Non-ossifying fibroma (NOF) is a common benign bone lesion in children and adolescents, consisting of proliferating elongated fibroblasts, combined with a variable number of multinucleated osteoclast-like giant cells [7]. There are several synonyms: metaphyseal fibrous defect (MFD), cortical fibrous defect (CFD), histiocytic fibroma and fibrous xanthoma. When we are talking about small lesions of the cortical layer, the term MFD or KFD is more often used. When the lesion spreads medullarily, and even more so when there is a threat of pathological fracture, the term NOF is used.
In most cases, NOF has no clinical symptoms and, as a rule, is an incidental finding during examination. With actively enlarging lesions, complaints of local pain sometimes appear [10]. Some researchers consider NOF not as a true tumor, but as a local defect of osteogenesis during the growth of skeletal bones [1]. Multiple lesions are rare, more often within the framework of Jaffe-Campanacci syndrome, which, in addition to multiple NSF, is characterized by the presence of light brown spots on the skin (Café au lait spots), may be accompanied by mental retardation, hypogonadism or cryptorchidism, malformations of the cardiovascular system, eyes, and also be combined with neurofibromatosis [3, 4].
The detection rate of MFD/NOF reaches 30%. Since clinical symptoms are most often absent, the true prevalence of this pathology remains unknown. MFD/NOF is registered more often in children and adolescents, rarely in those under 5 years of age and in adults over 20 years of age.
Despite the high prevalence of this pathology, the awareness of surgeons, radiology specialists and pathologists regarding the latter remains extremely low.
Material and methods
We analyzed 678 cases of tumors and tumor-like bone lesions in children and adolescents from January 2009 to June 2015. NOF/MFD were identified in 35 patients. In each case, data from the medical history (gender, age, location, complaints, treatment), X-ray (and/or CT examination) and MRI examination (if available) and histological material were analyzed. All patients underwent surgical treatment (excochleation). In each case, differential diagnosis was made with fibrous dysplasia, aneurysmal bone cyst, giant cell tumor, chondromyxoid fibroma, and desmoplastic fibroma.
Treatment
If there is a defect measuring less than 1/3 of the diameter of the bone tissue (no pathological fracture), conservative treatment and observation is possible with the exception of physical activity until the lesion is closed. If there is pain and the lesion is more than 1/3 in diameter, surgical intervention in the form of marginal resection and bone grafting (auto- or allografts) is necessary. In the presence of a pathological fracture, extrafocal osteosynthesis is performed.
MFDC always proceeds benignly; after adequate surgical intervention, the disease does not recur.
You can obtain more detailed information about the MFKD and the procedure in your particular case by contacting our call center by phone.
results
In our study, in the structure of all tumors and tumor-like bone lesions in children and adolescents, MFD/NOF amounted to 5.16%.
The age of the patients varied from 7 to 18 years, the largest number of observations was noted at the age of 12 to 18 years. The age distribution is shown in Fig. 1.
Rice. 1. Distribution of MFD/NOF by age.
Multiple lesions were observed in one patient (boy, 14 years old) in the distal metaphysis of the left femur and proximal metaphysis of the left tibia. The patient underwent excochleation of the left tibia.
The number of female patients slightly exceeded the number of male patients (20/15). However, according to the literature, this pathology is somewhat more common in boys [1].
The size of the formation varied widely: from 0.8 cm (in diameter) to 8×5×4 cm (the case was complicated by a pathological fracture).
As a rule, there were no complaints at the time of discovery of the formation. Some patients noted inconsistent pain during exercise. The pain syndrome was mainly expressed with a large volume of damage to the distal metaphysis of the femur. In 2 (5.71%) cases, a pathological fracture was detected due to a large volume of bone damage.
Two children had a recurrence of the tumor after surgical treatment (after 2 and 3 years, respectively).
NOF/MFD are most often found in the metaphyses of long tubular bones, the vast majority in the bones of the lower extremities (distal metaphysis of the femur, proximal and distal metaphyses of the tibia and fibula). The most common localization, according to our observations, was the distal metaphysis of the femur and the proximal metaphysis of the tibia (Fig. 2).
Rice. 2. Localization of MFD/NOF in our observations.
The clinical diagnosis before surgical treatment in most cases (22, 62.85%) was fibrous dysplasia, in 3 (8.57%) cases - giant cell tumor, in 2 (5.71%) - osteomyelitis, in 1 (2.85%), 85%) - osteoid osteoma, 1 (2.85%) - osteosarcoma, 3 (8.57%) - bone tumor, unspecified. The diagnosis of cortical fibrous defect was made before surgical treatment in only 3 (8.57%) patients, which directly indicates a low level of awareness of this pathology among surgeons and radiology specialists.
