Testicular inflammation or orchitis is inflammation of one or both testicles. It is most often the result of infection with the mumps virus. This is a nasty problem. If left untreated, it can lead to many complications and even infertility.
The testes are the male reproductive glands that produce male gametes (sperm) and hormones. Sex cells first accumulate in the testes (tubes located above and behind each testicle). Of these, as part of sperm, they enter the vas deferens, and then come out, passing the prostate and urethra.
Causes of testicular inflammation
The content of the article
Men over 45 who have a urinary tract infection or who have a catheter are at increased risk.
Known causes of orchitis:
- Bacteria - most often Escherichia coli, staphylococcus, streptococcus and Klebsiella pneumoniae. Prostate infection and epididymitis (inflammation of the testicles) may occur.
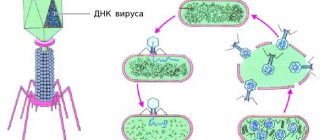
- Viruses - in almost 70% of cases, the cause is mumps - this is an infectious viral inflammation of the parotid glands that swell on one or both sides of the face.
- Sexually transmitted diseases: gonorrhea, chlamydia.
Prevention
Orchitis and the complications it can cause are extremely painful for men, both physically and psychologically. Removal of a testicle or infertility often becomes a real tragedy, so it is extremely important to follow simple preventive measures that can prevent the development of the disease:
- Prevention and timely correct treatment of any disease of the sexual or urinary system.
- Compliance with the rules of personal hygiene, protection of the genital organs, in particular the mucous membranes, from injury, hypothermia and overheating.
- Regular sex life with a regular partner, use of protective equipment.
- Maintaining a healthy lifestyle, proper nutrition.
- Protecting the body's immune status.
- Mumps vaccination.
Remember! Only prevention and timely correct treatment will prevent complications of the disease and maintain a man’s quality of life at the proper level.
Symptoms of testicular inflammation
Signs of orchitis:
- pain in one or both testicles (inflammation of the right or left testicle), it can spread to the groin;
- sensitivity of the testicles to touch;
- edema (swelling) of the testicles;
- testicular erythema (redness);
- frequent urination;
- burning before, during and after urination;
- possible pain when urinating;
- discharge from the penis;
- painful ejaculation;
- blood in semen;
- heat;
- nausea;
- vomit;
- pain during intercourse.
Symptoms and forms of orchitis
Orchitis can occur in both acute and chronic forms. Depending on this, the clinical picture of the disease differs.
Symptoms of acute orchitis
Signs of general intoxication. When infectious agents penetrate, the body is poisoned with toxins - waste products and decay of pathogenic microorganisms. Depending on how reduced the patient’s immunity is, signs of intoxication may be expressed to a greater or lesser extent. The “classic” symptoms are:
- increase in body temperature to 38˚C and above;
- weakness;
- pain in muscles and joints;
- headaches, dizziness;
- nausea, vomiting;
- chills
Severe pain in the testicle, which can not only be localized where the inflammatory process occurs, but can also radiate to the lumbar, sacral and inguinal region. Patients indicate that the pain is of significant intensity and intensifies while walking and touching the affected testicle. Severe pain is due to the fact that with orchitis, swelling develops and, as a result, the tunica albuginea of the testicle, which contains a large number of nerve endings, stretches.
Increased pain is noted if a purulent form of orchitis develops. In this case, the patient requires immediate medical attention for surgical treatment. The purulent process is also dangerous due to its complications: melting of testicular tissue can cause secretory infertility.
On the affected side, the scrotum doubles in size or more. After a few days, the skin turns red and acquires a peculiar glossy shine.
Even in the absence of adequate therapy, in most cases the patient's condition with acute orchitis improves after 2-4 weeks, except in cases where an abscess forms.
Still have questions?
