Birth injuries are not uncommon. Although the overall quality of medical services has been improving in recent years thanks to modern equipment, 5% of all newborns fall into this category. The main thing in the case of birth injury is timely diagnosis and treatment.
Cephalohematoma in newborns on the head - symptoms, treatment
Cephalohematoma is a birth injury characterized by the formation of a hematoma.
Pathology is diagnosed in 3% of children, regardless of gender. Cephalohematoma in newborns on the head can be accompanied by various kinds of complications: deformation of the skull bones, suppuration, anemia and jaundice. The formations come in different sizes and depend primarily on the volume of accumulated blood. Due to the failure of the hemostatic system in the baby's body, blood can accumulate for several days after birth, contributing to an increase in the size of the hematoma. Causes of cephalohematoma during childbirth:
- large fruit;
- rapid labor;
- malposition;
- premature or prolonged labor;
- umbilical cord entanglement;
- discrepancy between the sizes of the mother's pelvis and the fetal head;
- pathologies of intrauterine development;
- use of forceps during childbirth.
Prevention
Periosteal hemorrhage can be avoided if the following conditions are met:
- the expectant mother should lead a healthy lifestyle and not take medications without consulting a doctor;
- The doctor and midwife must conduct the birth carefully, choose the method of delivery correctly and quickly.
To prevent recurrent hemorrhage, mothers should not rock the baby until 6 months of age. You cannot refuse surgical treatment of a hematoma. If your doctor recommends a cesarean section, it is best to choose this method of delivery. If these recommendations are followed, the child will quickly recover from the injury.
A cephalohematoma on the head of a newborn noticed in time, the treatment of which is quite easy, does not pose a threat to the child’s life.
Classification of cephalohematoma
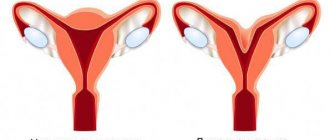
As noted above, external cephalohematoma is a hemorrhage between the periosteum and the surface of the skull bones, which disappears by the end of the second month of the baby’s life.
Depending on the location, hemorrhage can be frontal, occipital, parietal and temporal. Based on the severity, cephalohematoma is divided into grade I (hematoma volume 3-4 cm), II (4-9 cm) and III (hemorrhage more than 9 cm). The consequences of a birth cephalohematoma in the future depend on the size of the formation and the general condition of the newborn. Considering the location of the hemorrhage, cephalohematoma can be left-sided, right-sided or bilateral. In some cases, the pathology is accompanied by concomitant injuries in the form of a fracture (crack) of the skull bones.
Pathogenesis
Cephalohematoma is a consequence of soft tissue damage during childbirth . The essence of the mechanism of this injury is that as the child’s head passes through the birth canal, the bones of his skull are compressed, the soft tissues are displaced, and the vessels of the subosteum are ruptured. When the tendon helmet moves along with the skin, tension occurs on the fibrous fibers that connect it to the periosteum. Strong mechanical stress provokes damage to the small vessels of the periosteum, and blood from them pours into the subperiosteal space. As a result, a cephalohematoma is formed.
Until recently, experts believed that the main cause of this condition in infants was pathological childbirth. However, medical statistics record an increase in the number of cases of this diagnosis in recent years, and this also occurs in children born in physiological labor. Therefore, the development of cephalohematoma is currently associated with various factors, in particular with the incorrect position and presentation of the fetus, its large size, and diabetic fetopathy. Also, this pathology can be associated with various complications during pregnancy , the application of obstetric forceps during childbirth and the use of vacuum extraction.
Signs of ossified cephalohematoma
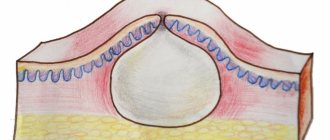
Cephalohematoma occurs within a few hours after the baby is born. Over the next 2-3 days, the formation increases in size, after which a period of regression begins. Complete resorption of the hematoma occurs by the end of 8 weeks.
Main symptoms:
- education has clear boundaries;
- on day 2-3, the growth of the hematoma stops;
- the color of the skin in the area of the cephalohematoma is unchanged;
- the hematoma is soft to the touch;
- the general condition of the baby is unchanged.