In one case (a 10-year-old girl), a morphological diagnosis of giant cell tumor was made due to the large number of giant multinucleated osteoclast-like cells. However, upon review of the x-rays (well-circumscribed oval lesion in the cortical layer of the distal metaphysis of the femur with a perifocal zone of sclerotic changes) and histological material (spindle cell lesion, curtain-shaped pattern, no mitotic activity detected, groups of xanthoma cells, hemosiderin deposits), as well as, Taking into account the age (giant cell tumor is casuistically rare in children and adolescents), the diagnosis was changed to MFD.
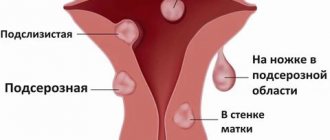
Types of fibroids
There are two types of tumors: soft and hard.
Soft fibromas in a child are characterized by very slow growth, rather flabby consistency, mobility and clear localization. Such growths occur mainly in the genital area and anus, sometimes forming multiple clusters. Solid neoplasms are smooth or slightly rough pink and flesh-colored nodules with dense contents. Such fibromas are located on a wide base and, as a rule, do not exceed 1 cm in size.
Discussion
MFD/NOF are localized in the metaphyses of long tubular bones and, as the skeletal bones grow, they can shift slightly towards the diaphysis. It is well known that the metaphysis and growth plate areas are the sites of the most intense bone growth in children and adolescents. Consequently, MFD/NOF as a local “osteogenesis defect” occurs in this zone. Some authors believe that the trigger for the development of MFD/NOF can be a minor injury with subperiosteal hemorrhage [5]. Most lesions occur around the knee joint, but cases have also been described in the pelvic bones, vertebrae, clavicle [8], even in the lower jaw [1, 2]. However, when examining tumors of the lower jaw, the first step is to carry out a differential diagnosis with giant cell reparative granuloma.
A case of a combination of NOF with osteosarcoma of the distal metaphysis of the femur in a 15-year-old girl is described [10].
On X-ray examination, the MFD appears as a round or oval lytic formation of the cortical layer (or subperiosteal), often slightly elongated parallel to the axis of the bone. The boundaries are clear, as a rule, a small zone of osteosclerosis around is clearly visible (Fig. 3). As the MFD grows, it begins to spread in the medullary direction. Therefore, NOF always looks eccentric, but also with clear boundaries and a zone of perifocal osteosclerotic changes (Fig. 4). With large lesions that occupy more than a third to half of the diameter of the bone, lobulation can often be detected due to sclerotic septa, in which histological examination reveals fibrous tissue with foci of reactive osteogenesis. In these cases, the disease can manifest itself as a pathological fracture. In rare cases, the contours of the NOF may extend beyond the anatomical limits of the bone. There is no periosteal reaction in most cases.
Rice. 3. Well-defined cortical lesion in the area of the distal metaphysis of the femur. Perifocal sclerotic changes are not pronounced. Stage A according to Ritschl.
Rice. 4. Well-defined lesion of the distal metaphysis of the tibia with pronounced perifocal sclerosis, more pronounced in the area of the diaphyseal pole of the formation. Stage D according to Ritschl.
P. Ritschl et al. [6] described the process of evolution of MFD and NOF from their onset to complete sclerosis, based on radiological data and identified 4 stages: A, B, C and D. Stage A: a small cortical round or oval eccentric lesion located near the growth zone (close to pineal gland). The area of perifocal sclerosis is practically absent. Stage B: the lesion distances itself from the epiphysis, acquires irregular polycystic outlines, and a thin sclerotic rim appears along the periphery. Stage C: sclerotic changes become pronounced, and begin, as a rule, from the diaphyseal pole of the formation. Stage D: the formation is completely replaced by a homogeneous zone of sclerotic changes. The MFD/NOF is then replaced by normal bone tissue and is not detected radiographically. Active growth of MFD and NOF occurs at stages A and B; when formation was detected at stages B and C, no increase in size was observed in dynamics.
The X-ray picture of NOF/MFD is so typical that in the vast majority of cases the diagnosis can be made only on the basis of this study. Since NOF/MFD belong to the “leave me alone lesion” group of bone lesions, this serves as a basis for observation and periodic radiological monitoring. Due to the fact that NOF/MFD can regress spontaneously during the growth and maturation of skeletal bones, active surgical tactics are not always justified. Surgical treatment methods are used only for large volumes of formation, when there is a threat of a pathological fracture or when the NOF manifests itself as a clinically pathological fracture.
