Thrombophlebitis (TF) is an inflammatory process that affects the wall of venous vessels, resulting in the formation of blood clots. Depending on the stage of development, several types of the disease are distinguished.
Signs of the development of pathology are an increase in body temperature, redness and thickening in the area of the affected vein, pain, etc. These symptoms should be the reason for mandatory contact with a specialist who will conduct an examination and identify the cause of these symptoms.
Medical offers its clients high-quality and professional assistance from a phlebologist in the diagnosis, treatment and prevention of vein diseases, including varicose veins. In the clinic, equipped with modern equipment and equipment, you can receive high-quality services from experienced doctors at reasonable prices.
What is thrombophlebitis
Thrombophlebitis
(acute thrombophlebitis, superficial vein thrombosis, TPV) is an inflammation of the venous walls with further formation of blood clots. The thrombus is tightly attached to the inflamed vessel. If treatment is started in time, the blood clot will resolve, the inflammation will go away, and the venous lumen will be restored and will not affect blood flow.
The incidence of thrombophlebitis is determined by many factors, one of which is age. Thus, superficial vein thrombosis debuts annually in 0.3-0.6 per 1000 people under 30 years of age and in 0.7-1.8 per 1000 elderly patients. There are also gender differences. In men under 30 years of age, acute thrombophlebitis occurs in 0.05 cases per 1000 patients annually. For women, these figures are significantly higher. Thus, in the first 30 years of life, the onset of TPV is detected in 0.31 per 1000 women, but with age the detection frequency increases to 2.2 per 1000 patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
In 3-11% of patients, thrombophlebitis is localized on the lower extremities. The system of the great saphenous vein is affected in 60-80% of cases, the small saphenous vein - in 10-20%, and bilateral TPV occurs in 5-10% of cases i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Against the background of varicose veins, thrombophlebitis occurs in 4-62% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
Folk remedies
Along with drug treatment, traditional methods can give good results. However, you should not blindly believe and thoughtlessly try everything on yourself. The doctor should control the treatment regimen, the admissibility and effectiveness of folk remedies.
- White cabbage. Cabbage leaves need to be softened, one side greased with oil and secured with a bandage on the painful area. Leave the compress on all night.
- Kalanchoe pinnate. Grind the leaves and fill the jar halfway with them. Fill the rest of the jar with vodka. Next, leave for 7 days in a dark place, shaking the contents periodically. Strain the finished tincture. Rub the sore leg from the foot to the groin in the direction of the vein. So for a month 2 rubles/day.
- Apple vinegar. Mix 2 teaspoons of vinegar and honey in a glass of water. Drink half a glass before meals 2 times a day.
- Mumiyo. You can make a tincture for internal use and ointment:
- for the tincture you need to mix 10g of mumiyo with 0.5l of water - drink 1 tablespoon/1 ruble per day, 10 days
- For the ointment, you need to mix mumiyo with Vaseline (or peach oil) in a ratio of 1 to 5 - smear 3 times a day, leave for 1 hour, 10 days.
Types (classification) of disease
Thrombophlebitis is divided into several types, taking into account the origin and origin of the disease, the localization of the lesion, and the extent of the lesion.
Venous thrombophlebitis is divided according to the affected area into:
- Migratory
. A blood clot appears in one place. Over time, it disappears and appears in another area. The condition is dangerous and requires prompt medical attention. - Local
. A blood clot forms in a specific area. It doesn't have to be the shins. For example, thrombophlebitis of the hand is diagnosed.
Depending on the presence or absence of pathogens, subcutaneous thrombophlebitis occurs:
- Septic
. The infection spreads quickly through the bloodstream, so there is a risk of developing sepsis. Diagnosed after childbirth, surgery and erysipelas. Treated with antibiotics. - Aseptic
. There is no infection, the disease occurs after injury. Most often, varicose thrombophlebitis is diagnosed due to improper or absent treatment.
Depending on the size of the blood clot, the disease can be:
- Occlusive
. The lumen of the vein is completely blocked, so the outflow of blood is impaired. There is a risk of necrosis (tissue death), so immediate surgery is required. - Non-occlusive
. An attached blood clot partially blocks the venous lumen. Blood circulates.
Based on the extent of the pathological process, the following is revealed:
- Thrombophlebitis of the superficial veins
. Symptoms appear immediately. The patient complains of pain along the vein. The surrounding skin turns red and thickens. Over time, swelling forms, which is difficult to eliminate. The temperature is kept within 39 °C. Treated with medication. - Deep vein thrombosis
. This form is detected less frequently and is more severe. The symptoms are the same, but their severity is stronger. The limbs become very swollen and turn blue. If there is a high risk of developing pulmonary embolism, surgery is performed.