On our website Dobrobut.com you can make an appointment with a specialist and get an answer to any question. The doctor will talk about the main signs of ossified cephalohematoma and methods of treating the pathology.
Tests and diagnostics
In the process of establishing a diagnosis, differential diagnosis is carried out with a birth tumor, cerebral hernia, hemorrhage under the aponeurosis . If we are talking about an uncomplicated cephalohematoma, the doctor is primarily guided by the examination data. In this case, it is not difficult to establish a diagnosis if you examine the head and detect the characteristic signs of the disease.
The clinical picture of cephalohematoma is nonspecific; symptoms of damage to the nervous system are more pronounced.
In addition, during the diagnostic process, if necessary, the following methods are used:
- computed tomography – used if there is suspicion of damage to brain tissue;
- ultrasound examination - makes it possible to find out whether there is a fracture of the cranial bone, a cerebral hernia, and also determine the size of the tumor;
- Craniography in direct and lateral projections – allows to exclude bone damage;
- multislice CT;
- neurosonography – allows you to determine the presence of damage in the brain.
Treatment of cephalohematoma in a child
Hemorrhage is treated by a neonatologist or pediatric surgeon. For a small hematoma, there is no need for special treatment. The baby is prescribed calcium and vitamin K supplements for 5-7 days. The course of treatment for uncomplicated pathology is 7–10 days. Treatment of a cephalohematoma in a child that occurs with complications will require at least a month. A child with such a pathology must be registered with a surgeon and neurologist.
To speed up the healing of the formation, neonatologists advise using Troxerutin. The gel is applied to the hematoma area twice a day. The drug increases vascular tone and prevents further penetration of blood.
In case of extensive hemorrhage (more than 9 cm in volume), the doctor will prescribe surgery. Puncture of a cephalohematoma of the parietal bone is a procedure that is safe for the baby’s health and takes no more than 10 minutes. The child’s skin at the site of the hematoma is pierced with a special needle, the accumulated blood is sucked out, after which the puncture site is disinfected and a pressure bandage is applied. Surgical removal of cephalohematoma is indicated in the presence of purulent contents of the cavity, as well as in the III degree of development of the pathology.
Doctor's recommendations after puncture:
- parents need to strictly follow the specialist’s instructions;
- In no case should you self-medicate;
- protect the newborn’s head from damage;
- use a hat one size larger;
- carefully monitor the general condition of the baby.
Symptoms
Cephalohematoma in newborns becomes noticeable on the second or third day, when the birth tumor subsides.
Photo of cephalohematoma in newborns
From the first day, the size of the hemorrhage increases, since newborns lack blood clotting factors, therefore, it remains liquid for a long time, and damaged vessels are not thrombosed by blood clots. As pediatrician Komarovsky notes about cephalohematoma on the head in newborns, its size depends on how severe the bleeding .
The symptoms of cephalohematoma are especially pronounced on the second or third day after the baby is born. Its distinctive feature is precisely the gradual increase these days. The child's head becomes asymmetrical due to the appearance of a formation.
If you try this formation by touch, it will be elastic, and with slight pressure on it you can feel the liquid moving. The skin over it is unchanged, elastic.
There can be from 5 to 150 ml of blood under the periosteum. Accordingly, if the cephalohematoma is small, then it decreases approximately a week after its appearance, and no intervention is required.
If the cephalohematoma is isolated, the child’s health remains normal. If it is combined with another pathology, then the baby experiences neurological symptoms. In most cases, there is depression of the function of the central nervous system, which is manifested by a sluggish reaction to the action of pathogens and poor expression of reflexes.
In some cases, it is possible to manifest strong central nervous system excitation similar to a hydrocephalic or hypertensive complex of symptoms.
If the size of the formation is large or the child has impaired blood clotting, and the cephalohematoma does not shrink on its own, anemia , ossification , resorption hyperbilirubinemia , and infection of the hematoma are likely.