Request a call
Features of orchitis resulting from mumps are:
- inflammatory process. It can develop in the testicle as early as the 3rd day from the onset of the disease (mumps). In some cases this happens later, up to 7 days after recovery;
- in approximately 30% of cases, the pathological process affects both testicles;
- Often a complication of orchitis, which is caused by paramyxovirus, is testicular atrophy.
Symptoms of chronic orchitis
As a rule, the development of chronic orchitis is facilitated by the lack of treatment for the acute form, as well as the presence of chronic inflammatory processes in the organs of the scrotum.
The course alternates between a sluggish inflammatory process and periodic exacerbations. Symptoms of general intoxication are not pronounced, but the size of the testicle is moderately enlarged, it feels firm to the touch, and the skin in the affected area is hyperemic.
Patients note that pain is present, but is of moderate intensity, increasing with exacerbation. Usually, pain outside of an exacerbation is practically not felt at rest.
Chronic orchitis is often accompanied by infertility. This is due to a pathological process that occurs over a long period of time in the tissues of the testicle. The secretory function of the organ suffers: the process of sperm formation (spermatogenesis) worsens.
If you have any questions related to the forms and symptoms of orchitis, as well as the treatment of orchitis, you can ask them to the doctors at Nova Clinic. You can make an appointment with a doctor by calling the number listed on the website or using the booking button.
Treatment of testicular inflammation
If these symptoms are noticeable, you should consult a urologist who will do a history, physical examination, urine culture, blood tests, and ultrasound.
If orchitis is bacterial in nature, treatment is carried out with antibiotics for 10 to 14 days.
On the other hand, if the cause is mumps (a virus), then analgesics and nonsteroidal pain relievers (ibuprofen, naproxen, or acetaminophen) are taken. The resulting inflammation will subside within 1 to 3 weeks.
If fever, nausea, and vomiting occur, the patient may be admitted to the hospital for intravenous antibiotics.
Diagnosis of orchitis
Any changes in the testicular area (redness of the skin, swelling, pain) require an immediate visit to a consultation with a urologist-andrologist. This problem should be addressed to a urologist-andrologist. The doctor will prescribe the necessary examination, which may include various research methods.
Visual inspection
Visual examination, during which external pathological changes are revealed: an increase in the size of the scrotum on the side of the affected testicle, redness and a glossy sheen of the skin. On palpation, the vas deferens can be easily felt; the size of the epididymis most often remains normal. There is swelling along the spermatic cord.
If a purulent form of orchitis develops, upon palpation the doctor can identify a symptom such as fluctuation. What it is? When you press briefly on the testicle, the specialist feels that the surface is springy. This happens due to the fact that there is liquid content in a closed cavity with elastic walls.
Ultrasound
1. Ultrasound of the scrotum with Doppler ultrasound is an informative method for diagnosing orchitis, which makes it possible to differentiate this disease from other genitourinary pathologies.
Echo signs of orchitis
:
- thickening and hyperechogenicity of the tunica albuginea of the testicle
- increased echogenicity of testicular tissue
- increase in testicle volume and size
- significant increase in blood flow velocity in the testicular artery
- increased vascularization (formation of new blood vessels in the tissue)
- in some cases a hydrocele may be detected
2. Ultrasound of the prostate gland to exclude prostatic hyperplasia in older patients
Testicular biopsy
It may be necessary to remove a piece of testicular tissue for examination.
Analysis of urine
Urinalysis (general and bacteriological examination with determination of sensitivity to antibiotics). Markers of the inflammatory process are detected:
- leukocyturia (increased number of white blood cells)
- hematuria (presence of red blood cells)
- presence of cylinders.
Bacteriological culture allows you to identify the causative agent of infection and determine its sensitivity to certain antibacterial drugs.
Urethral swab
Examination of urethral discharge allows not only to find out which pathogenic microorganisms caused orchitis, but also to assess the stage of the inflammatory process.
