Both women and men can face the problem of urinary incontinence. The disease also often occurs in childhood. It is impossible to self-medicate this pathology, since a non-professional approach can lead to serious complications. Only on the basis of diagnosis and determination of the causes of the disease can a positive result be obtained.
What is cough incontinence?
Urinary incontinence when coughing, or in other words, stress incontinence (stress) is a condition in which involuntary leakage of urine occurs with any increase in intra-abdominal pressure: lifting weights, coughing, sneezing, playing sports.
In mild forms of incontinence, leakage may only occur during excessive, extreme exertion. In more severe cases, even normal walking or changing body position can provoke incontinence, requiring mandatory treatment.
Signs and symptoms
According to medical data, bedwetting in women more often occurs in old age. According to statistics from boarding houses specializing in elderly care, almost 70% of women suffer from this problem.
In the initial stages, there is a slight leakage of urine, which can be dealt with using regular panty liners. If the disease is not treated and left unattended, it worsens over time, causing not only physical, but also psychological discomfort. The patient limits her social circle, rarely leaves the house, and may fall into prolonged depression.
What should older women do with urinary incontinence and can the disease be cured? Medicine recommends treatment at the first signs of the disease, this will help avoid associated complications.
Symptoms of bedwetting in older women that require treatment:
- periodic or regular leakage of urine;
- unbearable urge to urinate, when the patient cannot endure even a few minutes before visiting the toilet;
- Frequent awakenings at night due to the desire to urinate;
- Urine leakage is observed during any physical activity, as well as during sneezing and coughing.
The pathology must be treated as early as possible. If bedwetting in elderly women is not treated in time, in advanced cases it will lead to uncontrolled emptying of the bladder at the first urge. The severe stage of the disease is much more difficult to cure.
What are the treatments for urinary incontinence?
The main treatment for stress urinary incontinence is surgery. Today, the “gold standard” and at the same time the most studied operation is the installation of a synthetic midurethral sling.
Other existing methods, such as the introduction of bulk-forming substances under the urethra, Birch colposuspension, plastic surgery of the anterior vaginal wall, etc., are less effective and can lead to serious side effects, the main of which is disruption of normal urination.
| anonymously to the doctor, through the feedback form, we will try to help you. | ASK A QUESTION |
Diagnostics
To cure the disease, older women need to seek medical help at the first symptoms of bedwetting. At the appointment, the urologist will record complaints and conduct a thorough examination to identify the type of bedwetting, which will help to quickly cure the pathology.
The examination before treatment takes place in several stages:
- collecting the patient’s medical history about the frequency and volume of urine excreted, the number of births and pregnancies, chronic diseases;
- gynecological examination to assess the condition of the genital organs, identify pathologies and their treatment;
- Ultrasound of the pelvic organs and bladder;
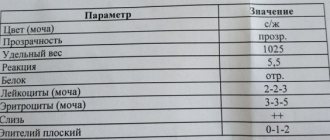
- Analysis of urine.
Depending on the stage of nocturnal urinary incontinence, the urologist may prescribe additional diagnostic procedures before treating the patient. Based on the results of the examination, the doctor decides how to treat urinary incontinence in older women and how long the course of treatment will last.
Pelvic check
In old age, women rarely visit a gynecologist. Having gone through menopause, some patients are sure that there is no longer any reason for regular treatment by a gynecologist. However, according to medical data, older women over 50 have an increased risk of inflammatory diseases of the pelvic organs. In advanced cases, it is extremely difficult to cure them, so you need to visit a doctor every six months.
During the examination, the gynecologist should:
- take a swab to check for infections;
- assess the tone of the pelvic muscles;
- check the woman for the presence of atrophic vaginitis (the disease leads to enuresis, so it needs to be cured).
To detect bedwetting in older women, medicine also offers the Valsalva maneuver and other testing methods.