With large cephalohematomas, rapid hemolysis of red blood cells , as a result of which a yellowish tint of the skin and mucous membranes is observed in the first days of the baby’s life. In this case, jaundice persists for 10 days or more.
Sometimes, where the formation is localized, a fracture (crack) of the bone is noted.
What happens next to the cephalohematoma?
The cephalohematoma initially has an elastic consistency, sometimes fluctuates (that is, when pressing on the formation itself, you can feel movement, “ripple” of the liquid) and is limited by a cushion around its circumference.
If the amount of blood in the cephalohematoma is small, then from the 7-10th day the tumor begins to decrease in size and usually disappears in the 3-8th week, resolving on its own, without any intervention or treatment. If the hemorrhage is significant, then the resorption of the blood is delayed and may take months. In addition, with a very large cephalohematoma, the blood inside it can be absorbed into the surrounding tissue and saturate it. In this case, a certain amount of bilirubin (a product of the breakdown of hemoglobin in tissues) will enter the bloodstream and the child may develop jaundice, which will last longer than physiological (transient jaundice of newborns) and will not disappear by the 10th day of life. In these cases, the periosteum in the area of the cephalohematoma becomes denser, the hematoma ossifies, that is, it ossifies, followed by bone growth, which leads to deformation or asymmetry of the skull. Under the cephalohematoma, a bone fracture is sometimes found, through which communication with the epidural hematoma is possible.
Diagnosis of cephalohematoma is usually not difficult. Ultrasound examination can help to clarify the extent of cephalohematoma, as well as to exclude the presence of a bone defect and cerebral hernia.
List of sources
- Obstetrics. National leadership / Ed. E. K. Ailamazyan, V. I. Kulakov, V. E. Radzinsky, G. M. Savelyeva. - M.: GEOTAR-Media, 2007. - P. 1160-1161.
- Bardeeva K.A., Pisklakov A.V., Lukash A.A. A new look at the treatment of cephalohematomas in children // Modern problems of science and education. – 2015. – No. 5.;
- Ch. 6. Children's diseases // Directory of a paramedic / Professor L.A. Isaeva. - Moscow: “Medicine”, 1975. - P. 319. - 662 p. — 280,000 copies.
- Kerchelaeva S.B. Cephalohematoma as a result of complications of childbirth / Kerchelaeva S.B., Tyagunova A.V., Kuznetsova O.V. // Attending physician - 2015. - No. 10 - p. 88–92.
- Handbook of obstetrics, gynecology and perinatology / Ed. G. M. Savelyeva. - M.: MIA, 2006. - P. 344-348.
Forecast
As a rule, the prognosis for this disease is favorable.
Serious complications occur in a small number of children and are a consequence of displacement of brain structures, which are pressed by a hematoma and accumulation of blood.
Statistics show that in approximately 80% of cases, subperiosteal hematomas significantly decrease in the first week after their appearance, and completely resolve within 2-3 weeks. However, if this does not happen, then the cephalohematoma begins to ossify.
Research Institute of Psychotherapy and Clinical Psychology
The concept of injury (Greek: τραῦμα) is damage to living tissue with a violation of its protective mechanism. Damage occurs as a result of violence against the subject. Trauma can be both physical and mental. Both can combine signs of a violation of the physical nature, functional interaction of organs and a violation of the adequate state of the psyche. Physical treatment of injury eliminates the violation of the integrity of the physical nature, restores the functions of damaged organs and even the adequacy of the mental state of the victim of injury. However, the consequences of trauma continue to influence a person’s quality of life for a very long time due to the fact that trauma affects not only consciousness, but indirectly also its unconscious perception. It is capable of causing structural dissociation of personality [1], when a dissociated personality, without the help of a psychotherapist, is not able to integrate back into the general personality system. The main function of dissociated personalities, along with the central personality, is the adaptation of the individual to society and internal communication of the psyche.