According to the Enneking staging system, benign tumors of NOF/MFD in most cases have stage I (G0T0M0), in rare cases, when they spread beyond the normal anatomical boundaries of the bone - stage II.
On macroscopic examination, the lesion is clearly circumscribed and yellowish-gray in color (Fig. 5). Cystic changes and areas of hemorrhage may occur. Areas of necrosis may be identified after a pathological fracture.
Rice. 5. On macroscopic examination, the lesion is clearly limited, yellowish-gray in color.
On histological examination, the formation is well circumscribed and consists of fibroblast-like spindle-shaped cells forming randomly oriented bundles and curtain-shaped structures (Fig. 6). The nuclei are oval or elongated; small nucleoli are not detected in all nuclei. Mitotic activity is not reliably determined or only a few mitotic figures are detected. One of the consistent morphological features is the identification of clusters of large histiocytes or xanthoma cells with abundant clear cytoplasm. It is almost always possible to detect small scattered granules of hemosiderin, which are better visible with a special histochemical stain for iron. Clusters of giant multinucleated osteoclast-like cells can often be identified (Fig. 7). Cystic changes of the type of secondary aneurysmal bone cyst are often found. With a large volume of formation, zones of reactive osteogenesis can be identified in the form of coarse fibrous bone tissue (woven bone), zones of hypocellular mature connective tissue. If NOF is complicated by a pathological fracture, areas of necrotic changes are often identified.
Rice. 6. Typical histological picture of MFD/NOF. Spindle cell component, xanthoma cell clusters and hemosiderin deposits. Hematoxylin and eosin staining, ×400.
Rice. 7. MFD/NOF are always clearly limited, in places they can contain a large number of giant multinucleated osteoclast-like cells. Hematoxylin and eosin staining, ×300.
Differential diagnosis should include fibrous dysplasia, aneurysmal bone cyst, giant cell tumor, chondromyxoid fibroma, and desmoplastic fibroma.
Fibrous dysplasia by definition is a benign medullary fibro-osseous lesion in which one or more bones are involved in the pathological process. It is more often found in the bones of the skull and femurs, less often in the ribs, pelvic bones, etc. Radiologically, it looks like a well-defined lesion, but unlike MFD, it is not localized cortically. NOF is always an eccentric formation, spreading medullarily from the cortical layer. On histological examination, fibrous dysplasia consists of two components: fibrous (in the form of relatively hypocellular mature connective tissue with elongated fibroblasts) and bone (in the form of bizarre bony trabeculae, usually without perifocal osteoblastic rimming). In NOF there is no bone component; areas of reactive osteogenesis can only be determined, especially in the presence of a pathological fracture.
A solid variant of aneurysmal bone cyst (ABC) is rare. Most often localized in long tubular bones. On X-ray examination, the ACC, as a rule, is well limited in the form of a lytic focus, often extends beyond the normal anatomical limits of the bone, and sometimes a clear border with the soft tissue component may be lost. Histological examination does not show a pronounced curtainform pattern as in MFD/NOF; multiple foci of reactive osteogenesis (woven bone) are detected. Primary ACC exhibits t(16;17) with UPS6 gene rearrangement.
Giant cell tumor (GCT) practically does not occur in children and adolescents and begins to be registered at the end of the second - beginning of the third decade of life, while MFD/NOF occur in children and adolescents. Localization is epiphyseal-metaphyseal, long tubular bones are affected. In approximately half of the cases, it is diagnosed in the bones around the knee joint: the distal part of the femur, the proximal metaphysis of the tibia and fibula. In histological examination, the mononuclear component is often represented by oval-shaped neoplastic cells; the nuclei of mononuclear cells in GCTs are identical in morphology to the nuclei of multinucleated osteoclast-like cells [9].
Chondromyxoid fibroma (CF) is a benign tumor consisting of elongated myofibroblast-like and stellate cells with a chondroid and myxoid matrix. Can be detected at any age. It is more common in long tubular bones in the second and third decades of life, more often among male patients. The most significant clinical symptom is pain (from several months to several years). X-ray is detected in the metaphyses of long tubular bones as a sharply limited eccentric focus, often without an accentuated zone of sclerotic changes in the peripheral parts. In MFD/NOF, the zone of sclerosis along the periphery is always well defined. Histologically, CP consists of lobules with a relatively hypocellular center and increasing cellularity towards the periphery. The cells lie in a chondroid and/or myxoid intercellular matrix. Mitotic activity is not reliably determined or is low.
