Published: 08/13/2021 10:52:00 Updated: 08/13/2021
Hypoglycemia refers to a decrease in blood glucose levels to critical values. This is a dangerous condition that leads to disruption of the brain’s internal organs, and in a severe stage – to irreparable consequences or death due to hypoglycemic coma.
The symptoms of this condition are varied and depend on the cause of the pathology and the characteristics of the individual patient. Timely diagnosis and control of sugar concentrations make it possible to prevent serious complications and maintain the usual way of life.
Causes of hypoglycemia
A decrease in blood sugar levels is not a disease, but a condition that occurs due to a number of disorders of carbohydrate metabolism in the body.
Glucose, as a source of energy, determines the functioning of internal organs and the condition of a person as a whole. The brain is especially sensitive to a drop in sugar concentration. It works more intensively than all other organs, consumes an increased amount of “fuel”, is not able to store it and therefore is completely dependent on the continuous supply of glucose through the bloodstream.
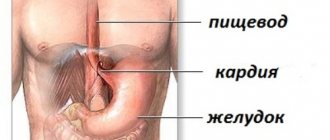
In the body of a healthy person, excess glucose from carbohydrates received from food is stored in the liver in the form of glycogen - a molecule consisting of many interconnected glucose molecules, which, if necessary, is broken down and absorbed into the blood. This ensures the smooth functioning of organs. Thus, any liver pathology can lead to hypoglycemia.
In addition, hormones significantly influence glucose metabolism:
- pancreas: insulin (responsible for the accumulation of glucose in the form of glycogen and reducing its level in the blood) and glucagon (stimulates the breakdown of glycogen, which causes an increase in sugar levels);
- adrenal glands: adrenaline, cortisol, growth hormone (increases sugar);
- thyroid gland: thyroxine and triiodothyronine (increase sugar).
Hypoglycemia is most often observed in diabetes mellitus.
On the one hand, the patient takes glucose-lowering medications. On the other hand, glucose from the liver enters the blood slowly. This leads to the fact that at some point the sugar concentration may drop to critically low values. This condition also occurs as a result of diseases of the gastrointestinal tract with impaired absorption of glucose, renal failure (increased excretion of sugar in the urine), cancer of the pancreas and some congenital pathologies.
Hypoglycemia resulting from disease is called pathological. In contrast, physiological hypoglycemia develops in healthy people during fasting, dehydration, emotional stress or excessive physical activity, taking certain drugs and alcohol.
In women, hypoglycemia is sometimes observed during pregnancy due to the fact that part of the mother's glucose is spent on fetal development. Hypoglycemia in children develops in the first hours or days after birth and can be temporary or permanent. Risk factors include prematurity, maternal diabetes, birth asphyxia, and congenital pancreatic anomalies.
Possible complications
The development of hypoglycemic coma can lead to severe dysmetabolic disorders that can damage most organs and systems. With the development of hypoglycemic coma, the removal of acetone from the body is impaired. The accumulation of acetone in the blood leads to intoxication of the body. The most serious complications are associated with inhibition of the vasomotor and respiratory centers of the medulla oblongata. With the development of deep coma, death is possible due to cardiovascular and respiratory failure.
Symptoms and types of hypoglycemia
Hypoglycemia is characterized by various symptoms, the nature and severity of which depend on the individual patient and the cause of the pathology.
The main signs of this condition include obsessive hunger, increased sweating, nausea and vomiting, weakness, tremors in the limbs, rapid heartbeat, decreased concentration, drowsiness, visual disturbances (blurred vision, double vision and “gnats” in the eyes), panic and anxiety, paleness of the face.
There are three types of hypoglycemia based on severity:
- Mild (a person is able to independently help himself by consuming sweet drinks and sugar-containing foods).
- Moderate severity (the person remains conscious, but needs the help of third parties to normalize blood sugar levels).
- Severe (a hypoglycemic coma occurs, the person is unconscious and needs urgent hospitalization).
Contraindications
There are many contraindications to the use of ICT. Therefore, before therapy, the patient undergoes an examination. Limitations for introducing it into an insulin coma may include:
- Active phase of tuberculosis
- Infectious diseases
- Liver pathologies
- Severe kidney disease
- Diabetes
- Stomach ulcer
- Heart defects
- Oncology
These are absolute contraindications. There are also relative ones - a mild form of tuberculosis, endocrine and vascular diseases, cholecystitis, gastritis and emphysema. If available, ICT can hypothetically be used. This is decided by the doctor in each specific case.
Diagnosis of hypoglycemia
The signs of this condition are quite characteristic, and the primary diagnosis is most likely made after a conversation with the patient and his examination.
The only difficulty is finding out the true cause of this pathology. Therefore, a wide range of laboratory and instrumental examination methods are used for diagnosis. First of all, if hypoglycemia is suspected, a blood test is performed to check the sugar level, which in this condition drops below 3.5 mmol/l. This test may produce biased results because many factors, including time of day, affect sugar concentrations.
The determination of glycosylated hemoglobin (HBA1c) is of great diagnostic importance. This is a stable combination of hemoglobin A with glucose in red blood cells: the more glucose in the blood, the higher the level of HBA1c. Throughout the life of a red blood cell (120 days), this compound continues to circulate in the blood, and determining the concentration of HBA1c allows us to reveal the true concentration of glucose over the last two to three months.