The aftereffects of trauma are determined by the existence of memory and the possibility of its isolation from the central personality. This possibility of isolating memory is especially noticeable when studying the content of the memory of a person who has been subjected to acts of violence. At this time, a person may develop several structurally dissociated personalities in response to trauma. For example, during sexual violence, combined with a real threat to a person’s life, several structural dissociated personalities with different types of behavior may arise at once. One of the types is when a person, out of fear for his own life, completely submits to the will of the rapist and does not offer any resistance. If the object of violence is a girl and at the same time she receives sexual satisfaction, then manifestations of this type are accompanied by a very strong feeling of guilt, often ending in suicide. Another type of behavior is desperate resistance, inadequate to the degree of influence (violence). The third type of behavior is an indomitable unconscious desire to take revenge on all males, especially close people, such as a husband. In our practice, there is a case where a woman (M.), who was subjected to physical violence in the form of injuries, starting from the mother’s womb, for reasons unknown to her, did not have a personal life. M.'s father often quarreled with his mother, even to the point of assault, and once, when she was still in her mother's womb at the age of four months, her father, in his anger, threw a heavy bunch of keys towards her mother and hit her right in the navel area. During age regression, M. saw and felt that a blow from a bunch of keys hit her right in the face. Physical violence and psychological pressure were exerted on M. for a very long time in the postnatal period of life, right up to adulthood. At one of the age regression sessions, M. stated: “I have been haunted by revenge all my life.” To the presenter’s question: “Were you retaliated against or did you take revenge?” M. replied that she took revenge on both her first and second husbands (currently four unsuccessful marriages).
Another case of violence against a pregnant woman in her third month of pregnancy. She was raped by her own husband, who was drunk. The violence occurred even before the prenate’s central nervous system matured, let’s call it A. In adulthood, 28 years later. during the age regression session, A. clearly reproduced all the events of that period, in addition, another picture was revealed that in front of him was his brother, who died in the womb without being born. It should be noted that we conduct age regression sessions with subjects who are in a fully awake state with preserved critical perception [2] [3]. Then, whenever possible, the facts reproduced at the session are verified by interviewing witnesses (in this case, parents) or analyzed for a causal relationship with the existing pathology that manifested itself in the postnatal period. As an adult, A. was bothered by severe back pain that was not relieved by any medical procedures. They released him only after working through the perinatal situation with rape at an age regression session. In addition, the situation with the mother’s rape caused complications in the birth process due to the strong resistance of the prenate. He did not want to be born and resisted it in every way available to him.
Our other subject E., during age regression, described in detail the Kristeller method, which she had no idea about before. While doctors were using this method, she felt strong pressure on the lumbar spine. As an adult, she was diagnosed with spondylosis of the spinous processes of the lower thoracic and lumbar vertebrae.
There are also memories that can be characterized as psychological trauma. Reaction to the current situation, for example: “My body is weak, powerless, my shoulders are sagging, my mother is very tired, and this fatigue was transferred to my body.” There are also memories such as: “My head fell back, my body convulsively stretched out in a column and this state lasts for quite a long time (moment of a strong quarrel between parents without assault).” There are also memories like: “I’m screaming very loudly inside”; “I’m crying from powerlessness”; “I probably have tears of joy,” “I have terrible fear. Everything shrank inside me... I looked at my dad with my face to my tummy and felt like I had no protection. Even my mother can’t protect me”; “I turned around in the womb facing my back, I want to warm up, there is much less light there. Prerequisites for falling asleep arise”; “I leaned my shoulder against my mother’s tummy, and I was facing her side. I'm really scared"; “My head is up, there is a feeling of being pressed down, they want to push me out” (provoked by the parents’ thoughts about whether or not to leave the child).
And here’s another story, when a mother is told at a doctor’s appointment that she may have a miscarriage: “It’s a strange feeling... mom smokes. In general, as far as I know, she is not a smoker... she smokes. Some worries about her father... she's waiting for him (E. had a severe coughing attack during this period of intrauterine life...) ... she's waiting from work in the evening... I've never seen her smoking ... It's not so much smoking that bothers me, but her brightness expressed excitement... There is no connection with my father, and he did not spend the night at home... I am 4 weeks old... I am facing the back . ..I’m 9 weeks old...my mother drinks wine.. it’s very difficult to explain the physical discomfort, it feels as if a crust of bread was stuck to my head and where my stomach is (I don’t know if I already have a stomach), it’s uncomfortable... seething and heaviness. I don’t know if my feeling of pronounced warmth in my legs is connected with this... and there is a passage under them and it’s as if someone is pulling me by my legs into this passage... Wow! Straight... you can fly off, but there is no feeling of danger.”