Spermogram
A spermogram allows you to determine the degree of reproductive dysfunction, and also makes it possible to detect in the ejaculate:
- Leukocytes (leukospermia)
- Red blood cells (hemospermia)
- Pus (pyospermia)
What is the prevention of inflammatory diseases of the scrotal organs and their complications?
To prevent the diseases described above and their complications, you should, first of all, avoid contracting sexually transmitted infections and treat them in a timely manner, not be exposed to sudden hypothermia, and protect the scrotum from injury. You should give preference to tight-fitting panties and dress warmly in winter. If you have the above-described signs of epididymitis, orchitis and orchiepididymitis, you should urgently consult a urologist!
| Hello. Six months ago, a nagging pain arose in the scrotum. I did an ultrasound and discovered a varicocele on the left, the veins were dilated to 3.9 mm and a fluid formation of the appendage on the right was 4.2 mm. I did a prostate ultrasound - dilatation of the veins of the paroprastotic plexus on the left by 3.5 mm. The pain does not go away what should I do thanks in advance Look at other questions or ask your own on the topic: Pain in the scrotum |
What is the treatment for inflammatory diseases of the scrotum?
Treatment of epididymitis, orchitis, orchiepididymitis and deferentitis is carried out primarily with antibiotics, since their main cause is various infections. The choice of antibiotic for an acute inflammatory process is carried out empirically, taking into account the known age-related characteristics of the causative infections. Upon receipt of the results of microbiological studies and analysis of the sensitivity of the isolated microflora to antibiotics, it is possible to adjust antibiotic therapy, change its duration, dosages of drugs, and sometimes the drugs themselves and their combinations.
Along with antibiotics, non-steroidal anti-inflammatory drugs (indomethacin, diclofenac, Celebrex, etc.) are prescribed in order to reduce inflammatory swelling, pain and quickly reverse the development of inflammatory changes. For severe pain, a blockade of the spermatic cord with a local anesthetic (lidocaine, prilocaine, marcaine) is used, which significantly reduces pain. All patients are recommended to wear tight panties (swimming trunks) that tighten the scrotum during treatment. This promotes better blood and lymph flow in the scrotum and accelerates the reverse development of inflammation.
In the presence of ulcers or abscesses of the testicle and its epididymis, as well as in chronic recurrent epididymitis, which is difficult to treat, in the case of testicular tuberculosis, surgical treatment is used. It may involve opening and draining abscesses, partial or complete removal of the testicle and/or its epididymis. The use of various methods of physiotherapy for inflammatory diseases of the scrotal organs has not proven its effectiveness in correctly conducted scientific studies and is not included in the international standards for the treatment of epididymitis, orchitis and orchiepididymitis. In this regard, we do not use physiotherapeutic methods for treating these diseases in our practice.
Epididymitis and infertility
The epididymis is a paired organ of the male reproductive system that plays an important role in metabolism, maturation, accumulation and promotion of sperm. The epididymis contains the head, body and tail. The tail of the epididymis passes into the vas deferens.
Sperm accumulate in the epididymis for the purpose of maturation. Inside there is an optimal environment for sperm to mature (temperature, pressure, etc.). Inflammation of the testicle makes it difficult to perform the function of this reproductive organ, which adversely affects the quality of sperm. Moving along the duct, they are finally formed and become mobile.
In advanced forms of chronic epididymitis, connective tissue grows in the epididymis, which in turn can lead to obstruction of the duct. Obstructive infertility occurs with bilateral disease of the appendages (expressed in impaired sperm formation in the testicles).
Reference! When one side of the epididymis is inflamed, sperm obstruction is observed; infertility may not occur; in this case, the number of sperm is significantly reduced.
Timely seeking medical help and prescribing the correct treatment, the ability to fertilize returns. Even if only 30% of the duct patency is restored during treatment, doctors can take a puncture biopsy of sperm and use it for IVF.