Assessment of residual urine in the bladder
This test is used in medicine to test the effectiveness of emptying the bladder. The procedure helps to identify and treat hydronephrosis, genitourinary infections or kidney damage in a timely manner. Medicine offers two assessment methods - ultrasound of the bladder or diagnosis using a catheter. The first method is less painful, however, with bloating and other intestinal problems, ultrasound results may be distorted.
(see video after article)
Imaging check
To identify the causes of nocturnal incontinence in medicine, there is no general set of diagnostic procedures suitable for all patients. For each application, the specialist prescribes examination and treatment based on a preliminary diagnosis, taking into account the symptoms of the disease, medical history and tests. To quickly cure pathology, it is important to provide complete information about your health.
How is the operation to install a midurethral sling (TVT, TOT) performed?
This operation is performed under intravenous anesthesia. Through a small (1-1.5 cm) incision on the anterior wall of the vagina, a synthetic sling is installed under the middle third of the urethra.
The sling replaces damaged structures that support the urethra, creating the necessary conditions for urinary retention. The ends of the sling are brought out through small punctures in the skin in the inguinal folds or above the pubis. The duration of the operation, as a rule, does not exceed 10-15 minutes
How many days does hospitalization take? How is the postoperative period going?
The standard period of hospitalization is 2-3 days. The day after the operation, the doctor evaluates the effectiveness of the treatment and, if necessary, adjusts the tension of the sling, setting it in such a way as to achieve complete urinary retention without affecting the quality of urination.
This procedure is performed under local anesthesia. The ability to adjust the tension significantly reduces the risk of postoperative urinary retention and helps achieve optimal results.
What is the effectiveness of surgical treatment for urinary incontinence?
The effectiveness of the operation is up to 90%. There are diseases, the presence of which aggravates the course of the disease and can reduce the effectiveness of treatment - these are concomitant bladder overactivity (the so-called mixed form of urinary incontinence), diabetes mellitus, chronic lung diseases (COPD, bronchial asthma), chronic constipation, obesity.
In patients with a complicated form of stress urinary incontinence (urethral hypomobility, urethral sphincter insufficiency, previous pelvic surgery), the effectiveness of treatment may also be lower.
Risk factors
According to medicine, the following factors can provoke bedwetting in older women:
- frequent pregnancies and difficult births;
- weakening of the pelvic muscles responsible for urinary control;
- genitourinary tract infections if left untreated;
- excess weight;
- significant physical activity;
- eating foods that irritate the bladder (alcohol, spicy foods);
- hormonal changes in the body during menopause;
- Parkinson's disease and other neurological diseases.
Surgical treatment of the pelvic organs can also lead to bedwetting.
What are the risks and side effects of surgery?
Complications associated with the installation of a suburethral sling are extremely rare in expert clinics. Among them are damage to nearby organs (bladder, urethra, abdominal organs), trauma to large vessels, pain syndrome, functional disorders (overactive or atony bladder, difficulty urinating), discomfort during sexual intercourse, erosion of the vaginal mucosa.
In specialized centers, due to the highly qualified surgeons and the use of modern materials, the number of complications is minimized (less than 1%)
Types of incontinence and causes of the syndrome in old age
Urinary incontinence syndrome in medicine is the inability of a patient to control the process of urination. The disease can be temporary or permanent, manifesting itself both at night and during the day. In older women, it often develops due to dysfunction of the genitourinary system, incompetence of the pelvic muscles, etc. The disease can be cured by eliminating the causes of its occurrence.