All of the above cases, which can be characterized as psychological trauma, as a rule, had negative consequences in adult life, and with some work through prenatal moments together with a psychologist or psychotherapist, the negative consequences were stopped or weakened and they could be worked with using other traditional therapeutic methods.
The question arises: What is elaboration and how can one process past events, which can sometimes occur during the perinatal period of human development before the formation of a fully mature brain. According to the modern scientific paradigm, a full-fledged human psyche is not possible without a normally functioning integral nervous system and its attribute of higher nervous activity (HNA). The presence (storage, retrieval, reproduction) of dynamic memory is also impossible when considering it as some kind of frozen, encoded record in one of the elements of the central nervous system. The practice of psychoanalysis (decoding dreams, identifying post- and perinatal imprints), data from transpersonal psychology[4][5] and age regression[6][7], especially on revealing the memory of the perinatal period, completely contradict the currently existing paradigm. In order to reconcile the obtained facts in the field of transpersonal and perinatal psychology with the idea of the obligatory necessity of the central nervous system and internal nervous system for the functioning of memory, apparently, some assumption should be made. The central nervous system and the internal nervous system are more necessary for interaction with memory (extraction and reproduction - the unfolding of real and virtual [8] “plots” of memory in time) than for its storage, that is, they are necessary for feedback of memory plots with human consciousness when the central nervous system and GNI have already formed and matured.
At the moment, the following types of memory are known: explicit, implicit, figurative, auditory, musical, associative, memory for pre- and postnatal stories, which are in the competence of consciousness, preconscious, unconscious and collective unconscious parts of the psyche. There are other classifications of memory. However, in order to make the next important assumption, the above classification is sufficient. The common thread running through all of these types of memory is the idea of their dynamism. In other words, the activation of memory requires a certain stimulus, and its deployment in time in the future is relatively independent of the stimulus that caused it and, on the contrary, acquires “power” over the stimulus [8]. Perhaps this is the mechanism for the emergence of neurosis and the neurosis of a similar state. That is, memory can be considered as a certain process of interaction of an information carrier (information without a carrier does not exist) with space-time. In this case, the “repository” of prenatal memory, for example, may be not only, and perhaps not so much the fully formed brain of the prenate, but certain specific informational morphofunctional fields like the fields postulated by Rupert Sheldrake [9]. As a kind of field structure, one can also imagine virtual reality, postulated in the works of prof. N. Nosova and Ph.D. Yu. Yatsenko[8][10]. The theory of these fields has not yet been clearly formulated. We assume that morphofunctional fields and virtual reality, multimodal in nature, are not tied to any specific time. They interact with incoming stimuli and can respond to them by deploying specific information depending on the properties of the stimulus itself in virtual, figurative-fantasy space and This is where their attachment to time and place occurs. Perhaps fantastic dream plots are formed in a similar way, but the nature of the stimulus that brought them to life is persona non grata for conscious perception, and therefore, it is difficult for these figurative fantasy plots to find “their” information carrier in the “material” world and they are quickly forgotten . That is, when it comes to the unfolding in time of any of the figurative plots of “memory” in response to a stimulus, the meaning is related to the stimulus of our conscious and unconscious perceptions, our criticism, which are linked to the time and place of action, that is, finding a carrier in real material world. Each time a stimulus arises, most likely either in the central personality or in one of its dissociations and, accordingly, the stimuli may differ from each other.