In order to establish the cause of hypoglycemia, a blood test is performed for hormones (in particular, the thyroid gland and adrenal glands), the presence of excess alcohol and medications, a urine test, a biopsy of the liver and pancreas to confirm insufficient production of enzymes, ultrasound, MRI and CT scan of internal organs.
Hyperosmolar non-acidotic
Non-ketoacidotic hyperosmolar coma also develops due to acute decompensation of diabetes. It is based on a sharp decrease in insulin levels and loss of fluid from the body. In this case, there is no excessive formation of ketone bodies and acidosis [7].
| Laboratory indicators | Values |
| Blood plasma glucose | >30 mmol/l |
| Blood osmolarity | 400-500 mOsm/l [4] |
In a general blood test, an increase in hemoglobin and hematocrit levels is noted due to a decrease in plasma volume. There is no acetone in the urine [3].
Treatment of hypoglycemia
First of all, when signs of this condition appear, it is necessary to provide the body with glucose.
Conscious patients should be given quickly digestible carbohydrates: sweet drinks (fruit juice, compote, tea, sweetened water) and sweets (sweets, marmalade, honey, pure sugar). In cases of moderate severity, a glucose/dextrose solution is administered intravenously and/or subcutaneously, glucagon is administered subcutaneously or intramuscularly.
For hypoglycemic coma, droppers with saline, insulin and electrolytes are used.
First of all, medical care for hypoglycemia is aimed at treating the underlying disease that caused the pathology.
Where does lactic acidosis come from?
Lactate is a natural by-product of lactic acid from the breakdown of glucose and amino acids. In a healthy body, it is produced in minimal doses and breaks down into water, carbon dioxide or glucose. Decomposition products are excreted through the kidneys. When their accumulation occurs (lactic acidosis), the acidity of arterial blood increases sharply, the enrichment of cells with oxygen decreases, and the effect of insulin decreases. As a result, hyperglycemic coma occurs.
Based on the nature of the clinical picture and the degree of progression, early, middle and late stages are distinguished. The patient's condition changes in just a few hours, the symptoms change sharply from general malaise to coma. The classification based on etiopathogenetic mechanisms, developed in 1976 by Cohen and Woods, distinguishes several types of lactic acidosis:
- Acquired - type A, manifests itself after 35 years, can develop even in the absence of diabetes. Tissue hypoxia (oxygen starvation of cells) inhibits the functions of the central nervous system and accelerates the respiratory and pulse rates.
- Congenital - type B, occurs due to the underlying disease (diabetes mellitus), toxin breakdown products, and congenital problems with metabolism. Causes kidney or liver failure.
In the international statistical classification (ICD-10), lactic acidosis refers to disorders of water-salt and acid-base balance.
Prevention of hypoglycemia
Simple and effective recommendations allow the patient to control their condition and live a full life:
- strictly adhere to the diet (healthy diet without long breaks between meals), as well as sleep, exercise, and taking prescribed hypoglycemic and other medications;
- Constantly monitor sugar levels (measurement with a glucometer at home, repeated tests for glycosylated hemoglobin every 3 months);
- learn to clearly identify signs of low glucose levels, always carry sweet bars with you and notify loved ones about first aid measures in case of an attack.
Author:
Pugonina Tatyana Alekseevna, Therapist
First aid during an attack
Providing first aid to a patient with a diabetic coma is carried out in the first hours after the onset of an attack. The following tactics are used:
- Call an ambulance.
- Monitoring vital human functions (respiration, blood pressure, pulse).
- In case of cessation of breathing or cardiac arrest, artificial respiration and indirect massage of the heart muscle are performed.
- The patient must be placed on his side, this will help avoid tongue retraction.
- The patient should be helped to administer insulin.
- After the ambulance arrives, inform the doctors about the time of the crisis and the characteristics of the patient’s condition.
More information about emergency care for the development of diabetic coma can be found here.
Proper first aid is just as important as hospital treatment
Important! The patient’s future health and life will depend on how competently the pre-medical care is provided.
Anti-infective regime
During ICT, the patient's immunity decreases. He becomes vulnerable to infectious diseases. To prevent their development, the following measures are taken:
- The patient is not allowed to cool down, especially when he is sweating heavily. You should dry him and change him into dry clothes. Also, orderlies periodically change bed linen;
- All windows in the room are closed to prevent drafts. The doors are not kept open;
- The patient is examined daily for inflammation. Even an ordinary boil can cause sepsis;
- Body temperature is measured twice a day. If it has increased so much that an infection can be suspected, the ICT course is interrupted.
If necessary, the patient is prescribed additional medications - antibiotics, anti-inflammatory drugs, etc.
Levels of switching off consciousness
One of the most important aspects of ICT is clear monitoring of the patient’s levels of unconsciousness. There are 4 of them in total:
- Doubtfulness - the patient sleeps, but quickly awakens when exposed to external influences;
- Stupefaction - the patient is able to answer questions, but slowly and in monosyllables;
- Stupor - a person fixes his gaze on the doctor or orderly, but can no longer answer questions. His attempts to follow instructions become weak and ineffective;
- Coma - the patient completely stops responding to external stimulants.
Staff must be able to differentiate between these levels in order to administer sugar or medications in a timely manner.