it is about 10%.
What happens if you don't have surgery?
If you do not undergo surgery for early stages of kidney cancer, the survival prognosis will be disappointing. This aggressive form of cancer is removed surgically. Other treatment methods are used to maintain the condition of an already doomed patient and alleviate his symptoms.
What is the most important thing if you are suspected of having kidney cancer?
Medicine does not stand still; new ways to combat kidney cancer at different stages are emerging. Our breast-conserving laparoscopic techniques are among the most advanced in this field. How long you will live after kidney cancer depends on your body and how wisely you choose your doctor. Contact our clinic and we will help you survive this disease.
Tests and diagnostics
At the first signs of deterioration in the renal system, you should contact a nephrologist. The doctor will help you correctly collect anamnesis, take tests and assess the severity of clinical symptoms.
Lab tests:
- Blood chemistry . With nephrosclerosis, there is an increase in urea and creatinine , as well as a decrease in protein. In more advanced stages, the levels of magnesium, phosphorus, potassium and sodium increase.
- General urine analysis . A decrease in specific gravity is recorded, casts, red blood cells and protein are detected.
- General blood analysis . There is a decrease in platelet and hemoglobin .
Hardware diagnostics of nephrosclerosis:
- ultrasound examination of the kidneys;
- excretory urography;
- scintigraphy;
- kidney tissue biopsy;
- Dopplerography of the renal vessels.
Types of disease
Highlight:
- Unilateral hydronephrosis
- Bilateral hydronephrosis
In the first case, the pyelocaliceal complex is affected only on one side, in the second - on both sides. Unilateral damage usually occurs against the background of congenital narrowing, conflict with abnormal renal vessels, as well as urolithiasis. The cause of a bilateral process can be stones, tumors or prostate adenoma.
The doctor knows how to treat kidney hydronephrosis at one stage or another. It is only important for the patient to contact a specialist as soon as possible.
Procedures and operations
If there is no effect from the drug therapy, the progression of the nephrosclerotic process and the inability to restore the functional functioning of the renal system, they resort to hemodialysis or a kidney transplant.
The essence of hemodialysis is to filter the patient’s blood through a special artificial kidney apparatus, thanks to which the body is cleansed of decay products and the water-salt balance is normalized. At the same time, it is recommended to take antihypertensive medications and vitamin complexes .
In the most extreme cases, they resort to kidney transplantation. After surgery, medications are prescribed that suppress the work of the patient’s own immune system to prevent rejection of the transplanted donor organ.
Prevention
There are no specific preventive measures that are guaranteed to prevent the development of nephrosclerosis. If you follow certain recommendations, you can significantly reduce the risk of developing nephrosclerosis:
- drink at least 1.5-2 liters of water daily;
- consume meat dishes and salt in moderation;
- completely eliminate canned products;
- engage in physical education;
- monitor your weight;
- complete cessation of bad habits;
- regular monitoring of blood pressure levels;
- undergo medical examination with examination of the renal system;
- Do not take medications without a doctor’s prescription.
Diet for nephrosclerosis
Diet for kidney failure
- Efficacy: therapeutic effect after 2 weeks
- Timing: constantly
- Cost of products: 1200 - 1300 rubles per week
Diet after kidney transplant
- Efficacy: healing effect
- Timing: constantly
- Cost of products: 1450-1550 rubles. in Week
To achieve maximum results, in addition to therapeutic measures, it is recommended to adhere to a balanced and rational diet if possible. A diet for renal pathology involves reducing the load on the renal system, depending on the degree of nephrosclerosis. Basic recommendations:
- Restriction in protein diet, because it affects the level of urea in the blood. Poultry, rabbit, fish and lean beef are allowed.
- Reduce salt intake. In the early stages of the disease, you can consume a small amount of salt (up to 15 g per day) to control the appearance of swelling in the lower extremities. In more advanced cases, the amount of salt consumed is reduced to 7 g. Salt cannot be completely excluded from the diet, because this can cause dehydration.
- The diet must include legumes, raisins, bananas, green vegetables and whole grain flour products rich in calcium, potassium, and phosphorus.
- The food consumed must be high in calories, because... During illness, the body consumes its own proteins, which can cause an increase in urea levels. The diet must include fruits, potatoes, and butter.
Forecast
Shriveled kidney is a chronic disease that lasts a long time and is characterized by periodic alternation of stages of remission and exacerbation. The number of exacerbations directly depends on proper nutrition and treatment tactics in the fight against the underlying disease.
The prognosis is considered favorable if the pathology is detected at an early stage. The functional state of the renal system deteriorates, and the prognosis is considered unfavorable in the malignant course of nephrosclerosis. The disease can lead to the development of chronic renal failure.
In the most severe cases, the work of the renal system is replaced by hemodialysis or a kidney transplant. Lack of adequate therapy and failure to take measures to maintain the functioning of vital organs and systems can lead to death.
Treatment methods
Therapy should be started as early as possible. It can be carried out by two main methods: medication and surgery. The choice of technique is made exclusively by the doctor. In this case, the specialist takes into account a number of factors, including: the degree of development of the disease, the functionality of the organ, age and other individual characteristics of the patient, the cause of hydronephrosis, etc.
Call now
(495) 7 800 500
Leave a request
You will receive an automatic call back, wait for the operator to respond.
Policy regarding the processing of personal data Consent to the processing of personal data
Make an appointment
Conservative therapy
This treatment is aimed at eliminating pain, as well as fighting infection and preventing complications. It is very important to prevent the development of urolithiasis and kidney failure.
Doctors can prescribe drugs from the following groups:
- antibacterial
- uroseptic
- anti-inflammatory
Important! It should be understood that in most cases, conservative therapy does not get rid of the cause of the disease. It is aimed only at eliminating symptoms and does not allow the pathology to become chronic.
Therapy should be started as early as possible. It can be carried out by two main methods: medication and surgery.
Surgical interventions
Operations are performed to ensure normal urine flow and kidney function.
In case of serious disorders caused by obstructed urine outflow, the following is carried out:
- Stenting.
A stent, which is a flexible and thin tube, is placed in the ureter. It ensures the free flow of urine from the kidney to the bladder. The tube begins in the pelvis area and ends in the bladder. The indication for installation of a stent is the need to ensure the outflow of urine when the urinary tract is blocked. The stent is removed immediately after the cause of the blockage is eliminated - Nephrostomia.
This intervention involves a whole range of surgical techniques. The procedure is temporary and precedes a full-fledged surgical operation to eliminate hydronephrosis. When intervening in the area of the renal pelvis, drainage is inserted in the form of a catheter. The outer end of the catheter is connected to a urinal
Important! Both of these measures are temporary. They only ensure normal urine flow, but do not cope with the cause of hydronephrosis.
The pathology is eliminated exclusively by surgery.
Operations are performed to ensure normal urine flow and kidney function.
Today can be held:
- Laparoscopic interventions
- Manipulations using the da Vinci robot
Experienced doctors who know modern working methods try to carry out interventions using minimally invasive methods. This allows you to reduce the risks of various complications and shorten the patient’s rehabilitation period. Particular attention is paid to organ-preserving technologies.
Interventions are aimed at plastic surgery of the pelvis or ureter, removal of tumors, crushing stones or removing them from organs and cavities. If during the examination it is determined that the functioning of the kidney is partially or completely impaired, operations may be performed to remove it.
Important! Even after removal of the kidney, the patient can return to his normal life (with some restrictions in physical activity and nutrition).
Before starting treatment for kidney hydronephrosis in adults and children, an examination is carried out to assess the cause of symptoms, determine the degree of damage and other features of the course of the disease.