The formation in the human psyche of an imprint, a structural pathological dissociative personality, provides a hypothetical opportunity for extrapersonal stimuli, for example from virtual reality or the reality of morphofunctional fields, to interfere with the work of a person’s internal nervous system and become the cause of neurosis and neurosis of similar states due to the fact that for it there is no resistance to the transfer of information from the virtual reality into the real one, since there is no time reference in virtual reality and morphofunctional fields. The stimuli they generate bring to life virtual negative stories[10], which can traumatize the psyche and through it the soma. We have encountered this mechanism for the emergence of psychosomatic pathology in an adult many times in our age regression sessions. For example, one of our subjects E. (a 26-year-old woman with a great sense of guilt) contacted us about the depression that had overcome her. Depression, in her opinion, is caused by pregnancy from a married man. She is afraid and does not want to have an abortion, especially since she sincerely loves the young man. The above circumstances brought her to the point of obsessive thoughts of suicide and deep depression. During an age regression session, a picture of Hell appeared in front of her, more typical of the Muslim religion, although she was a Christian by religion. When asked why they were showing this to her, the virtual voice answered that they were showing it so that she would know! After an age regression session held three times, the depression was relieved, and E. no longer had thoughts of suicide. At the moment, she is a happily married mother of two beautiful healthy children with her beloved husband.
A favorable property for the process of psychotherapy with our new theoretical and practical approach to working with the patient is the possibility of creating in him any new figurative and fantasy plot, with the help of which any painful stimulus emanating from the central nervous system or virtual field reality can be stopped. The essence of our approach is that we stimulate figurative imagination in a patient who is in a fully awake state with preserved criticism. The figurative imagination begins with neutral images that do not traumatize the psyche, then the patient’s perception, often in a playful form, is gradually reoriented to the images of his “personal” virtual reality. From the height of the current life experience, it is easy for a patient who is in a waking state to move on to a conscious dialogue with a traumatic situation and stop it with the help of tips and certain techniques of a psychotherapist. That is, any negative figurative fantasy plot, when conducting a dialogue with it, can be completely reformatted with the transformation of a negative moment into a positive one. We use this very often in our work if our patient has an imprint that interferes with a normal life in adulthood and this imprint is caused by some serious quarrel between parents or punishment of our client in the early postnatal period of his development. For example, our client A. constantly had obstacles to the implementation of any personal or work plans. During age regression, A. developed a plot of cruel punishment by his father for a trivial reason. We worked with guilt and forgave our father. We went back a little in time and “cancelled” the punishment. The results exceeded all expectations. A., who for a long time did not dare to get married, is now happily married, his work is going as well as possible. Unexpectedly for both of us, he even ended up in the plot of the “future”, where he was hired to work in a very prestigious office. That is, the method of predicting the future has been legalized using our age regression methodology in a conscious state. In other words, the method greatly expands the boundaries of accessibility to work with various types of psychosomatics and relationship psychology.
Working in this way, we have demonstrated in hundreds of our patients the high productivity of our approach for the treatment of neuroses and neurosis-like conditions. In addition, it turned out that plots of the collective unconscious that sometimes arise suddenly during psychotherapeutic work, as in the above example with E., have a high healing potential when working with them. For example, our client G. At the age of 35 she was seriously ill, as they say, on the verge of life and death. She, as a sincere believer, turned in prayer to God with a request to give her the opportunity to raise her children to independent age. She recovered, the children grew up and became independent and successful. Trouble came unexpectedly; a pathology of the internal carotid artery was diagnosed, requiring mandatory surgical intervention. The operation was successful, but the psychological state was extremely difficult. “God kept his promise” and it’s time to leave this life. Repeated elaboration of the plot of the appeal to God restored G.’s normal psychological state. And she is currently nursing her grandchildren with care and love. After these cases, we ourselves began to provoke, if necessary, the appearance of figurative and fantasy plots of the collective unconscious and the result exceeded all our expectations. I will give just one example with a patient from the intensive care ward Zh., who indomitably sought to take his own life. He constantly pulled out any catheters and turned off the intensive care devices. He was admitted to the hospital due to his participation in an accident. While overtaking the vehicle in front, he drove into the oncoming lane and, as a result of a collision with an oncoming car, his pregnant fiancee died. He himself ended up in the intensive care ward with moderate injuries. While working with J., we evoked the image of the collective unconscious in the form of a space where the dead live. He had a dialogue meeting with his fiancee, who asked him to help her single mother, who was left alone. From that moment on, Zh. quickly recovered and no longer had suicidal thoughts.