Preventive measures
In order to avoid the development of these diseases, you must follow simple rules:
- lead an active life, constantly play sports;
- eliminate blood stagnation during sexual abstinence through physical exercise;
- eat right, including foods high in minerals, beneficial microelements and proteins in your diet;
- timely treat all diseases of an inflammatory and infectious nature;
- give up cigarettes and alcohol consumption;
- lead a regular intimate life, do not change partners frequently, avoid unprotected and interrupted sexual intercourse;
- avoid overheating and hypothermia of the body.
Performing preventive procedures will minimize the risk of orchitis and epididymitis. However, it is worth remembering that at the slightest suspicion of the development of pathology, you should immediately consult a doctor. Only timely diagnosis and treatment will avoid complications.
How to treat orthiasis in men?
Treatment of orchitis consists of prescribing medications that are aimed at eliminating the source of inflammation. First of all, antibiotics are recommended. Paracetamol is most often prescribed to reduce fever. To eliminate pain and improve the outflow of sperm, antispasmodics are prescribed.
Treatment regimen for orchitis:
- Pathogenetic treatment - the use of anti-inflammatory drugs “Indomethacin”, “Ibuprofen”, painkillers “Baralgina”, “Ketorol”, angioprotectors “Venorus”, “Detralex”, vitamin complexes.
- Etiotropic treatment is aimed at eliminating the cause of the disease. Antibiotic therapy is carried out: patients are prescribed drugs from the group of fluoroquinolones - Ciprofloxacin, Ofloxacin, cephalosporins - Cefotaxime, Cefazolin or macrolides - Azithromycin, Clarithromycin.
- Physiotherapeutic procedures have an anti-inflammatory, local immunostimulating and restorative effect. Patients with chronic orchitis are prescribed UHF therapy, magnetic therapy, laser therapy, acupuncture, electrotherapy, physical therapy, mud and mineral baths.
- Patients with an acute form of the disease are advised to have bed rest, a minimum of movements, rest and an elevated position of the scrotum, and the use of a support bandage that improves blood circulation in the inflamed organ and eliminates congestion in the pelvic organs.
At home, cold compresses are used as a pain reliever. Every 4 hours, a compress is applied to the scrotum for 10 minutes. Treatment of orchitis includes following a diet and giving up bad habits. Spicy, sour and salty foods should be excluded from the diet.
Routes of infection and risk factors
There are several ways of contracting orchitis, which depend on the causes of its occurrence. When infected by viruses, the infection process is hematogenous in nature. When infected with sexually transmitted diseases, the only route of infection is contact.
Risk factors for developing the disease are:
- HIV status;
- diabetes;
- severe form of infectious diseases;
- other factors of immunosuppression;
- taking hormones, chemotherapy or immunosuppressants and others.
Surgical intervention
If conservative treatment of orchitis does not bring the required results, then the question of surgical intervention is raised.
Indications for its implementation are:
- tuberculous nature of the disease;
- frequent exacerbations in chronic orchitis;
- tissue suppuration;
- acute form, developed as a result of injury;
- severe course of the disease, etc.
Depending on the complexity of the case, surgical intervention can be performed using several methods. With the least consequences for functioning, resection is performed - removal of the inflamed part of the testicle. If the operation is insufficiently thorough and in the case of a number of other factors, complications and relapses are possible.
In case of severe purulent lesions - orchiectomy - removal of the testicle and epididymis. If the operation affects both organs, this leads to a significant decrease in the level of male sex hormones and infertility. The attending physician may also suggest other surgical techniques.
Epidemiology of orchiepididymitis
An infectious-inflammatory process that simultaneously affects both the testicle itself and the epididymis is called epididymitis orchioepididymitis. The term includes the names of two anatomical structures at once - the testicle (orchitis) and its epididymis (epididymitis). The ending “-itis” in both words means an inflammatory process.
These diseases, as a rule, occur together, which is why they are referred to by the same term. After all, microorganisms that penetrate the epididymis enter the testicle itself, and vice versa. The infection penetrates the male reproductive glands through the bloodstream.