Desmoplastic fibroma (DF) is a rare benign, locally aggressive bone tumor composed of spindle cells and collagenized matrix. It is an analogue of deep soft tissue fibromatosis. Occurs at any age, including children and adolescents. Any bone can be involved in the pathological process, but more often it occurs in the lower jaw, metaepiphyseal zones of the femur, tibia, radius, humerus, as well as in the pelvic bones. During X-ray examination, as a rule, the contours of the pathological focus extend beyond the anatomical boundaries of the bone. DF is well limited, often has a “honeycomb” structure, sometimes soft tissues are involved in the pathological process, in some cases a periosteal reaction is observed, which does not happen with MFD/NOF. Histologically, the DF consists of bundles of spindle-shaped fibroblast-like cells with a pronounced collagenized intercellular matrix. Immunohistochemical examination often reveals a nuclear reaction with an antibody to β-catenin.
Causes
The exact culprit behind the development of fibroids in children has not yet been determined. Experts have identified a number of factors contributing to the appearance of tumors. These include:
- unfavorable environmental living conditions (proximity to chemical and cement plants, landfills, contaminated areas);
- frequent injuries, bruises and falls;
- various infectious diseases of acute and chronic form;
- irrational use of potent drugs;
- endocrine pathologies;
- prolonged exposure to direct sunlight.
Preventive measures
Due to the fact that the pathogenesis of this lesion is difficult to trace, it is impossible to say exactly what should not be done to cause the disease to occur. Experts give the following recommendations:
- conduct an annual medical examination, as this will help to detect the problem in time;
- seek medical help in a timely manner;
- eat a balanced diet;
- do not self-medicate, especially when it comes to fractures;
- do not carry heavy objects, reduce physical activity;
- do exercises.
Non-ossifying fibroma does not pose a health risk if detected in time. Although it does not lead to negative consequences, it is better to avoid it. To do this, it is necessary to carry out preventive measures that will protect not only from bone damage, but also from many other diseases. Otherwise, you may get a fracture of the femur or tibia.
Prevention
There is no specific prevention that can eliminate the likelihood of fibroids. You can reduce the chance of neoplasms forming by carefully monitoring the health of your children.
- It is necessary to bring children regularly for preventive examinations.
- It is advisable to avoid prolonged exposure of children to direct sunlight, especially during the period of greatest sun activity.
- It is necessary to promptly and correctly treat infectious diseases, injuries, burns and other damage to the skin or internal organs.
You should not give children medications without the instructions of doctors, or try traditional and non-traditional treatment methods. It is also important to ensure that babies eat properly and get enough physical activity on a daily basis.
Fibroids do not always pose a danger to the body, however, they must be kept under control. Doctors at the SM-Doctor clinic will carefully examine the child and select the optimal method of treating the disease.
Diagnostics
Initially, experienced specialists - oncologists or multidisciplinary surgeons - conduct a detailed examination of the patient, record all the complaints that exist, palpate the formation and make a preliminary diagnosis. Then you need to determine the nature of the tumor. After this, you need to conduct an ultrasound examination of the tissues where the tumor is located to determine its size, nature, and changes in the tissues. If necessary, an X-ray examination is performed. If questions remain, a biopsy of the suspicious area should be performed to rule out a malignant process.
Fibroids can be detected by palpation (feeling with fingers or hands) performed as part of a pelvic examination, or diagnosed through imaging procedures such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI).
What it is?
Non-osteogenic or non-ossifying fibroma occurs not only in older people, but also in children and adolescents. Such pathological changes in the body require medical intervention. Non-osteogenic fibromas are benign neoplasms consisting of tissues whose cells synthesize extracellular structure.
Non-osteogenic fibroma includes damage to the tibia or femur. The pathology is characterized by the dissolution of the outer bone layer, which forms the bone crust. The tubular section, which is adjacent to the cartilaginous plate, also dissolves. After the process of resorption of the tubular section, it is replaced by the epiphyseal line. The outer bone layer is replaced by fibrous tissue, which serves as a building material for tendons and is unable to fully recreate the bone cortex. Due to such pathological replacement, unnatural fractures of the arms and legs occur.
Fibroma shape
Tibial fibroids have a characteristic elongated appearance. The edges of the damaged bone are surrounded by cells and fibers that look like strange tufts. What are these weaves formed from? shown in the table:
Non-osteogenic fibroma may be composed of fibroblasts, collagen, lipocytes, or a combination of these.
| Biomaterial | Short description |
| Collagen protein fiber | Part of connective tissues. Such fibers perform a mechanical role. They have low elasticity. |
| Cells that produce extracellular substance (fibroblasts) | Extracellular substance is considered the main building material for connective tissues and provides mechanical support for cells. Fibroblasts help release chemical material from the cell (such as elastin). |
| Lipocyte cells | Form scar tissue. |
| Cellular elements | Their presence confirms the inflammatory process in bone tissue. |