First, thrombophlebitis of the superficial veins of the lower extremities develops. If left untreated, the disease develops into deep vein thrombosis, thrombophlebitis of the great saphenous vein.
Mechanism of thrombus formation
The formation of a blood clot always follows one scenario: first, damage occurs (trauma to the vessel wall), platelets rush to the site of damage, which stick together into a strong clot and adhere to the wound. Next, fibrin threads are formed, and the vessel receives a “patch.” Over time, the tissues are restored, the blood clot dissolves as unnecessary.
A useful mechanism that saves people from blood loss due to injury can become dangerous when there is an excess of platelets - thrombophilia. An excess of these blood cells results in blood clots that are too large for minor injuries. The second important factor in thrombus formation is the very presence of damage. Thrombosis becomes a pathology if it begins in the absence of injury to the vascular wall.
Stages
The sequence of development of the disease is as follows:
- Acute stage
. Clinical signs of thrombophlebitis are bright and appear unexpectedly. The temperature rises, the skin around the affected area turns red, and the patient shudders. If treatment is started within two weeks, the development of the disease can be avoided. The blood clot will dissolve. The duration of exacerbation is up to one month. - Subacute stage
. Lasts up to two months. Signs of the disease subside, but do not fade away. The skin remains red and the swollen veins turn blue. The swelling goes away, but the seals remain. - Chronic stage
. Diagnosed two to three months after the disease is detected. Symptoms are either absent or worsened. During remission, the limbs remain swollen, quickly become tired and itchy, but there is no pain. Discomfort occurs in the lower extremities when walking for a long time.
How to avoid thrombosis, prevention
The risk of thrombosis can be reduced by following these recommendations:
- Movement. Nobody talks about increased physical activity, but a walk combined with brisk walking is necessary every day. A sedentary lifestyle leads to blood stagnation and damage to the veins.
- Proper nutrition. The cause of thrombosis can be excessive consumption of carbohydrate, cholesterol foods, saturated with trans fats, as well as alcohol. A healthy diet prevents not only thrombosis, but also many other diseases.
- Wearing compression garments. It is recommended to be worn by people with varicose veins, before and after surgery, as well as during pregnancy. The degree of compression should be determined only by a doctor.
- For periods of prolonged immobility, wear only loose clothing and sit in a relaxed position. Do not cross your legs under any circumstances (this position most often leads to stagnation of blood).
- Patients over 50 years of age should take medications aimed at reducing the risk of thrombosis.
- Monitor the sensations in your body and immediately report any discomfort to your doctor.
How is thrombophlebitis different from varicose veins?
Varicose veins are increased pressure in thinned and inelastic veins, and thrombophlebitis is an inflammation of the venous walls with subsequent formation of blood clots. Most often, the diagnosis of thrombophlebitis is a consequence of varicose veins.
Thrombophlebitis differs from varicose veins in the following symptoms:
| Sign | Varicose veins | Thrombophlebitis |
| Pain | pulling | bursting and stabbing |
| Convulsions | Yes | No |
| Changing the appearance of your legs | noticeable tortuosity and bulging of veins | compactions and lumps when palpated |
| Change in skin color | pale skin, blue veins | red skin |
| Burning feeling | Yes | No |
Both pathologies develop as a result of impaired hemostasis, but inflammation of the venous walls is more often associated with the entry of an infectious agent. The difference is the absence of local inflammation. With varicose veins, the veins do not become inflamed. In this case, only the blood circulation is disrupted.
If the blood clot comes off
The thrombus is not always firmly attached to the wall of the vessel. When a clot is superficially attached, a simple surge in pressure, a blow, or a careless movement is enough for the clot to come off and travel through the circulatory system. Moving through the vessels, the detached thrombus sooner or later reaches the most important organs, and usually the pulmonary vein, if the thrombus was venous, or the left atrium, if arterial.
Pulmonary thrombus
In the most dangerous cases, blockage of the large vessels of the lung occurs, after which death occurs within a few minutes. A less severe option is infarction-pneumonia, when a blocked vessel bursts and the lungs begin to fill with venous blood, which is accompanied by acute pain and hemoptysis. In this case, the patient has every chance of survival.
The mildest case, when a blood clot enters the pulmonary veins, is accompanied by an increase in blood pressure in the lungs, pain, shortness of breath, and suffocation. If you call an ambulance right away, the patient is likely to survive.