Thus, based on all of the above and the above references to the scientific literature, a new hypothesis can be formulated. Primary memory is the reality perceived by our anatomical senses, virtual reality, morphofunctional fields and, perhaps, not yet explored “impersonal” realities, including the material of conscious experience, unconscious experience and the experience of the collective unconscious, which has always existed and continues to exist in the present time in the form of figurative and fantasy “puzzle plots”. Any figurative fantasy plots can be unfolded in time in the form of a certain process and perceived by the consciousness of a person with a fully formed central nervous system with a normally functioning internal nervous system. To reproduce figurative fantasy plots (adequately connect puzzle plots), an adequate stimulus is required from any dissociated personality that is part of the general system of the main personality or isolated from it. In turn, any figurative fantasy plots can generate stimuli capable of causing pathological personal dissociation of the general personality system, causing neurosis or a similar state of neurosis in a person. Any figurative fantasy plots are labile and amenable to reformatting. Thanks to the ability to interact with figurative fantasy plots while awake, the patient gains the opportunity to influence any unwanted imprint or lead a pathologically dissociated personality to integration into the general personality system. Based on the factual material of our research on age regression in a conscious state on more than 600 subjects and analysis of scientific literature, the following can be made:
Conclusions:
- A new effective psychotherapeutic method of regression therapy has been created, carried out with a client who is awake and has a critical assessment of the surrounding reality.
- A new addition to the concept of memory has been formulated, which significantly facilitates the work of a psychotherapist and reveals the mechanism for relieving neuroses and neurosis of similar conditions using the method of regression therapy.
- The boundaries of working with negative imprints have been expanded in order to effectively stop them, up to the use of virtual reality spaces, morphofunctional fields, and the reality of the collective unconscious.
- A start has been made for the inclusion in the subject of scientific research of facts that were traditionally “taboo” for science: the study of timeless figurative and fantasy “timeless” spaces of the collective unconscious and religious ideas.
- A new hypothesis has been formulated about figurative-fantasy plots-puzzles of memory and possible targeted work with them in many areas of psychotherapy.
Bibliography
- Van der Hart O., Ellert RS Nijenhuis, Kathy Steele, The Haunted Self. Structural Dissociation and the Treatment of Chronic Traumatization, 2006
- Tashaev Sh. S., Age regression as a tool for correcting prenatal negative imprints, 2008
- Tashaev Sh. S., Perinatal memory and imprinting. Int. Journal of ISPPM, 2011
- Grof S., Beyond the Brain, 1985.
- Avtonomova N. S., New philosophical encyclopedia. In 4 vols. M.: Thought. Edited by V. S. Stepin. 2001.
- Chamberlain D, Your Child's Intelligent Brain, 1998.
- Tashaev Sh. S., “Study of the unconscious, pre- and postnatal individual perception by means of the age regression model.” Int. Journal of ISPPM, 2007.
- Nosov N., Virtual psychology, 2000.
- Sheldrake, R., A New Science of Life. The Hypothesis of Formative Causation, 2005.
- Yatsenko Yu. T. Physiological, biochemical and psychopathological components of alcohol withdrawal syndrome in various treatment methods. Author's abstract. dis. for the job application scientist step. PhD: Specialist 03.00.13: Special. 14.00.45 / [North. state honey. University, Institute of advanced training Feder. ex. med.-biol. and extreme. problem under the Ministry of Health of the Russian Federation]. - Arkhangelsk: B.I.: 2001.
Risk factors
Signs of cephalohematoma occur under the influence of negative factors, which include:
- rapid labor activity;
- a narrow pelvis in a woman in labor;
- large fruit size;
- incorrect position of the child in the womb;
- intrauterine development disorders;
- long period of bearing a child (over 42 weeks);
- the pregnant woman is over 40 years old;
- oxygen deficiency;
- accumulation of mucus in the mouth.