In medicine, urinary incontinence syndrome is divided into the following types:
- Stressful
– associated with weakening of the pelvic diaphragm and prolapse of the pelvic organs. In older people, weakness of the pelvic floor muscles develops as a result of difficult, protracted labor, physical labor, heavy lifting and participation in “male” sports. It is often caused by chronic diseases of the respiratory system, accompanied by a constant cough, or diseases of the digestive system with regular bowel movements. Therefore, they need to be treated on time. The decrease in estrogen levels during menopause causes the loss of more than 30% of muscle tissue, including the muscles that support the pelvic organs. In older women, advanced stages of nocturnal urinary incontinence are treated surgically. - Imperative (urgent)
– develops due to high activity of the bladder. Even a small amount of urine provokes an unbearable urge to urinate. If the disease is not treated, it will progress. The pathology often occurs against the background of neurological problems and is treated with medication. - Iatrogenic
– develops due to taking a certain group of medications: antidepressants, diuretics or hormonal drugs. Treated by stopping medications that cause incontinence.
In older women, urinary incontinence, including nighttime, can be caused by other pathologies: stroke, multiple sclerosis, cancer. To cure a disease, you need to know the exact cause of its occurrence.
What restrictions exist after surgery?
As a rule, within 5-7 days after discharge from the hospital, women can return to everyday activities - going to work, doing housework. For 1-1.5 months after surgery, patients are advised to lead a gentle lifestyle: avoid lifting heavy objects, active sports, sexual activity, and also refrain from visiting saunas, swimming pools, and taking baths.
It is recommended to pay attention to behavioral habits: avoid smoking, adhere to a balanced diet, normalize body weight.
Is it possible to install a midurethral sling if I am planning a pregnancy?
After implantation of the prosthesis, you can safely plan a pregnancy and give birth through the birth canal. At the same time, the risk of relapse of the disease does not exceed 20% (regardless of whether a Caesarean section was performed or the birth was vaginal).
Bibliography
- Centers for Disease Control and Prevention. (2014). Prevalence of Incontinence Among Older Americans (PDF, 1.3 MB). National Center for Health Statistics. Vital Health Statistics; 3(36).
- Reddy, J., & Paraiso, M. F. R. (2010). Primary Stress Urinary Incontinence: What to Do and Why. Reviews in Obstetrics & Gynecology; 3(4): 150–155.
- Stewart, W. F., et al. (2003). Prevalence and Burden of Overactive Bladder in the United States. World Journal of Urology; 20(6): 327–336.
- American College of Obstetricians and Gynecologists. (2016). Urinary Incontinence (PDF, 84 KB). (link is external)
- Altman, D., Granath, F., Cnattingius, S., & Falconer, C. (2007). Hysterectomy and Risk of Stress-Urinary-Incontinence Surgery: Nationwide Cohort Study. (link is external) Lancet; 370(9597): 1494–1499.
- Gleason, J. L., Richter, H. E., Redden, D. T., Goode, P. S., Burgio, K. L., & Markland, A. D. (2013). Caffeine and Urinary Incontinence in Women. International Urogynecology Journal; 24(2): 295–302.
- Sangsawang, B., & Sangsawang, N. (2013). Stress Urinary Incontinence in Pregnant Women: A Review of Prevalence, Pathophysiology, and Treatment. International Urogynecology Journal; 24(6): 901–912.
- Kim, D. K., & Chancellor, M. B. (2006). Is Estrogen for Urinary Incontinence Good or Bad? Reviews in Urology; 8(2): 91–92.
- Health Resources and Services Administration, Agency for Healthcare Research and Quality. (2012). Nonsurgical Treatments for Urinary Incontinence in Adult Women: Diagnosis and Comparative Effectiveness (PDF, 12.9 MB). Comparative Effectiveness Review; 36.
- US National Library of Medicine. (2017). Kegel exercises – self-care.
- Institute of Medicine. (2004). Dietary References Intakes: Water, Potassium, Sodium, Chloride, and Sulfate (link is external).
- Rosinger, A. and Herrick, K. (2016). Daily water intake among US men and women, 2009–2012. National Center for Health Statistics Data Brief; 242.
- American College of Obstetricians and Gynecologists. (2017). Surgery for Stress Urinary Incontinence (PDF, 85 KB). (link is external)
- Food and Drug Administration. (2018). Considerations about surgical mesh for SUI.