Coronary thrombus
If a blood clot located in the left atrium or coronary arteries breaks off, the patient is at risk of: myocardial infarction, stroke if the blood clot enters the brain through the bloodstream, infarction of the intestines or kidneys if the arteries leading to them are blocked, as well as blood stagnation and gangrene with subsequent loss limbs if the blood clot gets into the large arteries of the arm or leg.
Causes and risk factors for the development of thrombophlebitis
Thrombophlebitis of the lower extremities rarely begins spontaneously. Most often, the disease becomes a complication of leg diseases. The development mechanism is associated with improper outflow of lymph and blood through the veins and vessels. After injury to the inner layer of the vein, bleeding begins. In response to this, a blood clot forms. It prevents blood loss, but over time it grows and completely blocks the lumen of the vessel, preventing blood from circulating.
The following factors precede this process:
- Damage to the vascular wall. This group includes mechanical injury to veins due to trauma and compression of the limbs. Venous walls are damaged when injections are performed incorrectly, frequent and long IVs, or operations.
- Deterioration of blood supply to certain areas of the body. The blood flows poorly due to wearing a cast for a long time, bed rest and physical inactivity. Less commonly, slowing of blood flow occurs as a result of heart failure.
- Improper flow of blood in the veins due to venous insufficiency. The complication develops against the background of pregnancy and diseases of the pelvic organs.
- Increased blood clotting. The viscosity and homogeneity of blood and plasma change with long-term use of hormonal drugs, discrepancies in the levels of estrogen and progesterone, and infections.
Other causes of thrombophlebitis may be:
- obesity;
- allergic reactions and sensitization;
- a history of venous thromboembolic complications (VTEC);
- taking a number of medications (diazepam, amiodarone, vancomycin, chemotherapy drugs, heroin addiction).
Acute thrombophlebitis often develops against the background of some autoimmune diseases, such as systemic lupus erythematosus, vasculitis, Behcet's and Buerger's diseases. In particular, in Behçet’s disease, TPV is detected in 53.3%, and DVT in 29.8% of patients i Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23. .
The risk group includes:
- Patients with heart disease - chronic heart failure, ischemic stroke. Limbs swell, motor activity decreases, and after a stroke there may be paralysis, which impedes the flow of blood through the veins.
- Patients with concomitant phlebological diseases - varicose veins, venous thrombosis. The speed of blood movement in the veins decreases, the blood stagnates, forming a blood clot.
- Bedridden patients, people with complex fractures. Their mobility is impaired and the likelihood of blood clot formation increases.
- People with a hereditary predisposition. Hemostasis disorders are transmitted genetically. The likelihood of the disease is increased if blood flow pathologies are detected in first-degree relatives.
Main causes
There are three main factors for thrombus formation.
- Damage to the vessel wall
(as a result of injury, surgery and poor nutrition (cholesterol plaques form), infection, heavy lifting, childbirth, etc.). - Blood clotting disorder
(tendency to increased clotting). Changes in blood clotting may occur due to metabolic disorders or hormonal imbalances. - Stagnation of blood
. It occurs when a person remains motionless for a long time in one position (for example, in front of a computer, in an airplane seat, or chained to a bed).
The risk group also includes people with varicose veins, those who are overweight, bad habits, leading a passive lifestyle, as well as people over 60 years of age.
Symptoms
Signs of thrombophlebitis appear immediately. The disease can be suspected based on the following clinical picture:
- the limb swells;
- the skin over the inflamed vein turns red, and the vessel itself darkens and is clearly visible under the skin;
- a compaction is felt to the touch along the course of the vessel;
- there is a feeling of heaviness in the legs and bloating of the veins;
- in a supine position, the patient cannot lift his leg and rotate his foot;
- The leg is cold to the touch.
At the initial stage, the symptoms are local, that is, the general condition does not change. As the disease progresses, mobility becomes impaired. The patient notes weakness in the legs and cannot stand for a long time. When bending the foot, he feels tension in the lower leg and thigh. Temperatures range from 37°C to 39°C.
Distinctive signs of thrombophlebitis of the lower leg are that the calf muscle turns blue and the veins on it swell. The pain is so severe that the patient cannot step on his foot.
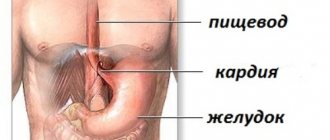
Thrombosis of the iliofemoral vein is manifested by pain in the lumbosacral spine, pain in the groin and the lower third of the abdomen on one side.
Femoral vein thrombosis is characterized by swelling of the veins in the upper thigh and discomfort in the groin area.
Diagnosis of thrombophlebitis
Diagnosis of the condition of the lower extremities includes:
- Vascular ultrasound in Doppler mode
. The blood flow of the superficial and deep veins is analyzed. Areas of narrowing of the vascular lumen and slowing down of blood flow are identified. - CT venography
. The transition of the femoral vein to the iliac vein is poorly visualized on ultrasound, so computed tomography shows a splash of blood after slow passage through a certain area. It is carried out with contrast enhancement, that is, a dye is injected into the vein. - D-dimer assay
. When a blood clot forms, the amount of fibrin breakdown products in the blood increases. The analysis is performed after an ultrasound. - Blood analysis
. The diagnosis is confirmed by high coagulogram (clotting test) values. The presence of C-reactive protein indicates inflammation. Leukocytes also grow, ESR increases, and the number of rods in the blood increases.
Treatment of thrombophlebitis
Therapeutic actions are aimed at suppressing inflammation, resolving blood clots and thinning the blood.
Drug treatment
venous thrombophlebitis involves taking:
- anticoagulants to thin and prevent blood clotting, in the acute phase are prescribed by injection;
- antibiotics for the infectious nature of the disease;
- angioprotectors to increase the tone of the veins, reduce venous stagnation;
- disaggregants for breaking down cells that form a blood clot;
- phlebotonics to strengthen and increase the elasticity of the walls of blood vessels;
- non-steroidal analgesics to relieve acute pain.
Compression therapy
using bandages, elastic stockings or class 2 sleeves accelerates blood flow in the superficial and deep veins, thereby preventing the growth of a blood clot. In addition, compression has an analgesic effect.
Physiotherapy
– an effective method of treating venous thrombophlebitis. After acute symptoms have been relieved, a course of magnetic therapy, infrared radiation, ultraviolet radiation, or darsonvalization of your choice is prescribed. The procedures reduce inflammation, increase blood circulation, and accelerate the regeneration of the internal walls of veins.
Surgical intervention
is prescribed if the blood clot grows and the threat of blocking the lumen of the vessel increases. There are several types of operations for thrombophlebitis:
- crossectomy – access to the saphenous vein through the groin and an incision in the thigh;
- thrombectomy – access to the thrombus through one incision;
- invagination stripping - with the help of a probe, the vein is everted, the blood clot is removed;
- stenting – the vein is expanded mechanically by installing a special balloon.
How to treat thrombosis
It is worth understanding that the treatment of thrombosis requires complex measures. Modern medical technologies make it possible to dissolve a blood clot by injecting special medications directly into the vessel. This method is used when there is a direct threat to life, since the injected drug permanently reduces blood clotting, which becomes dangerous with any injury.
There are also more conservative methods:
- Wearing compression stockings.
- Installation of vena cava filters that will catch blood clots.
- Prescribing medications based on acetylsalicylic acid (they normalize blood clotting).
REFERENCE!
The duration of treatment is determined only by the doctor.
Exercise therapy may be prescribed as an additional therapy. Doctors can recommend safe folk remedies for resolving blood clots:
- turmeric (promotes the resorption of blood clots);
- garlic (sulfur in its composition also fights clots);
- hot, red pepper or chili;
- flax seeds - contains a lot of Omega-3, which improves blood circulation;
- peppermint infusion.
Recommendations and contraindications for thrombophlebitis
The doctor advises you to follow a diet and wear low-heeled shoes with a comfortable last.
Forbidden:
- wear stilettos and heels higher than 3 cm;
- massage limbs;
- go to the gym and lift weights;
- remove leg hair with wax or epilator;
- go to the bathhouse and sunbathe;
- wear socks, stockings, and knee socks with a thick elastic band.
It is necessary to exclude the use of hormonal drugs and choose a different method of contraception.
Sources
- Bogachev V.Yu. Thrombophlebitis (thrombosis of superficial veins): modern standards of diagnosis and treatment / V.Yu. Bogachev [et al.] // Outpatient surgery. — 2021. — No. 3-4 (63-64). — P. 16-23.
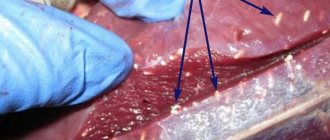
- Kuzmichev D.E. Pathomorphological findings. Thrombophlebitis / D.E. Kuzmichev [et al.] // Health care of Ugra: experience and innovations. - 2020. - No. 1. - P. 53-56.
- Marushchak E.A. Modern methods of ultrasound diagnosis of venous thrombosis of the inferior vena cava system / E.A. Marushchak, A.R. Zubarev // Outpatient surgery. Stationary replacement technologies. - 2014. - No. 3-4 (55-56). — P. 38-47.